Chapter 68 Surgery of the Stomach
Retrieval of foreign bodies is the most common reason for surgery on the stomach. Surgery of the pylorus is most often indicated for some forms of gastric outflow obstruction. The most common sign related to surgical disease of the stomach is emesis. The stomach has an excellent blood supply and heals rapidly (10–14 days).
ANATOMY
Stomach
• The stomach lies in a transverse plane. The larger part of the stomach (fundus) lies to the left of the midline.
• The esophageal entrance and duodenal exit are dorsal—the former lying to the left of the midline, the latter to the right.
• In the fasting dog, the stomach does not extend caudally beyond the costal arch and is rarely palpable.
• The stomach has four tunics: mucosa, submucosa, muscularis, and serosa. The submucosa and mucosa layers are easily separated from the overlying seromuscular layers.
• The blood supply to the distal stomach is from a branch of the hepatic artery, giving rise to the right gastric and gastroepiploic arteries.
• The splenic artery gives rise to the left gastroepiploic artery, which supplies the greater curvature.
• The left gastric artery supplies blood to the lesser curvature of the stomach and the distal esophagus.
• Veins are satellites to the arterial branches. Most blood drains from the left side of the stomach via the gastrosplenic vein and from the right side via the gastroduodenal vein. These veins ultimately drain into the portal vein.
Omentum
• The greater omentum extends caudally from the greater curvature of the stomach to the urinary bladder, forming a double-layered cover of the small intestine.
• A splenic portion of the omentum attaches to the greater curvature to the spleen and a smaller portion attaches to the pancreas.
• The lesser omentum extends from the lesser curvature of the stomach and attaches to the diaphragm, liver, and duodenum.
Pylorus
• The pylorus is composed of two segments, the antrum and the canal. The antrum is a narrow funnel-shaped chamber leading to the narrowed pyloric canal.
• The inner circular muscle layer is thickened in the pyloric region and functions as a powerful sphincter. An outer longitudinal muscle layer is also present.
GASTROTOMY
• Endoscopic retrieval of gastric foreign bodies is preferred. When this approach fails, a gastrotomy is indicated.
Surgical Procedure
Technique
1. Make a cranial ventral midline abdominal approach, with the skin incision extending from the xiphoid to the umbilicus.
2. Exteriorize the stomach and isolate it from the other abdominal organs using moistened laparotomy pads.
3. Place two Babcock forceps or two stay sutures 10 to 15 cm apart on a hypovascular area of the stomach, halfway between the lesser and greater curvature.
Closure
1. The first layer is a continuous inverting horizontal mattress (Connell) suture pattern involving only the submucosal and mucosal layers. A simple continuous suture pattern can be substituted. Synthetic 3-0 absorbable suture material is preferred. Use of chromic gut suture material is discouraged, because it breaks down too rapidly when coming in contact with the lumen of the stomach.
2. Close the second layer with a vertical (Lembert) or horizontal (Cushing) continuous inverting pattern.
Postoperative Care and Complications
PARTIAL GASTRECTOMY RELATED TO GASTRIC DILATATION-VOLVULUS
Surgical Procedure
Technique
2. Non-viable tissue is recognized by its lack of bleeding on cut surfaces, bluish-black or greenish discoloration, and severe thinning of the stomach wall on palpation.
3. Ligate and divide the appropriate short gastric vessels. LDS stapler apparatus is optimal. This procedure may not be necessary because these vessels are frequently torn.
4. After placement of stay sutures, apply intestinal forceps 2 lateral to the junction of viable and non-viable tissue. The tips of the forceps meet at an approximately 45-degree angle.
5. Use a #10 scalpel blade to cut along the intestinal clamps, leaving a 1-cm margin of healthy tissue outside the intestinal clamps.
Alternate Method of Resection
1. Place a TA stapler parallel to the junction of viable and non-viable tissue, leaving a 1-cm width of normal tissue.
Postoperative Care and Complications
Surgical Procedure—Partial Gastrectomy and Gastroduodenostomy (Billroth I)
Objectives
• To remove diseased tissue that is benign or, if malignant, is limited to the antrum and/or body of the stomach.
Technique
2. Stapling devices (e.g., the GIA stapler) can be substituted for more traditional suturing techniques.
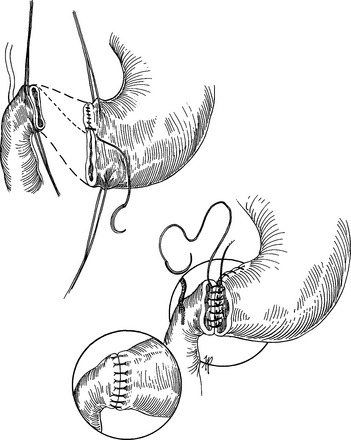
3. If the diseased tissue is limited to the pylorus, a modification of a Billroth I (von Haberer) technique can be done (Fig. 68-1).
5. More extensive resection of the pylorus or distal stomach can be done and reconstructed with the original Billroth I (Shoemaker) procedure (see Fig. 68-1).
6. After the line of resection is determined, ligate and divide the blood vessels supplying the lesser and greater curvature and attached omentum.
7. Mobilize the pylorus after incising the gastrohepatic ligament. Avoid cutting the common bile duct and hepatic arteries.
9. Place large, straight non-crushing intestinal forceps above and below the proposed lines of incision.
Closure
1. Use a single-layer interrupted appositional suture pattern to appose the stomach and duodenum. With unequal lumen sizes, first close the lesser curvature side of the stomach until the lumen disparity is corrected (see Fig. 68-1, top).
2. Appose the back (far) wall first, placing the knots into the lumen. Synthetic 3-0 absorbable suture (e.g., polydioxanone [PDS]) is recommended.