CHAPTER 4 Surgical Correction of Abnormalities Affecting the Reproductive Organs of Stallions
INGUINAL HERNIATION AND RUPTURE
Inguinal herniation in the stallion occurs when intestine, usually the ileum or distal portion of the jejunum, enters the vaginal sac or cavity (i.e., the inguinal canal) through the vaginal ring. If intestine extends into the scrotum, this herniation is sometimes referred to as scrotal rather than inguinal,1 but the terms are used interchangeably. Inguinal hernias of stallions are sometimes improperly referred to as “indirect hernias,” a term used to describe a similar condition in human beings.
Ruptured inguinal (scrotal) herniation occurs when herniated intestine protrudes through a rent in the vaginal sac into the subcutaneous tissue of the scrotum.2 Inguinal rupture is protrusion of viscera into the subcutaneous tissue of the inguinal canal or scrotum through a rent in the peritoneum and musculature adjacent to the vaginal ring.1 Inguinal ruptures in horses are sometimes inappropriately termed “direct hernias,” which is terminology borrowed from a somewhat similar condition in human beings. Direct hernias in human beings are caused by weakening of the inguinal musculature and are lined by peritoneum, whereas inguinal ruptures of horses are not lined by peritoneum. Direct herniation predominates in human beings, whereas inguinal herniation (i.e., indirect herniation) predominates in stallions.
Most inguinal hernias of foals are congenital and hereditary.3 They occur when a vaginal ring is so large that it permits viscera to enter the vaginal sac. Congenital inguinal hernias in foals may occur unilaterally (usually on the left side) or bilaterally and may occur more frequently in Standardbreds, Tennessee Walking horses, and American saddlebred horses.4,5
Ruptured inguinal hernias occur most commonly in foals and may be caused by high abdominal pressure generated during parturition.2,6 Inguinal hernias in adult stallions are generally acquired, but the underlying cause is usually a congenitally enlarged vaginal ring. The left vaginal ring is the ring most commonly involved.5 Herniation has been reported to occur during breeding or exercise,7 but it has also been identified in stallions being transported and in stallions confined to a stall. The incidence of acquired inguinal herniation is higher in Standardbreds, American saddlebreds, and Tennessee walking horses than in the general equine population,4,7 and the higher incidence in these breeds may be attributable to herniation of viscera through a congenitally enlarged vaginal ring. Inguinal ruptures in horses are rare and usually occur after a traumatic event.1
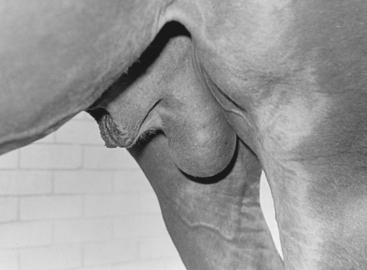
Inguinal hernias, ruptured inguinal hernias, and inguinal ruptures usually cause a noticeable increase in the size of the scrotum. Palpation of the scrotum of an affected horse may elicit a sensation of crepitus, and peristalsis of entrapped intestine may cause movement of scrotal skin. The contents of congenital inguinal hernias in foals, because of the relatively large size of the vaginal ring, are rarely strangulated and reduce easily. Rupture of a congenital inguinal hernia should be suspected if the viscera cannot be reduced, if the scrotum is cold and edematous, or if the hernia is accompanied by signs of colic.2,6
Foals with a congenital inguinal hernia should be monitored regularly by palpation for signs of strangulation. The hernia often resolves spontaneously by the time the foal is 3 to 6 months old, but the mechanism by which this occurs is not well understood.1,8,9 Application of a truss may hasten resolution (Fig. 4-1). The truss is applied with the foal in dorsal recumbency after the hernia has been reduced manually. Care should be taken to avoid interfering with urination by compressing the penis with the truss. The truss is usually changed at 3- to 5-day intervals. The hernia is often corrected within 1 to 2 weeks following application of the truss.

Fig. 4-1 “Diaper” applied to a foal to correct bilateral inguinal hernias.
(From Varner DD, Schumacher J, Blanchard TL, Johnson L: Diseases and Management of Breeding Stallions. St. Louis, 1991, Mosby.)
Congenital inguinal hernias of foals can also be corrected laparoscopically with the foal anesthetized and positioned in dorsal recumbency.10,11 After the contents of the hernia are reduced, the testis of the affected side is either removed laparoscopically or left in situ, and the vaginal ring is closed with a laparoscopic stapling device. Laparoscopic correction of congenital inguinal herniation is relatively quick and allows the foal to return quickly to normal activity.
Stallions with an acquired inguinal hernia, a ruptured inguinal hernia, or an inguinal rupture demand immediate attention, because the intestinal contents of the hernia nearly always rapidly strangulate. Reduction by external manual manipulation or rectal traction on inguinally incarcerated intestine is described,12 but is difficult and rarely successful. Surgical reduction of an acquired inguinal hernia is necessary if the viability of the affected testis or incarcerated intestine is uncertain.
To surgically reduce inguinally incarcerated intestine, the stallion should be anesthetized, positioned in dorsal recumbency, and prepared for inguinal exploration and celiotomy at the ventral midline. A cutaneous incision is created over the superficial inguinal ring or scrotum, the vaginal sac and its contents are isolated using blunt dissection, and the vaginal sac is incised to expose the testis, its spermatic cord, and the incarcerated intestine. Incarcerated intestine is most easily reduced by placing traction on it through a small ventral midline celiotomy. Often, the vaginal ring is so constricting that the intestine cannot be returned to the abdominal cavity without first enlarging the ring. The ring can be enlarged by cutting it with a curved bistoury or scissors.
Devitalized intestine (Fig. 4-2) can be resected and anastomosed at the inguinal incision, but resection and anastomosis are usually more easily accomplished after the intestine is returned to the abdominal cavity and exteriorized through a celiotomy at the ventral midline. Attempting to save the testis is impractical unless it and its vasculature appear to be undamaged. To remove the testis, the scrotal ligament is severed. The spermatic cord, including the parietal tunic, is ligated with heavy absorbable suture and severed distal to the ligature. The superficial inguinal ring is closed with a continuous or interrupted pattern using heavy absorbable suture. Inguinal fascia and skin can be sutured or left unsutured to heal by second intention. After removal of the affected testis, compensatory hypertrophy of the remaining testis may occur.13
TORSION OF THE SPERMATIC CORD
Torsion of the spermatic cord occurs when a portion of the spermatic cord rotates around its vertical axis.14 Torsion of the spermatic cord is sometimes incorrectly referred to as testicular torsion. Torsions of 180 degrees or less seem to cause no discomfort to stallions and are often considered to be an incidental finding,15 but torsion of a spermatic cord of 180 degrees may cause retrograde blood flow, indicating that torsion of this degree may have an injurious effect on testicular function.16 Torsions of 360 degrees or more cause acute venous and arterial occlusion of testicular blood supply, and if the rotation is not reduced quickly, the testis and spermatic cord distal to the torsion become gangrenous.14,15,17,18
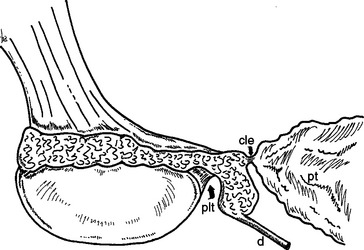
In human beings, torsion of the spermatic cord nearly always occurs intravaginally (within the vaginal tunic) rather than extravaginally (outside the vaginal tunic),14 and likewise, torsion of the spermatic cord of the stallion apparently occurs primarily intravaginally.15,17,18 Torsion may be caused by an abnormally long caudal ligament of the epididymis (ligament of the tail of the epididymis)15 or by an abnormally long proper ligament of the testis (Fig. 4-3).18 The gubernacular attachments of the contralateral testis may also be abnormally long, making that testis prone to torsion.18 Torsion of the spermatic cord of horses is infrequently reported,18,19 but torsion of 180 degrees is detected occasionally during examination of the external genitalia of the stallion. The spermatic cord of abdominally located testes may be more prone to torsion and may lead to gangrenous changes in the affected testis.19
Signs of torsion of the spermatic cord of stallions include scrotal swelling and signs of colic.15,17,18 Other diseases, such as inguinal herniation, orchitis, and epididymitis, produce similar signs, but these diseases can usually be excluded by palpation of the scrotal contents, examination of the vaginal rings by palpation per rectum, and ultrasonography. Normally, the head of the epididymis lies on the cranial pole of the testis, the tail lies at the caudal pole, and the body attaches to the dorsolateral border of the testis. With torsion of 180 degrees, the tail of the epididymis lies cranial, but with torsion of 360 degrees, the testis and epididymis may appear to be correctly aligned. The affected testis and cord are enlarged and firm, and the testis may appear to be surrounded by fluid.17,18 With torsion of 360 degrees or more, the scrotum and its contents may be so swollen that palpation of the epididymis is not possible. Ultrasonographic examination of the affected testis and cord may reveal increased fluid density throughout the affected side of the scrotum.18 Torsion of the spermatic cord of an abdominal cryptorchid testis may cause the affected horse to show mild signs of colic,20 but affected horses may display no signs of colic.21
A 360-degree torsion of the spermatic cord typically necessitates removal of the affected testis. If the testis is salvageable, orchiopexy using nonabsorbable suture can be performed to permanently fix the testis in its proper position.18 One suture is placed at the cranial aspect of testis and one at its caudal aspect. The suture is passed through the adjacent dartos tissue, vaginal tunic, and tunica albuginea. The surgeon should consider performing orchiopexy on the contralateral testis, because it may also be prone to torsion. Transient torsion of the spermatic cord of human beings may result in formation of antisperm antibodies or release of other factors that may affect fertility,22 but the effect of transient torsion of the spermatic cord of stallions is not known.
HYDROCELE
A hydrocele is a pathologic accumulation of serous fluid between the visceral and parietal layers of the vaginal tunic.23–26 Because of the insulating effects of the fluid, temperature-induced dysfunction of spermatogenesis is generally thought to occur, although one study did not reveal a substantial effect of hydrocele on semen quality. The vaginal tunic is secretory, and fluid produced by the vaginal tunic is resorbed through the veins and lymphatic vessels of the spermatic cord.27 Hydrocele results when production of fluid by the vaginal tunic is increased or resorption is decreased. Hydroceles may accompany testicular neoplasia or scrotal trauma or they may be idiopathic. Some forms of idiopathic hydroceles may occur during hot weather, sometime in association with restricted exercise.26 Because the vaginal cavity communicates with the peritoneal cavity, a hydrocele may form as an extension of ascites.24 Migration of parasites into the vaginal cavity and associated structures has been implicated as a cause of hydrocele.23
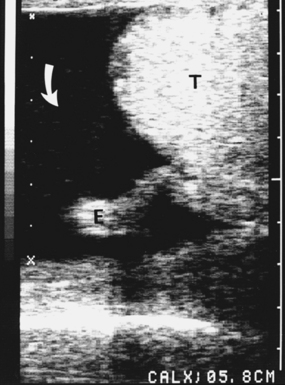
A hydrocele appears as a painless, fluid-filled scrotal enlargement.23–25,27 It may occur bilaterally or unilaterally and may develop acutely or insidiously. If the hydrocele is chronic, the testis within the affected tunic may become smaller than normal due to atrophy. A hydrocele can usually be differentiated from other diseases that cause scrotal enlargement by palpating the scrotal contents, by examining the vaginal rings per rectum, and by using ultrasonography. Ultrasonographic examination of a hydrocele reveals anechoic or hypoechoic fluid surrounding the testis (Fig. 4-4). Diagnosis is verified by aseptic aspiration of a serous, amber fluid from the vaginal cavity.
Exercise may cause a temporary decrease in the size of a hydrocele, and occasionally, a hydrocele may resolve spontaneously. Aspiration of fluid from a hydrocele usually gives only transient relief because the fluid soon re-forms. Treatment of a stallion with a hydrocele should be aimed at removing the inciting cause, but because the cause can rarely be identified, the usual treatment of a stallion with persistent, unilateral hydrocele is removal of the affected testis and vaginal tunic to avoid disruption of spermatogenesis of the contralateral testis that may be induced by increased scrotal temperature. Prognosis for fertility can be guarded if bilateral hydroceles persist, although the condition has been reported to have no ill effect on fertility in some cases.26
Hydroceles of men were successfully treated by sclerotherapy using either 2.5, 5, or 10% solutions of tetracycline injected into the vaginal cavity.28 Injection of the sclerosant often caused severe pain, even if local anesthetic solution was injected into the vaginal cavity prior to treatment. Sclerotherapy, as a treatment for stallions with hydrocele, has not been reported.
HEMATOCELE
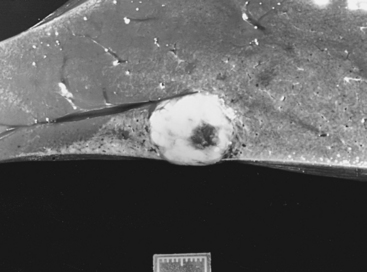
A hematocele resembles a hydrocele but is a collection of hemorrhagic, rather than serous, fluid within the vaginal cavity (Fig. 4-5).25,29 Hematoceles are usually caused by trauma to the scrotum and its contents, but because the peritoneal and vaginal cavities of the horse communicate, they can occur as an extension of hemoperitoneum.30
A small hematocele may cause no problem with fertility and may dissipate without treatment, but a large hematocele may insulate the testes, causing interference with spermatogenesis. A large hematocele should be evacuated from the vaginal cavity, and the testis and epididymis should be carefully inspected to identify the source of hemorrhage. The tunica albuginea, if torn, should be sutured. Orchidectomy is indicated if the testis or epididymis is badly damaged. The effect of testicular trauma on formation of antisperm antibodies and secondary subfertility in stallions is not known. Removal of the affected testis may be indicated to minimize the likelihood of such a complication and to prevent depression of spermatogenesis of the contralateral testis from increased temperature caused by inflammation of the scrotal contents.
VARICOCELE
A varicocele is a dilatation and tortuosity of the veins of the pampiniform plexus and the cremasteric veins (Fig. 4-6).24,25 Varicoceles of human beings and rams have been associated with testicular atrophy and decreased seminal quality, possibly caused by interference with normal exchange of heat from the testicular artery to the pampiniform plexus.24 Varicoceles of stallions are uncommon, and their effect on fertility is not documented. More than 50% of men with varicoceles have normal seminal quality.31 One of the authors (DV) has observed a varicocele in some stallions with normal seminal quality.
Most varicoceles are idiopathic, but a defect in the valves of the spermatic vein where it empties into the vena cava or renal vein, or a deficiency of elastic and fibrous tissue in the fascia that surrounds the spermatic vein has been postulated to cause varicoele.24 Varicoceles of stallions are usually unilateral and, when palpated, produce no signs of pain. The affected spermatic cord appears enlarged and may have the texture of “a bag of worms.”
Definitive treatment of stallions affected with varicocele is removal of the affected cord and testis, but therapy is unnecessary if seminal quality is unaffected. The venous loops of the pampiniform plexus have been ligated as treatment of human beings with varicocele.32 A hydrocele has formed in a small percentage of human beings following ligation of the spermatic vein.
TESTICULAR NEOPLASIA
Testicular neoplasms of the horse are encountered infrequently, probably because most horses are castrated at an early age. Only primary testicular neoplasms (i.e., those that originate within the testis) have been reported, and these can be divided into germinal and nongerminal types.33 Germinal neoplasms arise from the germ cells of the seminiferous epithelium and are the most common type of germinal neoplasm.24
Germinal testicular neoplasms reported to occur in the horse include the seminoma, teratoma, teratocarcinoma, and embryonal carcinoma. The seminoma is probably the most commonly reported testicular neoplasm of the horse. Nongerminal testicular neoplasms arise from testicular stromal cells and include the Leydig cell tumor and Sertoli cell tumor.33 Nongerminal testicular neoplasms of the horse are uncommonly reported. Cryptorchid testes of human beings and dogs appear to be predisposed to neoplasia,33,34 but for horses, a relationship between cryptorchidism and formation of testicular neoplasia has not been definitively established.
When examining a horse with a suspected testicular neoplasm, the clinician should use the contralateral testis for comparison, remembering, however, that bilateral testicular neoplasia can occur. The normal testis is smooth and compliant, and a neoplastic testis is often enlarged, with either a soft or hardened texture of the tumorous tissue. The neoplastic testis is often heavier than its normal counterpart. Small, neoplastic lesions located deep within the parenchyma may not be palpable. A neoplastic testis is usually painless when compressed and usually remains freely movable within the scrotum. Scrotal enlargement caused by neoplasia must be differentiated from other causes of scrotal enlargement, such as torsion of the spermatic cord, orchitis, hydrocele, hematocele, and inguinal herniation or rupture. Careful external palpation of the scrotal contents and palpation of the vaginal rings and viscera per rectum can be used to differentiate these conditions. Painless, scrotal enlargement that develops insidiously is more likely to be caused by testicular neoplasia than by inflammation or ischemia.
Ultrasonographic examination of the contents of the scrotum may be helpful in determining if a testis is neoplastic. Normal testicular parenchyma is homogeneously echogenic, but a neoplastic testis usually contains areas of decreased echogenicity. Affected testes may contain single or multiple tumors. Testicular neoplasia can be confirmed by cytologic examination of a needle aspirate or by histologic examination of a needle or incisional biopsy of the testis. Incisional biopsy has been associated with complications, but needle biopsy is unlikely to have injurious effects on the testis.35–38 Creation of antisperm antibodies and reduction in quality of semen reported to occur in other species after needle biopsy have not been found to occur in horses. Biopsy of neoplastic testes of human beings has been associated with a high incidence of neoplastic invasion of extratesticular tissue,39 and so, if testicular neoplasia is strongly suspected, the affected testis should be excised.
Before a neoplastic testis is removed, the iliac lymph nodes should be palpated per rectum to aid determination of whether the neoplasm has metastasized (Fig. 4-7). The neoplastic testis should be removed using the closed technique, and the spermatic cord should be ligated and severed as far proximally as possible. The spermatic cord should be examined grossly and histologically for evidence of metastasis. The scrotal incision should be sutured to reduce postoperative inflammation, which may interfere with thermal regulation of the remaining testis, but good hemostasis is required before the scrotal incision is sutured.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree