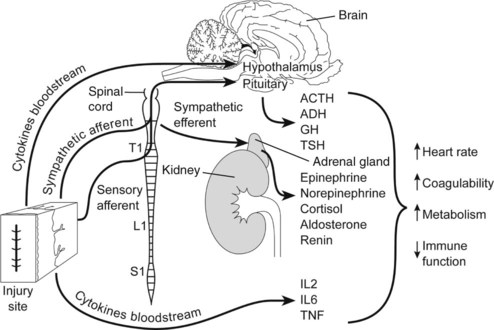
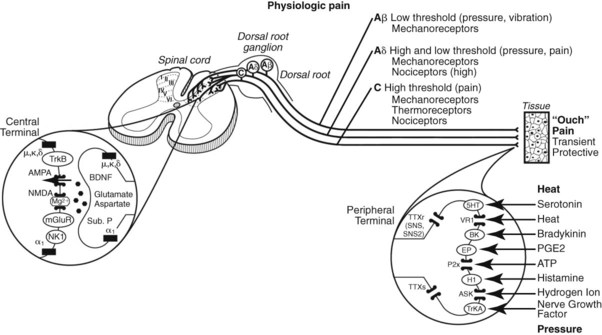
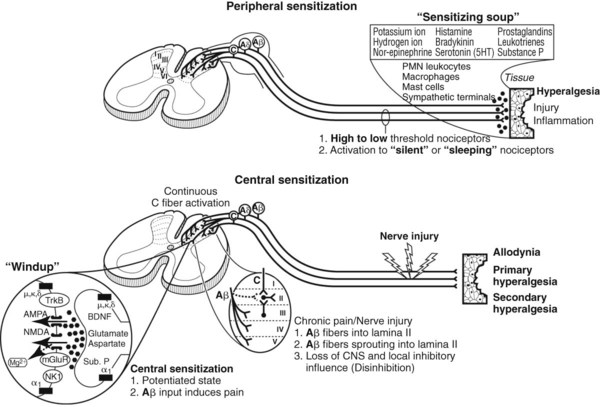
18 The definition, recognition, quantitation, and treatment of pain have become central issues in veterinary practice. This statement is particularly relevant when considering the treatment of perioperative pain. Untreated acute pain (e.g., from physical trauma, surgery) produces physiologic and emotional changes in animals that predispose them to adaptive pain states, or if untreated or severe, the potential for maladaptive (pathologic) pain states. Providing pain relief is as important as choosing the proper sedative, muscle relaxant, and injectable or inhalant anesthetic. Apprehension and stress, produced by fear, can initiate a variety of potentially deleterious neurohumoral reactions (stress response) that sensitize both the peripheral and central nervous systems to noxious stimuli (Fig. 18-1). Understanding pain pathways, the mechanism(s) responsible for pain and the action of analgesic therapies provide a rational approach to pain therapy. Recognizing and anticipating pain behaviors facilitates its prevention (preemptive analgesia) and early treatment. Acute pain: the sudden onset of pain that can be severe but disappears when the stimulus is removed or in a relatively short time; disappears with healing, and tends to be self-limiting Adaptive pain: pain evoked from actual or impending tissue damage and is protective. Pain induced by environmental stimuli that limits or prevents physical contact or movement and promotes healing Allodynia: Pain evoked by a stimulus that does not normally cause pain Analgesia: Loss of sensitivity to pain Analgesic: Any method or drug that relieves pain Breakthrough pain: A transient flare-up of pain in the chronic pain setting; can occur even when pain is being controlled by analgesic therapies Cancer pain: Pain that can be acute, chronic, or intermittent and is related to the disease itself or to the treatment Central sensitization: An increase in nerve excitability and responsiveness in the central nervous system, particularly the spinal cord (Fig. 18-2) Chronic pain: Pain that lasts several weeks to months and persists beyond the expected healing time Deep pain: Pain originating from tendons, joints, muscles, and periosteum; it is not unusual for deep pain to cause a drop in blood pressure, a slowing of the pulse, and nausea, vomiting, and sweating; can cause reflex cramping of nearby skeletal muscles Distress: (1) A state produced when the biologic cost of stress negatively affects biologic functions critical to the animal’s well-being; (2) to cause pain or suffering or to make miserable Epidural: The space above the dura mater Hyperalgesia: An increased or exaggerated response to a stimulus that is normally painful (a heightened sense of pain) either at the site of injury (primary) or in surrounding undamaged tissue (secondary or extraterritorial). Nociceptors (pain receptors) respond to painful stimuli more vigorously and at a lower stimulus intensity Hyperesthesia: Increased sensitivity to stimulation Hyperpathia: A painful syndrome characterized by an increased reaction to a stimulus, especially if it is repetitive Hypoalgesia: Decreased sensitivity to pain Hypoesthesia: Decreased sensitivity to stimulation Institutional Animal Care and Use Committee: A committee whose existence is required by the U.S. Department of Agriculture and the U.S. Department of Health and Human Services at institutions conducting research on animals; consists of veterinarians, practicing scientists, nonscientists, and individuals not affiliated with the institution; responsible for evaluating the institutional animal care and use programs and making recommendations to institution administrators; ultimately responsible for approving or disapproving the use of animals in research at the institution on a case-by-case basis Interventional pain management: Action taken to prevent or alter the body’s production or transmission of pain signals to the brain. Local anesthesia: Analgesia generally limited to a specific area where the anesthetic drug is applied or injected Major surgery: Any surgical intervention that penetrates and exposes a body cavity; any procedure that has the potential for inducing permanent physical or physiologic impairment; any procedure associated with orthopedics or extensive tissue dissection or transection Maladaptive pain: Pain that tends to be out of all proportion to actual tissue damage and which persists long after the tissues have healed so that the pain becomes the problem Minor surgery: Any surgical intervention that produces minimal impairment of physical or physiologic function (e.g., laparoscopy, superficial vascular cutdown, percutaneous biopsy) Multimodal analgesia: The use of multiple drugs that act by different mechanisms to produce analgesia with the goal of producing additive or synergistic (supra-additive) effects. Multimodal drug combinations have the potential to produce greater efficacy at reduced individual drug dosages, thereby increasing safety Myofascial pain: A syndrome of focal pain in a muscle or related tissues, associated with stiffness, muscle spasm, and decreased range of motion Neuralgia: Pain exhibiting periodic intensification, which extends along the course of one or more nerves Neuroleptanalgesia: Hypnosis and analgesia produced by the combination of a neuroleptic drug (i.e., tranquilizer) and an analgesic drug Neuropathic pain: Pain that originates from injury or after injury of the peripheral or central nervous system (CNS), possibly associated with motor, sensory, or autonomic deficits Neuroplasticity: adaptive changes in the central or peripheral nervous system caused by changes in the environment (e.g., infection, inflammation, trauma) Nociception: The transduction, conduction, and CNS processing of nerve electrical signals generated by the stimulation of nociceptors (pain receptors). The physiologic process that leads to the perception of pain Opioid: A pain-relieving drug that is related naturally or synthetically to morphine Pain: An aversive sensation and feeling associated with actual or potential tissue damage Pain threshold: The least stimulus that produces pain Pain tolerance level: The greatest level of pain that can be tolerated Pathologic pain: A disease state caused by damage to the nervous system (neuropathic) or by its abnormal function (dysfunctional). Pathological pain is maladaptive and usually includes peripheral sensitization, central sensitization, and hypersensitivity resulting in allodynia Perception of pain: Only humans report and demand treatment of pain; pain in animals must be inferred by the observation of deviations from normal behavior or the development of abnormal behavior; pain may manifest itself as a limp or altered gait; withdrawal of an injured part; awkward, abnormal postures; a worried or distressed expression; looking at, licking, scratching, or kicking at the site of perceived pain; these and similar signs are the only clues a veterinarian can use to diagnose the presence and magnitude of pain; it seems likely that the presence of pain in animals is underdiagnosed and, when diagnosed, that its magnitude is underestimated Perioperative: around (the time of) surgery; the period of time extending from when the animal enters the hospital for surgery until the time the animal is discharged Peripheral sensitization: An increase in the activity, excitability, and responsiveness of peripheral nerve terminals (see Fig. 18-2) Physiologic pain: The normal response (nociceptive pain; “ouch” pain) to a noxious stimulus that produces protective mechanisms causing the animal to minimize tissue damage (fight-or-flight response) or to avoid contact with external stimuli during a reparative phase (Fig. 18-3) Preemptive analgesia: The administration of analgesic therapy before painful stimulation to prevent sensitization of neurons, or windup, with the goal of improving analgesia Projected pain: An error in the localization of pain; occurs with superficial pain, which is normally quite accurately located; injury to a nerve containing pain pathways causes a phantom pain to be projected into the uninjured area at the origin of the pain fibers Referred pain: Pain originating in one part of the body but perceived as occurring in another; occurs as the result of the synapses in the spinal cord of visceral pain fibers with pain fibers from the skin Regional anesthesia: The loss of sensation in part of the body caused by interruption of the sensory nerves that conduct impulses from that region of the body Sedation: CNS depression in which the animal is awake but calm and generally uninterested in its surroundings; a term often used interchangeably with tranquilization; sufficient stimulation will arouse the animal Somatic pain: Pain that originates from damage to bones, joint, muscle, or skin and is described by humans as localized, constant, sharp, aching, and throbbing Stoic: Indifferent to pain or pleasure Stress: The biologic responses of an animal to cope with a disruption or threat to homeostasis. A stressor is a physical, chemical, or emotional factor (e.g., pain, trauma, fear) to which an individual fails to make a satisfactory adaptation and which causes physiologic tensions that may contribute to the development of disease Subarachnoid: The space above the pia mater and below the arachnoid mater in which cerebrospinal fluid is found. A subarachnoid injection is also referred to as a spinal Superficial or cutaneous pain: Originating on an outer surface (skin) and generally well localized; superficial pain may be sharp or acute or it may be chronic, burning, or aching; may cause an increase in pulse rate and blood pressure Surgery: The act of incising living tissue; an operative procedure; the room or facility where an operative procedure is performed Surgical facility: A group of interrelated rooms specifically designed for conducting surgery and for preoperative and postoperative functions associated with conducting surgery in animals Survival/recovery surgery: A surgical procedure from which animals recover from the effects of general anesthesia and become conscious Sympathetic mediated pain: A syndrome in which there is abnormal sympathetic nervous system activity, causing a severe debilitation and often associated with tenderness to a light touch Tolerance: A shortened duration and decreased intensity of drug effect and/or a marked elevation in the average dose required to achieve a given effect Tranquilization, ataraxia, neurolepsis: State of tranquility and calmness in which the animal is relaxed, reluctant to move, awake, unconcerned with its surroundings, and potentially indifferent to minor pain; sufficient stimulation will arouse the animal Visceral pain: Originating from internal organs, visceral pain is poorly localized; small injuries may not cause pain, but diffuse foci can produce extremely severe pain; pulling and twisting of viscera, mesenteries, and ligaments can cause pain in an anesthetized animal; visceral pain can be perceived as a pain on the body surface; this error in pain localization is called referred pain; if the visceral involvement results in an inflammation that extends to an area of parietal peritoneum, pleura, or pericardium, pain fibers from these areas are also stimulated; pain fibers in the parietal peritoneum or pleura are innervated like the skin and are capable of sensing acute, highly localized pain referring to the corresponding area on the surface of the body; visceral pain can also produce significant sympathetic activation (e.g., tachycardia, hypertension, tachypnea) and skeletal muscle spasm of the abdominal wall over the affected area; usually involves the parietal peritoneum Windup: Temporal summation of painful stimuli in the spinal cord. Mediated by C-fibers and responsible for “second” or delayed pain (see Fig. 18-2) II Physiology of pain and pain pathways 2. Thermosensitive; involves temperature change B Peripheral nerves (Table 18-1) TABLE 18-1 Injectable Analgesic Drugs and Their Mechanism of Action CNS, Central nervous system.
Pain and Pain Therapy
Overview
General Considerations
Drug
Mechanism of Action
Opioids (morphine, fentanyl, methadone, meperidine, hydromorphone, oxymorphone, buprenorphine, butorphanol)
Combine with opioid receptors to produce sedation, analgesia, and euphoria
α2-Agonists (xylazine, detomidine, medetomidine, dexmedetomidine, romifidine)
Combine with α2-receptors to produce sedation, muscle relaxation, and analgesia
Nonsteroidal antiinflammatory drugs (flunixin meglumine, phenylbutazone, aspirin, carprofen, ketoprofen, etodolac, meloxicam, deracoxib, firocoxib, robenacoxib, piroxicam)
Act centrally (CNS) on the hypothalamus; antiinflammatory and analgesic activity mediated by peripheral inhibition of prostaglandins
Local anesthetics (lidocaine, mepivacaine, bupivacaine, ropivacaine)
Block nerve transmission of electrical impulses
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree