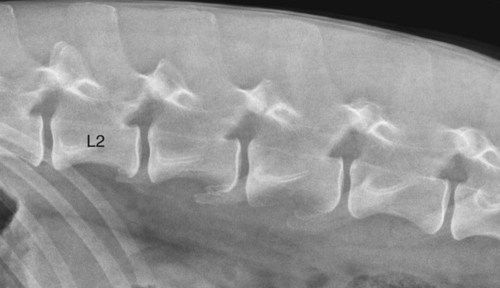
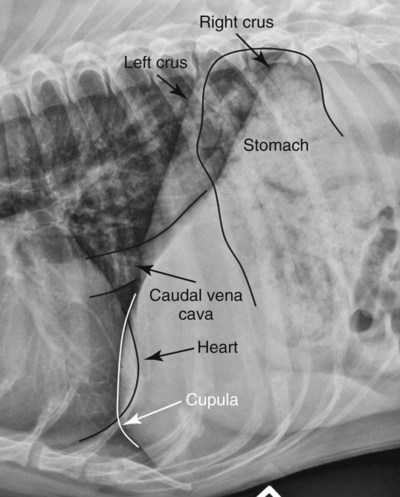
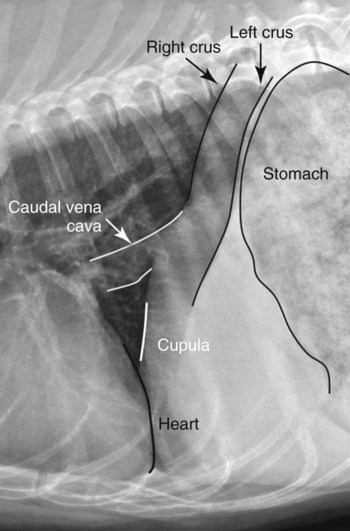
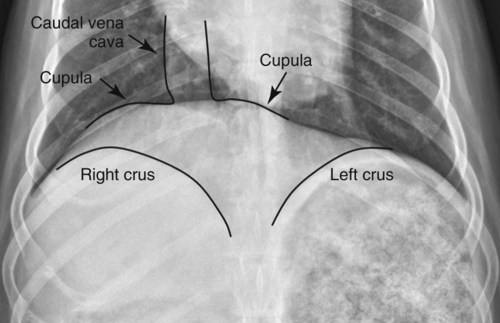
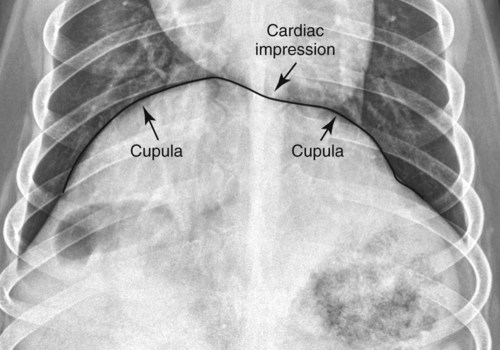
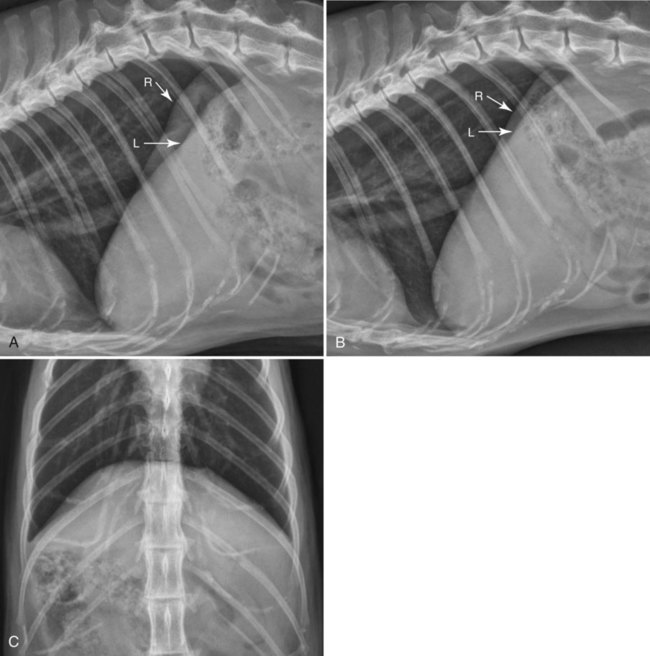
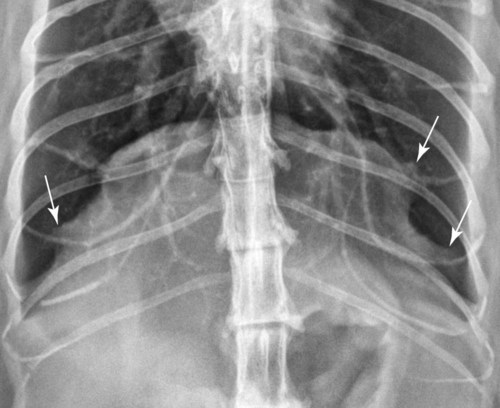
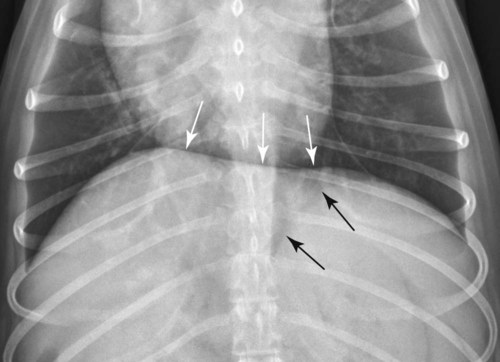
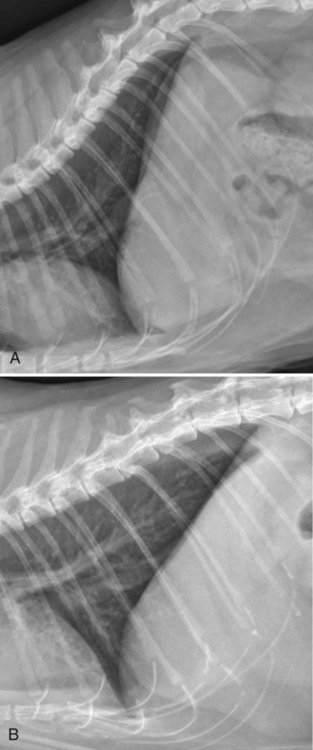
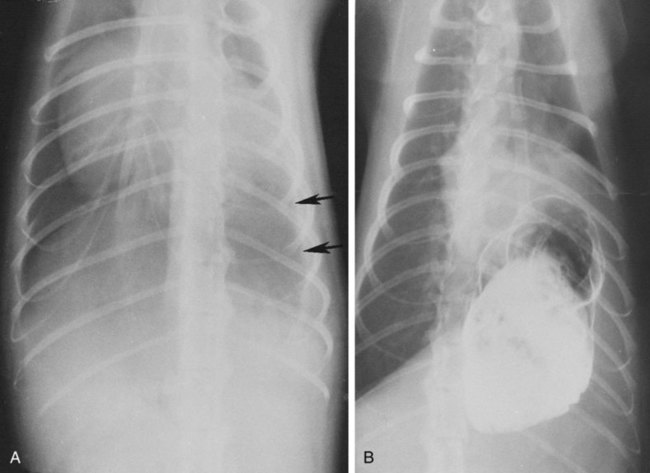
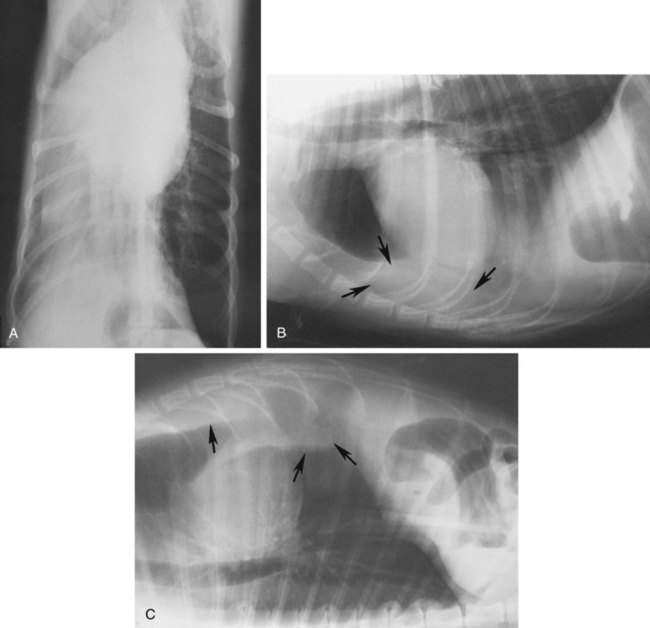
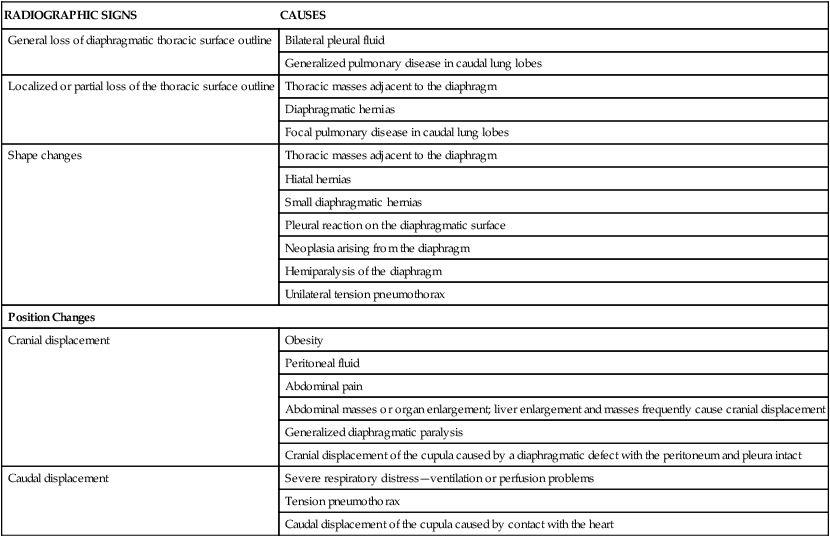
Movement of the diaphragm provides approximately 75% of the change in intrathoracic volume during quiet respiration.1 The diaphragm also acts as a mechanical partition between the thorax and the abdomen. Lymph vessels from the abdomen penetrate the diaphragm and drain into the thoracic lymph nodes and vessels. Thus inflammatory or neoplastic abdominal disease may spread to the mediastinum and pleural space. Lymph flow is unidirectional with the final destination being the thoracic trunks.2 The diaphragm consists of a tendinous center and three thin peripheral muscles: the pars lumbalis, the pars costalis, and the pars sternalis. The pars lumbalis consists of the right and left crura, which attach to the cranial ventral border of L4 and the body of L3. The attachment area on these vertebrae occasionally has a concave indistinct ventral margin that may be mistaken for bone lysis (Fig. 29-1). The pars costalis attaches in an oblique direction to the thirteenth through eighth ribs, and the pars sternalis attaches to the xiphoid cartilage.3 The diaphragm is convex and extends into the thorax from its attachments, creating the phrenicocostalis and phrenicolumbalis recesses. Diaphragmatic structures that may be visualized distinctly radiographically are the right and left crura, the intercrural cleft, and the cupula (body) (Figs. 29-2 to 29-5). Associated structures that may also be seen are the caudal vena cava and the caudal ventral mediastinum. On the lateral view, the right crus of the diaphragm blends with the caudal vena caval border, and the gastric fundus may be seen adjacent to the abdominal surface of the left crus. The intercrural cleft is a shorter, convex, opaque line caudal and ventral to the crura (see Figs. 29-2 and 29-3). The cupula is the most cranial convex portion of the diaphragm on both the lateral and the dorsoventral or ventrodorsal views. Also on these views, the thoracic surface of the diaphragm may be visualized as one, two, or three convex projections into the thoracic cavity (see Figs. 29-4 and 29-5). Several normal variations of diaphragmatic position and shape may be seen radiographically. Factors that cause this variable appearance are real and apparent. Real factors consist of breed, age, obesity, respiration, and gravity. Apparent factors are x-ray beam centering and animal positioning during radiographic examination. Many combinations are possible when all permutations of these variables are considered.4 Most of these variables are not radiographically significant; however, some must be recognized and understood. Changes most apparent radiographically are the position, shape, and visualization of the cupula and crura. The relative position of the crura depends mostly on position and size of the animal and primary x-ray beam centering. The most dependent crus is usually displaced cranially when an animal is in lateral recumbency. In right lateral recumbency, the crura appear to be parallel (see Fig. 29-3); in left lateral recumbency, they sometimes appear to cross. The crura also appear to be more extensively separated, by up to 2.5 vertebral lengths, if the animal is rotated slightly or if the x-ray beam is centered over the mid or cranial thorax.4 The radiographic appearance of the diaphragm in ventrodorsal or dorsoventral projections varies with x-ray beam centering. The diaphragm may appear as two or three separate domed-shaped structures (see Fig. 29-4) or as a single dome-shaped structure (see Fig. 29-5). The three structures represent the cupula and two crura. A single domed diaphragm may be seen on a ventrodorsal view when the x-ray beam is centered on the mid-abdomen or on a dorsoventral view when the x-ray beam is centered mid-thorax. Two or three separate domed structures are seen when the animal is in the ventrodorsal position and the x-ray beam is centered mid-thorax or on a dorsoventral view with the x-ray beam is centered mid-abdomen.4 Separate diaphragmatic structures are not seen as distinctly in the cat, probably because of the relatively small thoracic size (Fig. 29-6). On extreme inspiration, particularly if the animal is in respiratory distress, small symmetric muscle projections are noted from the thoracic diaphragmatic surface in the ventrodorsal or dorsoventral view (Fig. 29-7). This has been referred to as tenting of the diaphragm and is discussed in Chapter 33 in reference to pulmonary hyperinflation. The signs directly associated with the diaphragm are not as numerous and specific as those in many other organs. Radiographic changes observed most frequently with diaphragmatic disease include general or focal loss of the thoracic diaphragmatic surface outline and changes in diaphragmatic shape and position (Table 29-1). Table • 29-1 Radiographic Signs of Diaphragmatic Disease The thoracic diaphragmatic surface outline will not be visualized radiographically if soft tissue or fluid contacts the surface. Changes in diaphragm shape occur most frequently on the cupula; they are often normal and are frequently caused by contact with the heart (Fig. 29-8) or position of the animal during radiographic examination. The shape and position may also appear altered in some large-breed dogs, with the body appearing more convex and extending to a more cranial position in the thorax. This may be the result of a flaccid tendinous membrane, or it may be associated with a peritoneopleural hernia, which often produces no clinical signs. Positional changes consist of cranial and caudal displacement. Because the position of the diaphragm changes during the respiratory cycle, minor changes are difficult to diagnose and in most instances are not clinically significant. Severe positional changes may be significant and indicative of thoracic or abdominal disease. Cranial diaphragmatic displacement is usually associated with abdominal disease (see Table 29-1) or generalized diaphragmatic paralysis, which should be confirmed by fluoroscopic observation. Caudal diaphragmatic displacement is usually associated with severe respiratory disease (Fig. 29-9). The caudally positioned diaphragm is an attempt by the animal to increase the level of systemic oxygenation, which may be low because of ventilation or perfusion deficiencies in the lungs. Bilateral tension pneumothorax may also cause a caudally displaced diaphragm from increased pleural pressure. Abdominal trauma is the most common cause of diaphragmatic hernia. A high momentary increase in abdominal pressure when the glottis is open produces a high pleuroperitoneal pressure gradient that may result in a diaphragmatic hernia. The high pleuroperitoneal gradient may produce a rent in the muscular portion of the diaphragm, or it may force abdominal viscera through congenitally weak or defective areas. Clinical signs that may be observed with diaphragmatic hernias include dyspnea, pain, vomiting, regurgitation, muffled heart sounds, and a weak femoral pulse.5,6 Some diaphragmatic hernias may not cause clinical signs and are detected incidentally. Radiography plays an important role in confirming a diagnosis of diaphragmatic hernia and may provide information about location, extent, contents, and secondary complications associated with the hernia.7–11 If a diagnosis cannot be confirmed from survey radiographs (Box 29-1), ultrasonography and/or other imaging procedures may be performed to provide additional diagnostic information. Other radiographic procedures consist of administration of oral barium sulfate, positional radiographic views, removal of pleural fluid and repeat radiography of the thorax, and positive contrast-medium peritoneography. To ascertain the position of the stomach and proximal small bowel, a small amount (20 to 40 mL) of barium sulfate (30% w/v) can be given orally and radiographs obtained after 15 to 20 minutes (Fig. 29-10). Radiographs made with a horizontal x-ray beam help differentiate solid abdominal organs in the thorax from pleural fluid (Fig. 29-11). Thoracocentesis and pleural fluid removal followed by another radiographic examination provide better radiographic visualization of structures within the thorax. Positive-contrast peritoneography can be performed by injecting 2 mL/kg body weight of an iodinated, preferably nonionic, contrast medium into the peritoneal cavity. The animal should then be positioned such that gravity facilitates contrast medium accumulation around the liver and the diaphragm. Contrast medium within the thorax and an interrupted outline of the abdominal diaphragmatic surface are the most consistent positive-contrast peritoneographic signs of a diaphragmatic hernia (Fig. 29-12).12
The Diaphragm
Normal Radiographic Anatomy
Radiographic Signs of Diaphragmatic Disease
RADIOGRAPHIC SIGNS
CAUSES
General loss of diaphragmatic thoracic surface outline
Bilateral pleural fluid
Generalized pulmonary disease in caudal lung lobes
Localized or partial loss of the thoracic surface outline
Thoracic masses adjacent to the diaphragm
Diaphragmatic hernias
Focal pulmonary disease in caudal lung lobes
Shape changes
Thoracic masses adjacent to the diaphragm
Hiatal hernias
Small diaphragmatic hernias
Pleural reaction on the diaphragmatic surface
Neoplasia arising from the diaphragm
Hemiparalysis of the diaphragm
Unilateral tension pneumothorax
Position Changes
Cranial displacement
Obesity
Peritoneal fluid
Abdominal pain
Abdominal masses or organ enlargement; liver enlargement and masses frequently cause cranial displacement
Generalized diaphragmatic paralysis
Cranial displacement of the cupula caused by a diaphragmatic defect with the peritoneum and pleura intact
Caudal displacement
Severe respiratory distress—ventilation or perfusion problems
Tension pneumothorax
Caudal displacement of the cupula caused by contact with the heart
Diaphragmatic Diseases
Diaphragmatic Hernias
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The Diaphragm