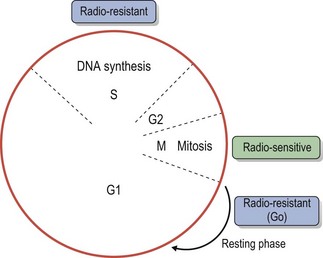
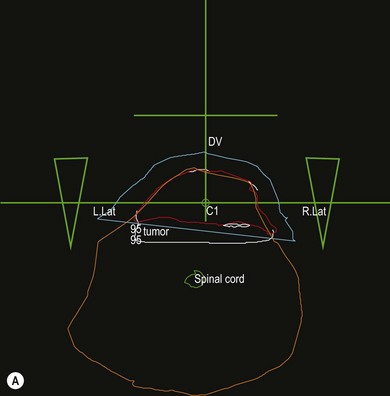
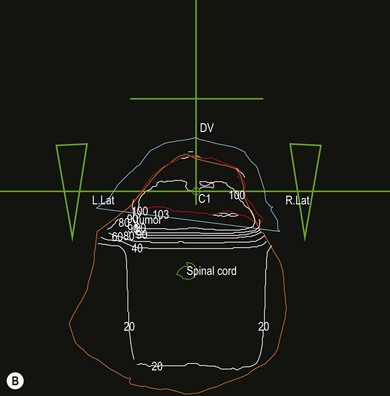
Chapter 15 The response of living cells and tissues to radiation depends upon the dose of radiation, how this is applied, and the radiosensitivity of the cell population. Radiosensitivity varies according to a number of factors (Box 15-1), one of the most important being the ‘growth fraction’ of the cell population. Small, rapidly growing tumors tend to respond more favorably to radiation than large, slowly growing tumors. Radiation treatment is unlikely to achieve more than a partial and temporary remission in the latter. One way to reduce normal tissue injury is to ‘fractionate’ the treatment. Following exposure to a single dose of radiation a number of changes occur in the exposed cell population, that are often referred to as the four ‘R’s’ of radiation (Box 15-2). A variety of ionizing radiations may be used for therapeutic purposes including There are essentially two techniques for the application of radiation to tumors: • Teletherapy: radiation is applied in the form of an external beam of X-rays, gamma-rays or electrons that are directed into the tumor • Brachytherapy: radioactive substances, which emit gamma or beta rays, may be applied to the surface of a tumor, implanted within the tumor or administered systemically to the patient. Each technique has advantages and disadvantages. Whilst external beam therapy is relatively safe for the operator, the equipment is expensive to purchase and maintain and multiple doses of radiation are required over a four to six week course of treatment. Brachytherapy often offers better localization of the radiation and permits the delivery of high doses of radiation to the tumor with minimal normal tissue toxicity. However, the implant and the implanted patient present a radiation hazard for the operator and any staff caring for the patient. Radioactive isotopes can only be used on licensed premises and strict local rules for handling the isotope and patient must be applied. Both techniques require careful planning in consultation with medical physicists to ensure the required dose of radiation is delivered to the tumor. Various devices exist for generating and delivering radiation to tissues (Box 15-3). With external beam radiation, the beam can be collimated to the area of the tumor and several treatment ports employed in order to reduce the amount of entry and exit beam radiation affecting the surrounding normal tissues. The prescription and planning of such treatment is facilitated by three-dimensional computerized treatment planning programs (Fig. 15-3). Multi-leaf collimators allow complex planning and shaping of the radiation field to the defined target volume. Intensity modulated radiotherapy (IMRT) allows multiple differently shaped photon beams to be effectively ‘painted’ onto the tumor, allowing higher doses of radiation to be delivered to the tumor with no increase in the dose delivered to normal tissue. More recent developments in radiotherapy include tomotherapy, which is a form of IMRT that uses a helical delivery system. Stereotactic radiosurgery describes a technique where multiple, highly targeted beams of radiation are delivered in large doses in fewer treatments (usually one to five). Radiosurgery may be delivered by a ‘gamma-knife’ which uses technology similar to IMRT, or a free standing ‘Cyberknife’. Tomotherapy and stereotactic radiosurgery have not been used widely in veterinary medicine to date, although there are some reports of radiosurgery in the treatment of brain tumors. Figure 15-3 Computer generated treatment plan for preoperative radiotherapy of an intrascapular feline injection site sarcoma (FISS). The use of three perpendicular beams (green lines) allows the radiation to be ‘focused’ into the tumor volume (red line), whilst sparing the surrounding normal tissues to a degree. The white lines are the isodose levels predicted by the computer program. The blue line is the tissue equivalent bolus used to ensure that superficial tumor receives the required dose of radiation. The green triangles are ‘wedges’ used to reduce the amount of radiation dorsally, where the tumor is narrower. The orange line represents the whole cross-section of the cat.
Radiation therapy
The basic principles of radiation physics and biology
Radiation biology
Sources of radiation used for therapy
External beam methods
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiation therapy