Chapter 4 In performing the procedures below the groom or owner must balance the need to interfere with the possible disturbance that this creates. It is suggested that parameters described for the APGAR score (see p. 69) are first established to determine the well-being of the foal. Assuming those parameters are normal and the birth process is considered normal, and there are no obvious risk factors, routine management procedures can be followed. • Ideally treatment should be initiated as soon as the cord has ruptured. This is because the stump is a very good portal of entry for bacteria into the bloodstream and until the foal has sucked colostrum it has no immunity to this infection. • Ideally the navel should be immersed in a 0.5% solution of chlorhexidine (Fig. 4.1).1 Dilute 1 part 2% chlorhexidine solution with 3 parts sterile water for a 0.5% solution. It is the authors’ experience that, although this preparation does decrease the incidence of umbilical stump infection, the stumps remain moist for a relatively longer period of time compared with the typical iodine preparations owing to poor desiccant effects. Consequently, a new recipe is now recommended such that, for every 500 mL of the 0.5% chlorhexidine solution made up with sterile water, the final 60 mL of this is in fact surgical spirit. • Dipping should be repeated every 6–8 hours for the first 24 hours. Spraying may potentially be a better method of application because the solution will be under mild pressure. • The use of povidone iodine has been called into question.1 The greatest reduction in bacterial colonization of the umbilicus after dipping has been shown to be with chlorhexidine as opposed to povidone iodine/2% iodine solutions. • Strong solutions of iodine or tincture of iodine can cause rapid desiccation of the umbilical stump and burning and necrosis of the surrounding skin. This predisposes to local infection and patent urachus. • The usefulness of aerosol antibiotic sprays (oxytetracycline, etc.) is questionable. These do not dry the stump as quickly as other preparations and all the time the stump is moist it is more prone to infection. In addition, the antibiotics are bacteriostatic and, therefore, the antibacterial effects are probably poor and non-persistent. The antibiotic may not be effective against the organisms present (many significant Gram-negative bacteria including E. coli are tetracycline resistant). However, the incorporated purple dye is at least an indicator that some attention has been given to navel health! • The usefulness of powder preparations is also questionable for similar reasons to the above but, in addition, the likelihood of powder penetrating into the natural crevices of the stump is poor and therefore some parts will remain a nidus for infection. Meconium consists of digested amniotic fluid and cell debris. It is never passed in fetal life unless there is fetal distress. Most foals pass meconium within 4 hours’ postpartum, and by 24 to 48 hours milk dung appears. Meconium retention is more of a problem in colt foals than in fillies (see p. 249). Enemas are often given prophylactically to foals by clients, either before or after the first suck (Fig. 4.2). The timing of administration can be argued either way and in practice appears to make very little difference. The type of enema used is the most important factor (100 mL phosphate-buffered solution is ideal, e.g. Fletchers®, Pharmax Ltd, Bexley, Kent, UK), and the amount of times it is given. It is important that a client knows to apply an enema only once and that if any foal continues to have problems then veterinary advice should be sought. (For treatment of meconium retention see p. 249.) At birth the oral nutrient intake becomes the sole source of nutrition and the importance of colostral antibody transfer cannot be overstated. Colostrum quality of the dam should be checked (see p. 391). If the quality is poor (i.e. < 50 g/L, < 1.060 or < 20%) then supplementation with donor colostrum is advisable before the first suck to prevent failure or partial failure of passive transfer of immunity. A local donor mare is the most suitable owing to the presence of antibodies to specific antigens or infections that she has encountered in the local environment. Fresh colostrum is better than frozen owing to the denaturing of complement in the freezing process. The uptake of IgG is greater if the foal is allowed to suck from a bottle rather than being stomach tubed (see p. 459). Unless the owner or stud groom is experienced with this procedure it is usually best for every placenta to be assessed by the veterinary surgeon. This could be performed during their visit to do a routine foal examination (see p. 69). Reduction in infestation rates can be achieved by chemotherapeutic or managemental control methods. The use of anthelmintic drugs to suppress fecal egg output has been the mainstay of strongyle control on studs for many years. However, this strategy can no longer be totally relied upon and managemental control is also vitally important (see below).2,3 Prophylactic use of anthelmintics usually involves giving the first dose at 6–10 weeks of age. If parasites are likely to be a problem treatment can begin at an earlier age. Anthelmintic treatment can be planned in three ways: as interval treatment, strategic treatment (based on seasonal transmission patterns), or targeted strategic treatment (based on individual fecal egg counts as well as seasonal transmission patterns). • Interval dosing: this involves the administration of a specific drug at regular time intervals during the high risk summer grazing period. • Strategic dosing: the use of anthelmintics at specific times of year to disrupt the seasonal cycle of transmission has been widely and effectively employed in farm animal practice. The seasonality of horse strongyles is well established so strategic dosing at turnout, in the middle of the grazing season and again in the autumn is a rational approach to parasite control. • Targeted strategic dosing: strategic dosing targeted at animals with significant (> 200 eggs/gram) adult parasite burdens to suppress pasture contamination at critical times of the year. • avoidance of high stocking density and overgrazed pasture • isolation of horses with high fecal egg counts • reducing year-to-year transmission by controlled grazing and management practices including resting pasture • avoidance of young/juvenile horses in the same fields as the foals • reducing translation of parasites to pasture by regular removal of feces from the pasture, twice weekly is the suggested frequency. Detailed examinations of a newborn foal are usually conducted within the first 3 days as a matter of routine to ensure the foal is healthy and to detect any congenital abnormalities and early signs of disease. Routine examinations are paramount because they allow identification of the high risk foal (see p. 60), enabling early diagnosis and intervention.4 Vital things to remember are: • changes occur rapidly – a normal foal can deteriorate within hours • it is essential that the clinician is familiar with normal parameters and postpartum changes (see p. 65). Usually most clients prefer the middle ground and ask for a single routine health check to be performed, and the clinical examination is normally recommended when the foal reaches 18–24 hours of age. This usually falls on day 2 postpartum and coincides with the blood sampling for routine IgG estimation (see p. 9) and with most insurance requirements. 1. Weighing and examination of placenta for abnormalities (see p. 43). 2. Clinical examination of the foal (see p. 69): 3. Tetanus antiserum administration: this is a routine procedure in almost all studs. However, if the mare is adequately vaccinated with tetanus toxoid in late pregnancy and colostral intake is good (serum IgG > 8 g/L) there will be adequate protection against tetanus in the neonate and, therefore, this can probably be left out. The dose of tetanus antiserum (Tetanus Antitoxin Behring®, Intervet Ltd, Bucks, UK) routinely used on many studs (regardless of the vaccination status of the mare) is 3000 i.u. subcutaneously given at or soon after birth. Higher doses (6000 i.u.) have been suggested,5 but in the field this high dose appears to be unnecessary. Tetanus antitoxin administered at this time usually provides up to 4–6 weeks of circulating immunity to tetanus in foals. 4. Administration of prophylactic antibiotics: prophylactic antibiotic use in newborn foals is controversial. However, many British stud farms use antibiotics as a matter of routine in all foals born. Recently, practitioners in the US have also begun using routine postbirth antibiotic administration to foals. Broad spectrum bactericidal drugs are preferred although a routine single injection of a ‘long-acting’ formulation of procaine penicillin (at 20 000 i.u./kg intramuscularly q 24 h) is commonly administered at birth or shortly afterwards. Given that most serious neonatal infections are Gram negative, penicillin would not seem to be the most appropriate choice of prophylactic antibiotic for newborn foals (this is effective only against Gram-positive organisms and there are many resistant bacteria). The occasional staphylococcal or streptococcal infection may be prevented by this. The common practice of a single dose of long-acting penicillin administered at birth is probably not useful and may be viewed as misuse of the antibiotic. However, many experienced clinicians report a benefit without significant problems. Potentiated sulfonamides are also often used at 20 mg/kg intramuscularly q 24 h. However, these injections can be painful and resented and a 12-hourly dose rate would be more therapeutic. 5. Early determination of IgG at 8–12 hours of age: early evidence for impending problems of failure of passive transfer can often be detected at this stage. However, many clinicians wait until peak serum IgG levels are obtained from 18 hours onwards, especially if financial restraints mean that only one routine visit to examine the foal is permitted. 3. Assessment of conformation with regard to exercise program: conformation and limb assessment and recommendations are made for amount and frequency of exercise, recheck, corrective trimming, hoof trim, etc. 4. Blood samples for routine hematology and biochemistry: these include serum proteins, fibrinogen/serum amyloid A and IgG measurement. This will allow determination of any evidence of failure of passive transfer of immunity, neonatal isoerythrolysis, septicemia, prematurity, etc. Submission of blood for all these tests is an optional practice – if money is restricted the single most important test is for serum IgG levels (see p. 394). 5. Assessment of passive transfer of immunity (see p. 9): this is important because of the total reliance that the foal places on passively transferred immunity for the first 4–9 weeks of life. The methods available are described on page 394 but include: (b) globulin estimation (by subtraction of albumin from total serum protein) (d) zinc sulfate turbidity test (g) concentration immunoassay technology (CITE) (i) radial-immunodiffusion (SRID) 1. to protect the foal and weanling against specific high risk infectious diseases that affect this age group and have the potential to cause significant disease, either directly or by predisposing to other secondary infections, or 2. to initiate primary immunization to protect against disease later in life. • booster vaccinate the dam before foaling to maximize uniformity of passive transfer • ensure good passive transfer of maternal antibodies • introduce management practices to reduce exposure to the infectious agent • vaccinate the foal if risk continues beyond first few months of life. • vaccinate the dam before foaling to maximize uniformity of passive transfer • ensure good passive transfer of maternal antibodies • start foal vaccination after the risk of maternal antibody interference is no longer present in most foals, as long as it has been ascertained that vaccination in the face of maternal antibodies does not impair the ability of foals to respond when vaccinated later in life • introduce management practices to reduce exposure to the infectious agent while primary vaccination is being completed • use three or more doses of vaccine in the primary series to improve the chances that foals that did not respond to earlier doses will respond when given additional doses later. Protection against tetanus appears to be mediated entirely by circulating antibodies and these antibodies are transferred well via colostrum.6 Limited and conflicting information is available in the literature regarding the potential for maternal antibody interference with vaccination. Based on available published results, primary vaccination of foals against tetanus is recommended at 4 to 6 months of age.5,7 Tetanus toxoid is considered to be a potent antigen, and it has been widely accepted that concurrent administration of tetanus toxoid and antitoxin at different sites does not interfere with the response to tetanus toxoid.8 Consequently, it has been assumed that maternal antibodies were unlikely to interfere with the response of foals to tetanus toxoid. However, recent studies indicate that the response of 3-month-old foals from vaccinated mares is substantially poorer than the response of 6-month-old foals and yearlings.9 In addition, these studies showed that levels of induced antitetanus antibodies were substantially higher after administration of a third dose of vaccine than after two doses of vaccine, even in older foals. Therefore, the following protocol would be recommended: Influenza specific antibodies of the IgG subisotypes are passively transferred to foals via colostrum and inhibit their response to inactivated influenza vaccine.9 Conclusive evidence has shown that these colostral antibodies declined with a half-life of approximately 30–38 days.10,11 These workers also demonstrated that the majority of foals from vaccinated mares did not respond to inactivated adjuvanted vaccines administered at 3 months of age, whereas a higher proportion of 6-month-old foals responded if given three doses of influenza vaccine in the primary course. In recent years, further studies have documented the failure of a high proportion of foals from vaccinated mares to respond serologically to inactivated influenza vaccines administered at less than 6 months of age.12,13 Another important finding was reported by Cullinane and co-workers14 who found that a substantial number of foals vaccinated at less than 6 months of age not only failed to respond serologically to doses of vaccine administered in the primary course but also failed to respond to as many as six doses of vaccine administered over the next year, suggesting that early vaccination in the presence of maternal antibody had induced immunotolerance to influenza vaccines. From these observations it is recommended that foals from vaccinated mares should not be vaccinated against influenza at less than 6 months of age and that three doses of vaccine are necessary in the primary series. Immunity following vaccination with conventional parenterally administered inactivated vaccines is short lived and is highly correlated with levels of circulating antibody directed against surface hemagglutinin antigens.15 With the possible exception of ISCOM vaccines, conventional vaccines have limited potential to induce cytotoxic T lymphocyte responses or nasal secretory IgA responses. • Maintain all horses on breeding farms on a program of booster vaccination against influenza at 4–6-month intervals. • Booster vaccinate mares 4 to 6 weeks before foaling. • Begin foal vaccination at 6 to 12 months of age using three or more doses in the primary series. • Booster vaccinate young horses at 3–4-month intervals until they are 2 years of age if risk of infection remains high. • Mature performance, show, and pleasure horses constantly exposed to potential infection should be booster vaccinated at 4–6-month intervals. Correlates for protection against EHV1 and EHV4 in foals and weanlings have been extensively investigated but are not yet clearly defined.16 No clear relationship exists between protection from EHV1 infection and levels of circulating antibody induced by vaccination or infection, but the duration and amount of virus shedding from the nasopharynx are reduced in animals with high levels of circulating antibody.16 As with other herpesviruses, mucosal immunity and cell-mediated responses probably play a role at least as important as circulating neutralizing antibodies in protection against EHV1 infection. Because EHV4 replication is largely confined to epithelial cells of the upper respiratory tract, it is likely that mucosal immunity is important in protection. Specific antibodies to both EHV1 and EHV4 are transferred in colostrum.17,18 Field studies with modified live EHV1 vaccines indicate that colostral antibodies exert a profound inhibitory effect on serological responses to vaccination up to at least 5 months of age,19 although a cytotoxic cellular immune response to both EHV1 and EHV4 was induced.20 Recent studies with different commercially available inactivated vaccines have shown that the majority of foals from EHV-vaccinated mares do not mount a detectable neutralizing antibody response to vaccines administered at 3 and 4 months of age, even when three doses are administered in the primary series.17,18 An increased proportion of foals responded when vaccinated with a three-dose series starting at 5 or 6 months of age, but still a substantial number failed to seroconvert.
ROUTINE MANAGEMENT AND CLINICAL EXAMINATION
ROUTINE MANAGEMENT OF THE NEWBORN AND NEONATAL FOAL
NEWBORN (0–24 HOURS)
Umbilical care
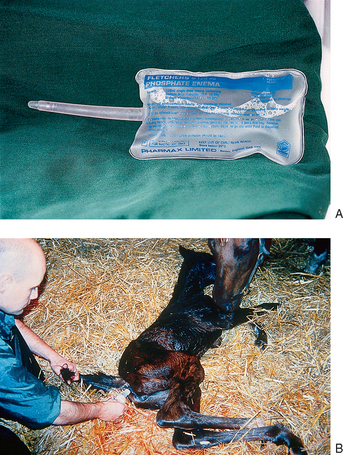
Prophylactic use of enemas
Supplementation of the newborn with colostrum
Weighing and examination of placenta for abnormalities (see p. 43)
OVER 1 WEEK
Parasite control strategies
Chemotherapeutic control
Managemental control
ROUTINE VETERINARY EXAMINATIONS AND PROCEDURES OF THE NEWBORN AND NEONATAL FOAL
Day 1 procedures
Day 2 procedures
FURTHER ROUTINE VETERINARY PROCEDURES IN THE OLDER FOAL
Vaccination recommendations for protecting foals
Recommendations for vaccination against specific diseases
Tetanus
Influenza
Equine herpesvirus1 and 4
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree