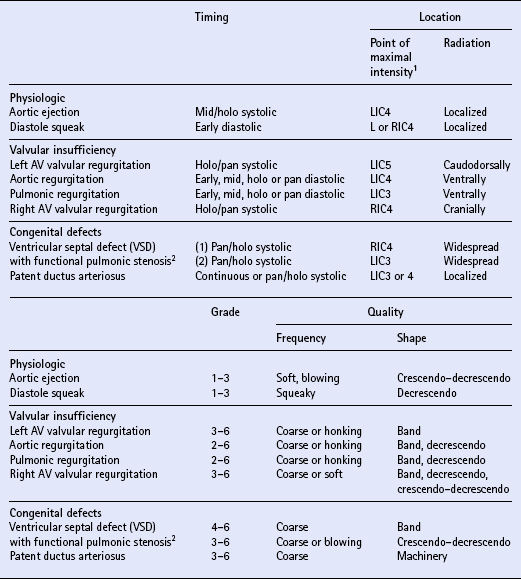
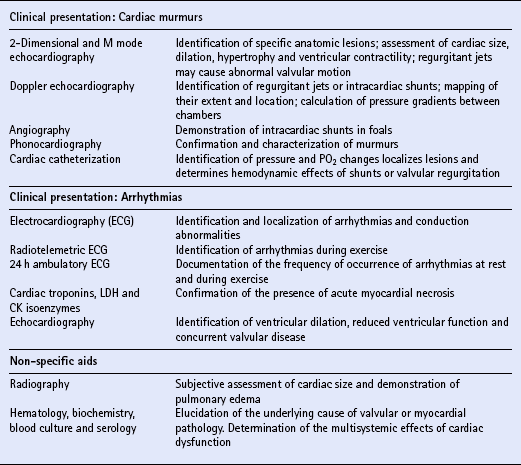
Chapter 8 In horses, the prevalence of cardiovascular disease is low although it can cause poor performance (q.v.) or cardiac failure and is frequently implicated in sudden death. Cardiovascular diseases can be classified on anatomic, pathologic or functional criteria. A functional approach serves the clinician well as it defines clinical manifestations and, often, appropriate management. A functional classification of equine heart disease is listed in Table 8.1. Table 8.1 Pressure overload occurs when there is an anatomic or physiologic obstruction impeding ventricular ejection. In response to increased afterload, the myocardial cells in the affected ventricle increase in diameter as myofibrils are laid down in parallel within them. Myocardial failure occurs as cellular function deteriorates. Lesions resulting in pressure overload such as aortic or pulmonic stenosis are uncommon in horses and this form of heart failure is rare. Both volume and pressure overload ultimately lead to failure of the affected ventricle. Accumulation of fluid and congestion in the vascular compartments develops “upstream” to the affected ventricle. Left-sided heart failure leads to congestion in the pulmonary circulation, pulmonary edema and respiratory signs ( Box 8.1). Right-sided heart failure leads to fluid accumulation in the systemic circulation, signs of venous distension and ventral edema. There can be effusions in the pleural and peritoneal cavities and, rarely, bowel edema and diarrhea ( Box 8.1). Usually, failure of one ventricle will lead to failure of the other, so that biventricular failure ensues and the clinical presentation includes both left- and right-sided signs ( Box 8.1). Primary myocardial (pump) failure implies that there is a primary defect in myocardial contractility leading to a reduction in stroke volume. The low cardiac output reduces perfusion and can lead to multiple organ dysfunction (see Box 8.1). This is seen in association with severe cardiomyopathies. Clinical signs produced by low cardiac output will also occur as myocardial failure develops in volume or pressure overload. Where the venous return is severely compromised, e.g. by effusive pericarditis (q.v.), low output heart failure also occurs. Physical examination including visual inspection and palpation provides a useful guide to hydration status, circulating volume and the efficiency of perfusion. The skin turgor, venous filling and moistness of the mucous membranes reflect total body water, while the color of the membranes, the capillary refill time, the temperature of the extremities and the pulse volume are indicators of circulating volume and perfusion. The horse has four heart sounds, although in some horses only two or three may be audible. The second heart sound is coincident with closure of the semilunar valves and reversal of blood flow in the great arteries at the conclusion of ventricular systole. The aortic and pulmonic valves may not close synchronously and physiologic splitting of the second heart sound is often found. The criteria used to describe murmurs are described in Box 8.2. If all five characteristics of a murmur are considered carefully, the clinician is usually able to formulate a differential diagnosis and differentiate those murmurs that are physiologic (functional) from those that indicate that there is cardiac pathology and justify further diagnostic evaluation. Functional murmurs are quieter (grade 3 or less), soft and localized, do not have precordial thrills and do not obscure the heart sounds. Functional murmurs in systole caused by ventricular ejection are localized to the heart base in the third or fourth intercostal space; they are usually grade 3 or less and have a soft, blowing quality. Functional diastolic murmurs occur in early or mid diastole, are frequently musical or squeaky, and are auscultated over the left heart base or left AV valve area. The characteristics of functional murmurs and those associated with a variety of forms of cardiac pathology are compared in Table 8.2. There are a wide variety of diagnostic aids available for use in the evaluation of equine cardiovascular disease. The selection of appropriate diagnostic procedures depends on the clinical presentation and the differential diagnosis. Table 8.3 summarizes some of the diagnostic techniques that are used in equine cardiology. Echocardiography is the principal means of evaluation of horses with cardiac murmurs where valvular pathology or congenital cardiac diseases are suspected. Normal values for various M mode echocardiographic parameters are listed in Table 8.4. Table 8.3 Summary of diagnostic techniques in equine cardiology Modified with permission from Marr, C.M. (1990) Ancillary aids in equine cardiology, Equine Veterinary Education 2: 18–21. Table 8.4 Normal M mode echocardiographic values for adult horses 1The ieft ventricular fractional shortening is normally ≤40% at heart rates of less than 50 bpm. 2At heart rates of less than 50 bpm. Reproduced with permission from Bongura et ai. (1985) Veterinary Clinics of North America 1:311-333. Electrocardiography, including radiotelemetric and ambulatory electrocardiography, is the principal means of investigation of arrhythmias. Non-specific aids are used to investigate the etiology of certain cardiac diseases and to assess the other body systems that may be affected secondary to cardiac disease. Myocardial disease is characterized by cardiac arrhythmias and/or ventricular dysfunction with ventricular dilatation and reduced myocardial contractility. The presenting signs depend on the severity of myocardial dysfunction and range from varying degrees of exercise intolerance to signs of congestive or low output heart failure in severe cases (see Box 8.1). The diagnostic procedures that are useful in investigation of myocardial disease are listed in Table 8.3. Echocardiography is used to assess ventricular function while electrocardiography is used to categorize arrhythmias and can reveal S-T segment changes or changes in the duration of complexes. Prolongation of ECG intervals may be associated with primary myocardial disease, however this should alert the clinician to the possibility of electrolyte or metabolic imbalances. Therapy for myocardial dysfunction includes rest, diuretics (furosemide) and, if the horse is showing signs of heart failure, positive inotropic agents such as digoxin or, in emergency situations, dobutamine. Digoxin is contraindicated in ionophore poisoning. Activated charcoal or mineral oil may be beneficial in horses that are known to have ingested ionophore very recently. Careful cardiac auscultation will enable the detection of most cardiac arrhythmias in the horse and in some instances a tentative diagnosis can be made from auscultation alone. However, an ECG is required to diagnose definitively the type of arrhythmia present, and should always be performed if a pathologic arrhythmia is suspected (see Table 8.3). The base-apex lead is used routinely in the horse for assessment of the heart rate and rhythm because movement artifacts are minimized and waveforms are easily visualized. For the base-apex lead placement is as follows: 1. The negative (“right arm”) electrode is sited dorsal to the right scapula, or in the right jugular groove, two thirds of the way down the neck. 2. The positive (“left arm”) electrode is sited over the cardiac apex (just above the point of the elbow in the sixth intercostal space on the left side). 3. The ground (“right leg”) electrode is sited anywhere on the body, remote from the heart. Multiple leads can be necessary for the accurate diagnosis of some complex arrhythmias and the standard limb leads used in other species are adequate in the horse. PR, QRS and QT interval determinations are most commonly calculated from lead II ( Table 8.5). Table 8.5 Normal interval durations in the equine ECG (lead II)
The cardiovascular system
INTRODUCTION
Problem
Etiology
Volume overload
Acquired valvular disease (degenerative or inflammatory) Congenital defects (intra- or extra-cardiac shunts, valvular malformations)
Pressure overload
Congenital valvular defects (stenosis)
Myocardial failure
Primary myocardial disease (toxic, nutritional, viral, immune-mediated) Secondary myocardial disease (toxic, drug-induced, hypoxia, endotoxemia, septicemia, electrolyte or metabolic disturbances)
Arrhythmias
Primary myocardial disease (toxic, nutritional, viral, immune-mediated) Secondary myocardial disease (toxic, drug-induced, hypoxia, endotoxemia, septicemia, electrolyte or metabolic disturbances)
Diastolic failure
Pericardial disease (effusive or constrictive)
CLINICAL EVALUATION OF THE CARDIOVASCULAR SYSTEM
THE CIRCULATORY SYSTEM
THE HEART
CARDIAC MURMURS
DIAGNOSTIC AIDS IN EQUINE CARDIOLOGY
Range (mean)
Right ventricle: diastole
32-52 (38.6) mm
Ventricular septal thickness: diastole
19-43 (30.6) mm
Ventricular septal thickness: systole
35-62 (48.1) mm
Left ventricular internal dimension: diastole
80-130 (110.6) mm
Left ventricular internal dimension: systole
43-79(61.1) mm
Left ventricular wall thickness: diastole
20-40 (29.2) mm
Left ventricular wall thickness: systole
32-56 (44.5) mm
Left ventricular fractional shortening
32-55 (44.1) o/o 1
Septal-left AV valve E point separation
<10 mm
Left auricular dimension
35-75 (56.4) mm
Aortic root dimension
55-90(73.1) mm
Left ventricular ejection time
<0.45s 2
MYOCARDIAL DISEASE
CARDIAC ARRHYTHMIAS
Diagnosis of arrhythmias
Interval
Duration
P-R
0.22–0.56 s
QRS
0.08–0.17 s
Q-T
0.32–0.64 s ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The cardiovascular system
Only gold members can continue reading. Log In or Register to continue