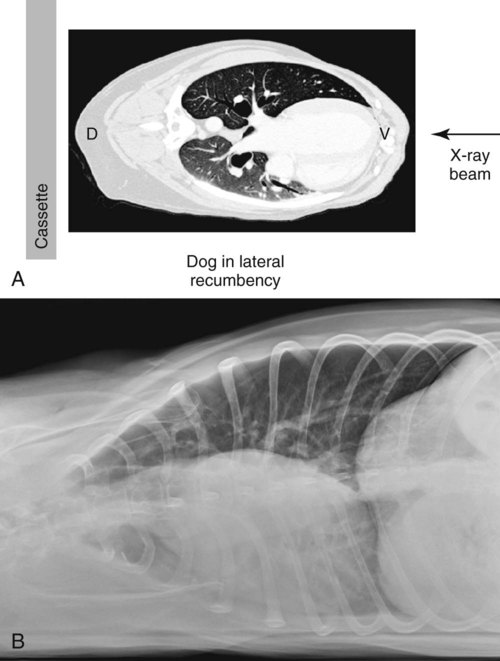
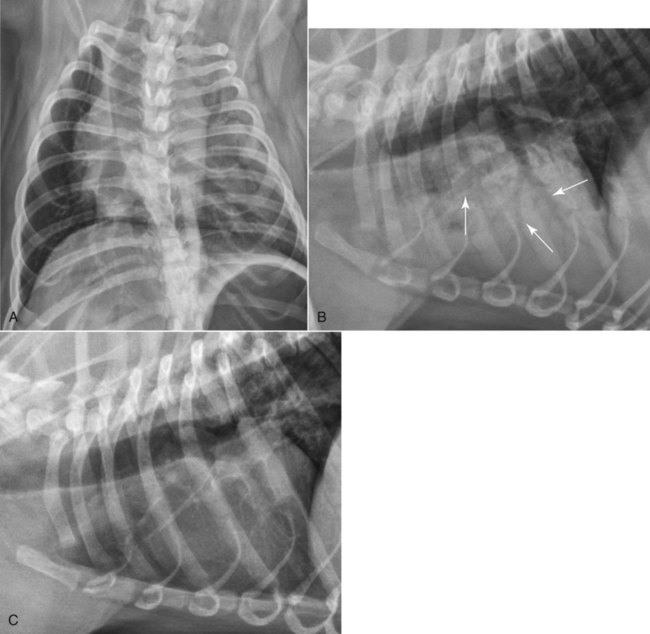
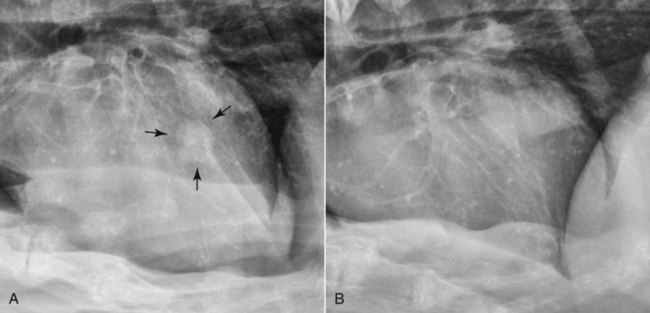
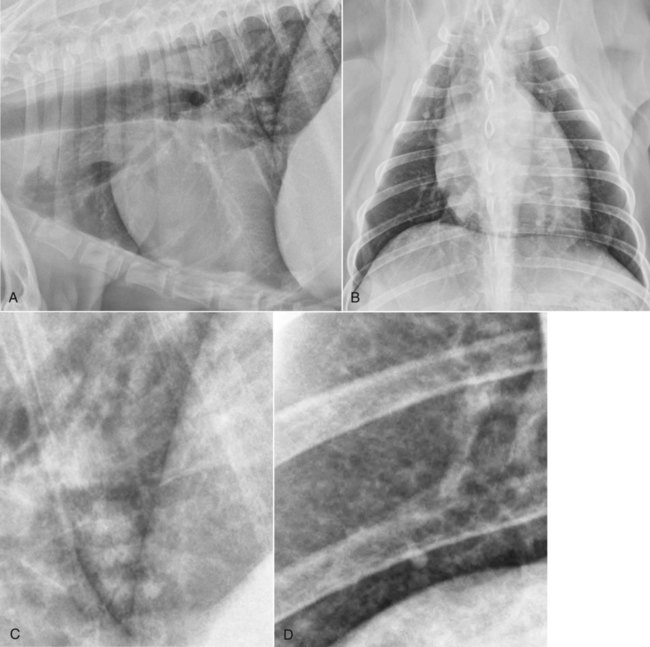
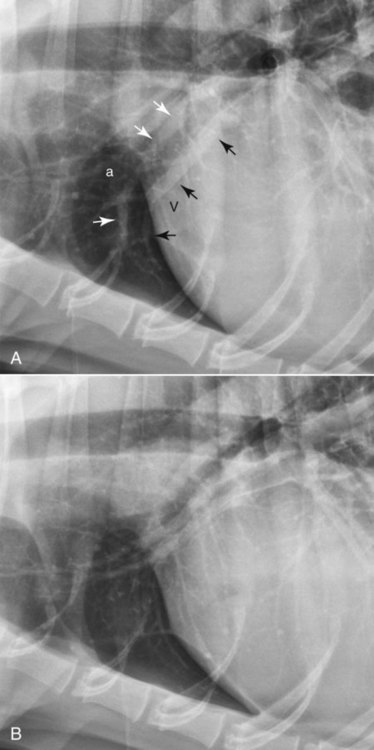
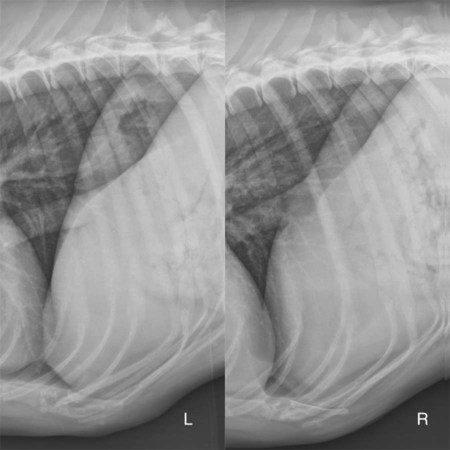
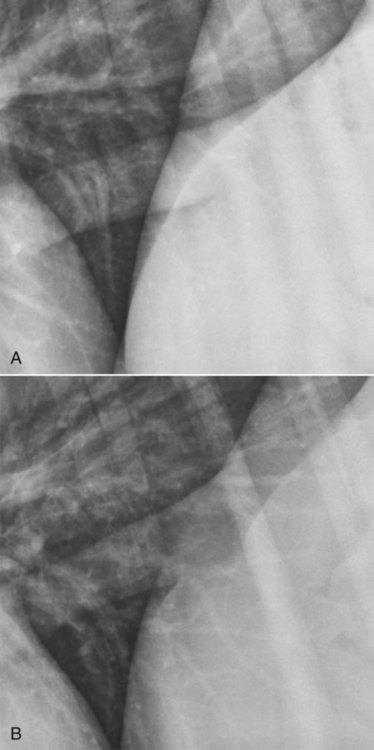
The naming of lateral thoracic radiographs made with the patient recumbent and a vertically directed x-ray beam, as commonly done in dogs and cats, violates the point-of-entrance to point-of-exit nomenclature system described in Chapter 5. In that system, a lateral view made with the dog or cat in left recumbency would be termed a right-left view because the x-ray beam strikes the right aspect of the thorax and exits the left aspect of the thorax. But, for the thorax, the terminology for lateral projections has been abbreviated to describe the side of the patient lying on the x-ray table. Thus, for example, a thoracic radiograph acquired with the dog or cat lying on the left side would be termed a left lateral view. When an animal is in lateral recumbency, as for a lateral radiographic examination, the dependent lung collapses from (1) the effects of the heart compressing the lung, (2) reduced movement of the dependent thoracic cage because of compression, and (3) cranial excursion of the dependent portion of the diaphragm. This collapse occurs in awake, sedated, and anesthetized dogs and cats relatively shortly after being placed in lateral recumbency. The magnitude of this collapse, which is related directly to the body mass of the patient, can be appreciated by making a radiograph of the thorax with the dog in lateral recumbency and using a horizontally directed x-ray beam. Such a projection would be termed a right (or left) recumbent horizontal-beam VD. The configuration for acquiring such a radiograph and an example are provided (Fig. 25-1). The amount of recumbency-associated atelectasis that occurs is striking. This atelectasis cannot be visualized directly in a conventional lateral radiograph made with a vertically directed x-ray beam because the aerated nondependent lung is superimposed on the collapsed dependent lung. Nevertheless, the increased opacity of the dependent lung contributes to an appearance of overall increased lung opacity in lateral radiographs that is misdiagnosed commonly as disease. In addition to being misdiagnosed as lung disease, recumbent atelectasis is important because the increased radiographic opacity of the collapsed lung causes border effacement, or silhouetting, of any soft tissue lesion in the dependent lung, rendering it inconspicuous in the radiograph.1 This phenomenon results commonly in lesions in the dependent lung not being visible radiographically in the lateral view (Fig. 25-2). The most significant aspect of this phenomenon is in the situation where the lesion is small and is not visible in the VD or DV view, such as commonly occurs with a lung nodule or small mass. If only one lateral view is made of such patients, and the lesion happens to be in the dependent lung and also in a region where it is not visible in the VD or DV radiograph, the lesion will be missed (Fig. 25-3). The collapse of the dependent lung is the main reason why both the left lateral and right lateral views should be included in every routine thoracic radiographic examination. If only one lateral view is obtained, a significant number of patients will be diagnosed incorrectly.2 Given the amount of dependent atelectasis that occurs in lateral recumbency, it is not surprising that the overall radiographic opacity of the lung field will be increased in lateral versus VD or DV radiographs. Overinterpreting this increased opacity as lung disease is a common mistake (Fig. 25-4). If lung disease is suspected from one or both lateral views, it is critical that this be confirmed in the VD or DV view to rule out that the suspected lung disease is caused simply by atelectasis. Assessing the absolute and relative size of pulmonary vessels is an important process of thoracic radiographic interpretation.3 The pulmonary artery and vein in the right cranial lobe are used commonly as a basis for assessing the pulmonary circulation. It is important to be able to identify these two vessels specifically and to be able to compare the size of the right cranial lobe pulmonary artery to the size of the right cranial lobe pulmonary vein without having other vessels superimposed. The pulmonary vessels in the right cranial lung lobe are more conspicuous in a left lateral than in a right lateral radiograph (Fig. 25-5). This is caused mainly by the dorsal displacement of the right cranial lobe that occurs when the patient is in right lateral recumbency resulting in the right cranial lobar vessels being superimposed on the left cranial lobar vessels. In the left lateral view, the two dorsal crura of the diaphragm deviate from each other, whereas in the right lateral view they are more parallel (Fig. 25-6). The diaphragmatic hiatus for the caudal vena cava is located slightly to the right of midline. In the right lateral view the dependent right crus will be cranial to the left crus because of pressure from abdominal contents, and therefore the caudal vena cava will silhouette, or merge, with the more cranial crus. In the left lateral view, the left crus will be cranial to the right crus, and the caudal vena cava will be superimposed on the left crus before silhouetting, or merging, with the more caudally located right crus (Fig. 25-7). The appearance of the junction of the caudal vena cava with the diaphragm can be used as a way to distinguish a left lateral from a right lateral radiograph if an external marking system has not been used, but this is not 100% reliable because sometimes the left crus will be cranial to the right crus in the right lateral view, and vice versa.
Principles of Radiographic Interpretation of the Thorax
Nomenclature
Positioning: Dog and Cat
Lateral Views
Atelectasis
Cranial Lobe Vessels
Diaphragm
Principles of Radiographic Interpretation of the Thorax