Chapter 129 Peripheral Nerve Disorders
ANATOMY AND PHYSIOLOGY
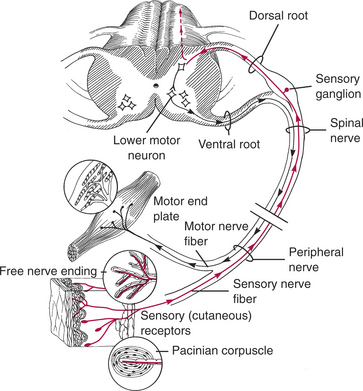
The peripheral nervous system (PNS) is composed of 12 pairs of cranial nerves (see Chapters 125 and 126) and 36 pairs of spinal nerves that arise from the spinal cord. Spinal nerve fibers give rise to the peripheral nerves, which usually are composed of both sensory and motor fibers. Sensory nerve fibers are activated by peripheral receptors (Fig. 129-1). Impulses are transmitted up the peripheral nerve to the spinal cord. Some disorders affect only the sensory nerve fibers or ganglia, causing clinical signs such as hyperesthesia and analgesia, proprioceptive deficits, and self-mutilation (Table 129-1). In many cases sensory losses may be difficult to detect.
Motor or efferent nerve fibers arise from nerve cell bodies in the gray matter of the spinal cord. They carry information from the central nervous system (CNS) to the striated muscles (see Fig. 129-1). Motor deficits, characterized by limb weakness, muscle atrophy, and reduced spinal reflexes, occur with injury to any of the following: lower motor neuron in the gray matter of the spinal cord, ventral nerve root, spinal nerve, peripheral motor nerves, neuromuscular junction, and muscle (see Fig. 129-1). Disorders of the neuromuscular junction and muscle are discussed in Chapter 130.
CLINICAL SIGNS
Motor nerve disorders generally cause weakness and muscle atrophy. Sensory nerve disorders cause hyperesthesia or anesthesia, self-mutilation, and other abnormalities (see Table 129-1). The clinical signs of motor nerve disorders are similar to those of muscle disorders and can be distinguished using muscle enzyme determinations and muscle and nerve biopsies (see Chapter 130).
Many common peripheral nerve disorders are manifested as one of the following clinical problems: acute flaccid tetraplegia, chronic progressive tetraparesis, monoparesis or monoplegia, and sensory disturbances (Table 129-2).
Table 129-2 DIFFERENTIAL DIAGNOSIS BASED ON CLINICAL SIGNS OF NEUROPATHY
| Problem | Differential Diagnosis |
|---|---|
| Monoparesis or Monoplegia | |
| Acute onset | Trauma to nerve root or peripheral nerve |
| Fibrocartilaginous infarct | |
| Intervertebral disc herniation to lateral side | |
| Chronic onset | Tumor of nerve root or peripheral nerve |
| Intervertebral disc herniation to lateral side | |
| Joint disease | |
| Acute Flaccid Tetraplegia | |
| Acute polyradiculoneuritis (coonhound paralysis) | |
| Tick paralysis (see Chapter 130) | |
| Botulism (see Chapter 130) | |
| Myasthenia gravis crisis (see Chapter 130) | |
| Post-vaccinal polyneuropathy | |
| Acute idiopathic polyneuropathy | |
| Protozoal neuritis/myositis | |
| Chronic Progressive Tetraparesis | |
| Immature | Globoid cell leukodystrophy |
| Giant axonal neuropathy (German shepherds) | |
| Progressive axonopathy (boxers) | |
| Hypertrophic neuropathy (Tibetan mastiffs) | |
| Motor neuron diseases (Brittany spaniels, pointers, rottweilers) | |
| Mature | Chronic relapsing polyradiculoneuritis |
| Distal denervating disease | |
| Distal polyneuropathy (Doberman pinschers) | |
| Distal symmetrical polyneuropathy | |
| Metabolic neuropathy | |
| Neoplastic and paraneoplastic neuropathy | |
| Toxic neuropathy | |
| Nutritional neuropathy | |
| Various myopathies | |
| Sensory Disturbances | |
| Immature | Acral mutilation in pointers |
| Sensory neuropathy (longhaired dachshunds) | |
| Mature | Sensory neuropathy (ganglioradiculoneuritis) |
PRINCIPLES OF DIAGNOSIS
History and Physical Examination
Laboratory Evaluation
Electrodiagnostics
Muscle and Nerve Biopsy
PRINCIPLES OF TREATMENT
SPECIFIC PERIPHERAL NERVE DISORDERS
Anomalous, Inherited, and Congenital Disorders
Globoid Cell Leukodystrophy
Glycogen Storage Disease in Norwegian Forest Cats
Other Storage Diseases Affecting Peripheral Nerves
See Chapter 126 for a discussion of other lysosomal storage diseases affecting the nervous system.
Hyperoxaluria Type 2 in Domestic Shorthaired Cats
Giant Axonal Neuropathy in German Shepherds (Alsatians)
Hypertrophic Neuropathy in Tibetan Mastiffs
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree