40 SAMPLE COLLECTION AND PREPARATION
6 Which size of needle and syringe should be used with the fine-needle technique (aspiration and nonaspiration)?
7 How is fine-needle aspiration performed?
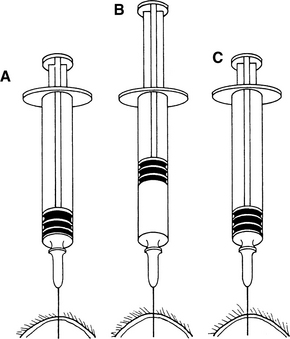
For fine-needle aspiration of cutaneous masses, the mass is stabilized between the thumb and index finger of one hand while the needle (with syringe attached) is introduced into the mass. Negative pressure is applied by rapidly withdrawing the syringe plunger two-thirds to three-fourths the syringe volume. Multiple areas of the mass should be aspirated. If the mass is large enough and the animal calm enough, the needle may be redirected in the mass while negative pressure is maintained. If the mass is small or the animal difficult to restrain, the negative pressure should be released, the needle redirected, and negative pressure reapplied (Figure 40-1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree