12.1 Variations in thickness of soft tissues331
12.2 Variations in radiopacity of soft tissues332
12.3 Contrast studies of sinus tracts and fistulae (sinography, fistulography)334
12.4 Contrast studies of the lymphatic system (lymphography, lymphangiography)334
12.5 Contrast studies of peripheral arteries and veins (angiography, arteriography, venography)335
12.6 Ultrasonography of soft tissues336
12.7 Ultrasonography of muscles, tendons and nerves337
12.8 Ultrasonography of superficial lymph nodes338
Soft tissues and fluid have a similar radiopacity, which is less than that of bone and other mineralized material and greater than that of gas. Fat is slightly less radiopaque than fluid and other soft tissues and can usually be distinguished from them. It is not usually possible, therefore, to distinguish different components of fluid or soft tissue structures within a region unless they are outlined by fat, gas or mineralized material, or unless contrast techniques are used. Fat in areas such as the abdominal cavity, pericardial sac, fascial planes and joints provides helpful contrast with other soft tissues and often aids interpretation. Magnetic resonance imaging (and to a lesser extent, CT) is the preferred technique when detailed soft tissue information is required. The use of ultrasonography for the musculoskeletal system is described briefly in Chapter 3. In the case of the limbs, evaluation of imaging abnormalities may be easier if the presumed normal contralateral body part is also evaluated for comparison.
12.1. VARIATIONS IN THICKNESS OF SOFT TISSUES
1. Diffuse increase in thickness of soft tissue.
a. Fat deposition – obesity; distinguished by fat radiopacity that is less than that of other soft tissues (seen subcutaneously, within fascial planes, and in the thoracic and abdominal cavities).
b. Muscular hypertrophy.
– In response to activity.
– Cats – feline hypertrophic muscular dystrophy; uncommon, leads to progressive muscular hypertrophy.
c. Oedema.
– Obstruction to venous drainage.
– Congestive heart failure.
– Hypoproteinaemia (secondary to renal, hepatic or intestinal disease).
d. Lymphoedema.
– Developmental anomaly of lymphatic drainage.
– Acquired obstruction to lymphatic drainage.
– Lymphangiosarcoma.
e. Cellulitis.
f. Diffuse or extensive neoplasia.
h. Emphysema (gas bubbles and streaks visible).
2. Focal increase in thickness of soft tissues.
a. Subcutaneous administration of fluids.
b. Skin folds – especially certain breeds, such as the English Bulldog and Shar Pei.
c. Seroma (e.g. following surgery).
d. Neoplasia – benign or malignant.
e. Cellulitis or abscess.
f. Haematoma.
g. Granuloma (e.g. lick granuloma, or soft tissue callus over a pressure point).
h. Hygroma.
i. Cyst.
j. Hamartoma.
k. Vascular malformation.
l. Compartment syndrome – elevation of interstitial pressure in a closed osseofascial compartment, usually due to vascular injury or trauma ± fracture; most commonly in a limb.
3. Decrease in thickness of soft tissues.
a. Emaciation – primarily loss of fat layer.
b. Muscular atrophy.
– Disuse (e.g. chronic lameness).
– Neurogenic.
– As a consequence of myositis.
12.2. VARIATIONS IN RADIOPACITY OF SOFT TISSUES
1. Increased radiopacity – but remaining of soft tissue opacity.
a. Increased thickness of soft tissues (e.g. given the same exposure, the soft tissues of the thigh will appear more radiopaque than those of the distal limb, due to their increased bulk).
b. Superimposition of skin or subcutaneous masses.
c. Superimposition of nipples.
d. Superimposition of engorged ticks.
e. Skin folds.
f. Positioning aids (e.g. foam wedges).
g. Wet or dirty hair or fur, or ultrasound gel – usually gives a streaky appearance.
2. Increased radiopacity – unstructured mineral opacity due to deposition of calcium salts or other minerals.
a. Artefactual, due to dirty intensifying screens or cassettes.
b. Surface application of some lotions or ointments.
c. Foreign material (e.g. dirt, glass).
d. Secondary to injection of corticosteroids.
e. Hyperadrenocorticism (Cushing’s disease) – calcinosis cutis (see below) and also mineralization of bronchopulmonary structures, kidney and sometimes other soft tissues; other features include hepatomegaly, osteopenia and adrenal masses.
f. Dystrophic calcification, i.e. deposition of calcium salts in damaged or diseased tissue.
– Secondary to trauma (e.g. calcifying tendinopathy).
– Chronic haematoma.
– Chronic abscess, granuloma or granulation tissue.
– Chronic necrosis (e.g. abdominal fat necrosis).
– Within a neoplasm.
– Cyst wall.
g. Metastatic calcification – calcification of soft tissues secondary to disorders of calcium and phosphorus homeostasis (e.g. kidneys, major blood vessels, gut wall).
– Pseudohyperparathyroidism (hypercalcaemia of malignancy), usually secondary to anal sac adenocarcinoma or lymphoma.
– Primary hyperparathyroidism – uncommon; usually older dogs, particularly Keeshond.
– Vitamin D toxicosis – cats are more sensitive than dogs; may die from renal failure prior to visible soft tissue mineralization.
h. Calcinosis cutis – granular deposits of calcium in the skin and/or linear streaks of calcium in fascial planes; usually secondary to hyperadrenocorticism (Cushing’s disease) but may also be seen secondary to hyperparathyroidism.
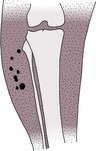
i. Calcinosis circumscripta (tumoral calcinosis) (Fig. 12.1) – young, larger-breed dogs, especially German Shepherd dogs, and rare in cats; amorphous calcium deposits within soft tissues, often attached to tendons, joint capsules or periosteum. Possibly associated with trauma, such as pressure points and at sites of previous surgery. Commonly recognized sites include the extremities or prominences of the limbs, the neck and the tongue, and it has also been reported in the spine, causing neurological deficits.
j. Chondrocalcinosis (pseudogout, calcium pyrophosphate deposition disease) – rare; unknown aetiology and mainly older animals; articular or periarticular deposition of calcium pyrophosphate crystals.
k. Idiopathic vascular calcification.
l. Iatrogenic – percutaneous injection of calcium-containing drug or long-acting corticosteroid.
3. Increased radiopacity – more structured mineral opacity that in some cases has trabecular detail suggestive of bone formation.
a. Normal anatomical structures or variants (e.g. sesamoids, clavicle, hyoid apparatus, separate centres of ossification).
b. Fragments of bone displaced from their normal position due to avulsion or other fractures.
c. Chronic tendinopathy.
d. Neoplasia.
– Extraskeletal osteosarcoma – described in a wide range of sites in both dogs and cats; variable degrees of mineralization, and some appear as soft tissue masses only.
– Multilobular tumour of bone – usually attached to adjacent bone but has been reported in axillary soft tissues.
– Other neoplasms may occasionally contain mineralization.
e. Heterotopic osteochondrofibrosis in association with von Willebrand’s disease – Dobermann, hip area (see 3.9.12).
f. Myositis ossificans – formation of non-neoplastic bone within striated muscle; termed heterotopic because it is in an abnormal position.
– Idiopathic.
– Secondary to trauma or chronic disease.
g. Cats – hypervitaminosis A; there may be extensive periarticular mineralization as well as periarticular and vertebral osteophytes (see 5.4.8).
h. Cats – osteochondromatosis: may have widespread soft tissue mineralization unconnected to adjacent bone.
i. Fibrodysplasia ossificans (Fig. 12.2) – rare, progressive disorder, especially cats; similar to myositis ossificans but differs in that the bone may displace muscle but does not involve it. Typically multiple, symmetrical lesions unrelated to trauma.
4. Increased radiopacity – metallic opacity.
a. Artefactual due to dirty intensifying screens or cassettes.
b. Surface application of lotions or ointments containing metallic salts.
c. Surface contamination with contrast medium.
e. Foreign material (e.g. bullets, air gun pellets, needles).
f. Migration of metallic implants originally in skeletal structures.
g. Surgical staples or wire sutures.
h. Microchip.
5. Decreased radiopacity of soft tissues.
a. Artefactual – overexposure or overdevelopment.
b. Decreased thickness of soft tissues.
c. Presence of fat.
– Normal or obese; linear fat deposits in a subcutaneous site and along fascial planes.
– Localized fatty mass (lipoma, liposarcoma, e.g. intermuscular lipomas in the thigh region of dogs).
d. Presence of gas (Fig. 12.3).
– Puncture, laceration or incision of skin.
– Secondary to subcutaneous or intramuscular injection.
– Penetration of the pharynx, oesophagus or trachea.
– Extension of pneumomediastinum.
– Within intestinal loops in a hernia or rupture.
– Infection with gas-forming organisms (uncommon).
– Sinus tract or fistula (for dermoid sinus see 5.7.4).
12.3. CONTRAST STUDIES OF SINUS TRACTS AND FISTULAE (SINOGRAPHY, FISTULOGRAPHY)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree