CHAPTER 47 Tetanus
Tetanus was first described in Egypt more than 3000 years ago and was familiar throughout the ancient world.1,2 In 1890, von Behring and Kitasato3 demonstrated that rabbits produced neutralizing antibodies in response to the administration of small doses of tetanus toxoid. Two years later, von Behring immunized sheep and horses against tetanus toxin to produce commercial quantities of antitoxin, and equine antitoxin was used extensively in injured soldiers during World War I. In 1927, Ramon and Zoeller4 developed a vaccine from tetanus toxin; a similar vaccine for horses was first used in the 1940s.
ETIOLOGY
Tetanus is caused by exotoxins produced by Clostridium tetani, a motile, anaerobic, gram-positive bacillus. C. tetani is a ubiquitous soil inhabitant and can be isolated from feces of domestic animals, including horses.5 Endospores are formed that give the sporulating organism a drumstick appearance.1 They are not completely destroyed by boiling but can be eliminated by autoclaving at 115° C (239° F) for 20 minutes.6 Toxin may account for 5% of the mass of the organism during proliferative growth.7 It has been estimated that the lethal dose for humans is 500 pg/kg.8 Among animals, the horse is considered most sensitive to tetanus toxin.9
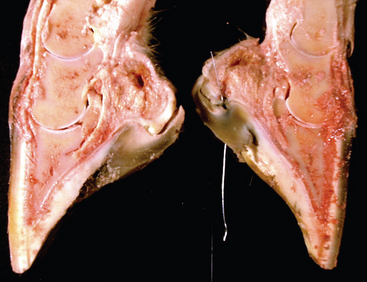
The most common route of infection is inoculation of wounds with C. tetani spores (Fig. 47-1). Puncture wounds contaminated by manure, soil, or rusty metal are especially likely to cause tetanus. In 18 horses with tetanus after known wounding, nine had lesions of the lower limb, six had punctures in the solar surface of the hoof, and two had wounds on the face.10 Contaminated surgical sites, the postpartum uterus, injection abscesses, and infected umbilical structures are also potential sites for C tetani infection. Causative wounds were not found in 2 of 20 horses with tetanus10 and reportedly are not found in 15% to 30% of human cases.
EPIDEMIOLOGY
Tetanus occurs in all parts of the world but is most likely in closely settled areas that are intensively farmed. Although the disease is rare in developed countries, tetanus is still important worldwide. In 1992, more than 1 million human deaths were still caused by tetanus, more than half of which were in neonates.11
PATHOGENESIS
The clinical signs of tetanus are caused by exotoxins encoded on a 75-kilobase plasmid.12 Two toxins are produced: tetanolysin and tetanospasmin.13 Tetanolysin damages viable tissue, lowering the redox potential and creating favorable conditions for expansion of the anaerobic infection.14 Tetanospasmin is produced as a single, inactive, 150-kilodalton polypeptide comprising three linked domains: L, HN, and HC. The peptide is activated by posttranslational, single-site proteolysis into active, heavy (H) and light (L) chains connected by a single disulfide bond. After its production by proliferating organisms, active tetanospasmin diffuses locally and circulates in the bloodstream to peripheral nerve terminals throughout the body. Tetanospasmin does not enter the central nervous system (CNS) directly, except at the fourth ventricle. At nerve endings, the lectinlike HC domain binds to membrane gangliosides GD1b and GT1b. The toxin is then internalized and transported retrograde in axons at 75 to 250 mm/day.15 After 1 to 14 days the toxin enters the CNS, traverses the synaptic cleft, and binds irreversibly to presynaptic inhibitory interneurons.2 Following HC-mediated binding to membranes, the entire toxin is internalized by a process requiring HN. Within the endosome, the disulfide link is reduced, and the L chain is released into the cytosol. The L chain is a zinc metalloproteinase that cleaves synaptobrevin, a protein necessary for exocytosis of neurotransmitter vesicles.13,16 In inhibitory interneurons, the light chain thus prevents release of the inhibitory neurotransmitters glycine and gamma-aminobutyric acid (GABA).17 This results in the sustained excitatory discharge of alpha motor neurons, evident clinically as muscle rigidity and muscle spasms.14
Preganglionic autonomic neurons in the lateral column of the gray matter and parasympathetic centers are affected by a similar mechanism, but with delayed kinetics compared to somatic motor neurons.18 Autonomic dysfunction therefore occurs days after spasms begin, probably because of relatively slow transport of toxin in the autonomic nerves.2 There is both a basal increase in sympathetic activity and episodes of intense hyperactivity (“autonomic storms”) involving both α-adrenergic and β-adrenergic receptors. During autonomic storms the concentration of circulating catecholamines increases up to tenfold. The resulting sympathetic overactivity causes hemodynamic instability and is an important cause of death in ventilated patients with tetanus.
The tetanus toxin also acts at the neuromuscular junction to cause muscle paralysis.19 This botulinum-like effect causes the facial paralysis characteristic of the rare cephalic form of tetanus; however, any paralysis usually is overridden by spasmogenic effects at the inhibitory interneuron. Tetanospasmin also has been shown in experimental animal studies to have a cortical convulsant effect.20 Whether this contributes to tetanic spasms in horses is unknown.
Neuronal binding of toxin is thought to be irreversible.21 Recovery requires growth of new nerve terminals, a process that is completed in weeks to months.
CLINICAL FINDINGS
The time from wound inoculation by C. tetani to development of first clinical signs can range from 1 day to more than 60 days, but usually is 7 to 10 days. In a series of 18 horses with tetanus, signs were first seen 2 to 21 days after wounding, with an average incubation period of 9 days.10 The period of onset (time from first sign to first spasm) has not been reported for equine cases but probably is similar to the 1 to 7 days reported for humans.1
Generalized, localized, and cephalic forms of tetanus are described in humans. By far the most commonly recognized form in horses is generalized tetanus. Neonatal tetanus is always of this type. Probably because cranial somatic nerves are shorter than nerves to the limbs, the first signs of tetanus are associated with rigidity of muscles around the head and neck. Increased tonus of the masticatory muscles (trismus), rigidity of facial expression (risus sardonicus), and neck stiffness are typical presenting signs10,22–27 (Fig. 47-2). Prolapse of the nictitans begins during this phase9 (Fig. 47-3). The head and neck are held in an extended position, and the face has a fixed, anxious expression. Often, the mouth is clamped shut, and the jaws cannot be pried apart manually (lockjaw). Hyperthermia (usually <39.1° C [102.5° F]) occurs in some horses during the early stages, and rectal temperature may rise further after tetanic convulsions.9

Fig. 47-2 Extensor rigidity observed in foal with tetanus secondary to umbilical abscess.
(Courtesy Dr. John Barnes.)
In mildly affected horses, signs may be restricted to the head and neck (Box 47-1). Moderately affected horses exhibit signs of dysphagia because of pharyngeal involvement, and rigidity extends to the muscles of the limbs, trunk, and tail. These horses also adopt a “sawhorse” posture, with rigid extension of the neck, back, and limbs and elevation of the tailhead10,26,27 (see Fig. 47-2). The gait appears stiff and stilted. In severe tetanus, affected animals are recumbent, and respiratory muscles are affected.