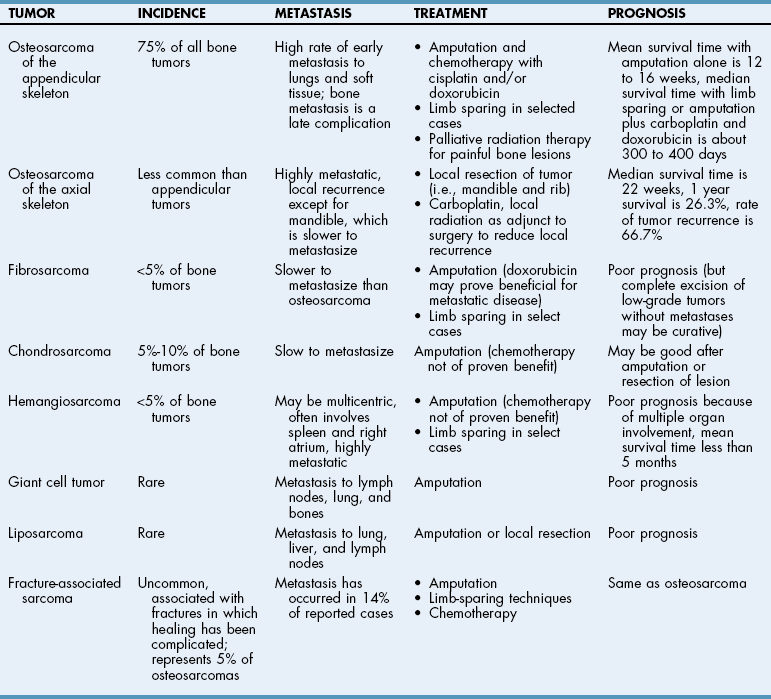
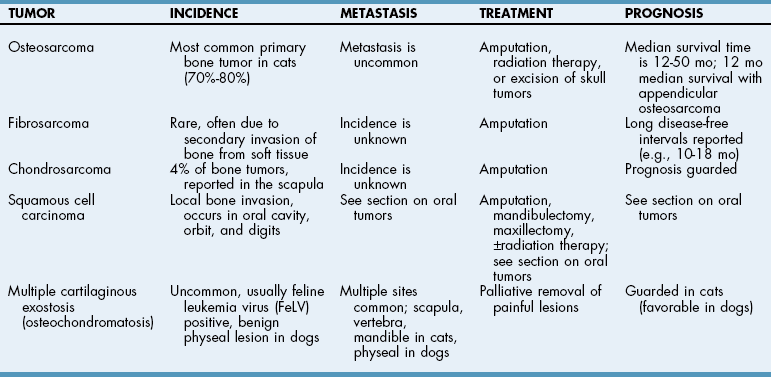
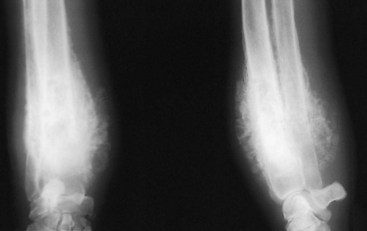
Chapter 36 Hypertrophic Osteopathy Hypertrophic osteopathy can affect all four limbs. It can be a paraneoplastic syndrome (e.g., primary and metastatic lung tumors, esophageal carcinoma, rhabdomyosarcoma of the bladder, anal sac adenocarcinoma, renal transitional cell carcinoma, nephroblastoma), or it may be associated with other diseases (e.g., granulomatous lesions, chronic megaesophagus, patent ductus arteriosus, bacterial endocarditis, heartworm disease) (Hammond et al, 2009). The precise pathophysiology of this disease is unknown. Alterations in pulmonary function have been suggested to increase peripheral blood flow, resulting in connective tissue congestion. The increased peripheral blood flow is thought to be neurally mediated. The periosteum responds by forming new bone on the cortical surfaces of the metacarpal, metatarsal, and long bones. This new bone may be diffuse or nodular. Histologically, the affected area is made of bands of new cortical bone that contain small, fibrous marrow spaces. Radiographs of the limbs reveal a uniform periosteal proliferation, which is seen initially on the phalanges and metacarpal and metatarsal bones (Fig. 36-1). As the disease progresses, periosteal proliferation progresses proximally (i.e., radius/ulna and tibia/fibula). Articular surfaces of long bones usually are spared and appear normal. Radiographic signs of panosteitis are progressive. Radiographs of affected limbs are often normal during early stages, and clinical signs may precede radiographic abnormalities by up to 10 days. If clinical signs are consistent with panosteitis but radiographs are normal, radiographs should be repeated in 7 to 10 days. Nuclear scintigraphy is a more sensitive diagnostic test of panosteitis than radiography. The earliest radiographic signs include widening of the nutrient foramen and blurring and accentuation of trabecular patterns (which often are difficult to identify, except in retrospect); these are followed by the appearance of radio-opaque, patchy, or mottled bone within medullary canals (Fig. 36-2). Eventually, remodeling of medullary canals occurs, and cortical thickening may remain as the only residual finding. The disease is self-limiting, so treatment consists of controlling pain. Nonsteroidal anti-inflammatory drugs (NSAIDs) (see Table 34-4 on p. 1221) usually are administered during acute episodes of lameness. Exercise restriction is recommended when the animal is lame. Owners should be warned of the likelihood of recurrence, but the long-term prognosis is excellent for complete recovery. The cause of craniomandibular osteopathy is unknown. It is most often recognized in West Highland White Terriers, Cairn Terriers, and Scottish Terriers. A genetic predisposition is suspected in many breeds; in West Highland White Terriers, it is thought to have an autosomal recessive inheritance pattern. A similar syndrome (calvarial hyperostotic syndrome) has been reported in Bullmastiffs (McConnell et al, 2006). Craniomandibular osteopathy has been associated with canine leukocyte adhesion deficiency in Irish Setters. A link to canine distemper virus has been postulated but is not supported by epidemiologic studies. Skull radiographs reveal increased irregular bone density of the caudal mandibles (84% of cases), including tympanic bullae (51% of cases) (Fig. 36-3). Sometimes lesions are confined to the mandibles (33% of cases), and occasionally they are confined to the base of the skull (13% of cases). The calvarium may be thickened. As dogs reach maturity, the edges of the new bone become smooth and affected areas shrink. Analgesics (see Table 34-4 on p. 1221) should be given to control pain until the animal reaches maturity. Severely debilitated animals that cannot open their mouths enough to eat solid foods require oral fluid nourishment or a feeding tube. Although antibiotics and corticosteroids are often administered during febrile episodes, they will not alter disease progression. Hypertrophic Osteodystrophy The cause of hypertrophic osteodystrophy is unknown. Proposed causative factors include vitamin C deficiency, oversupplementation of dietary calcium, and infectious organisms. A link to canine distemper virus has been postulated but is not supported by epidemiologic studies. Experimentally, vaccination protocols have been associated with the development of hypertrophic osteodystrophy in Weimaraner puppies; however, no specific vaccine has been identified (Crumlish et al, 2006). The pathogenesis is obscure, but an apparent disturbance of metaphyseal blood supply leads to changes in the physis and adjacent metaphyseal bone, causing delayed ossification of the physeal hypertrophic zone. The acute phase lasts about 7 to 10 days. Affected animals show signs ranging from mild lameness to anorexia, pyrexia, lethargy, severe lameness, refusal to rise, and generalized weight loss. Clinical signs may wax and wane. Radiographs of affected long bones reveal an irregular radiolucent zone in the metaphysis, parallel and proximal to the physis. This gives the appearance of a double physeal line. Metaphyseal flaring with increased bone opacity occurs because of periosteal proliferation in later stages of the disease. This reaction subsides with time but may leave a permanently widened metaphysis (Fig. 36-4). This condition should be differentiated from septic arthritis, septic physitis, and panosteitis. Analgesics should be administered to control pain (see Table 34-4 on p. 1221). Occasionally, severely debilitated animals require fluid support. Corticosteroids, antibiotics, and vitamin C have been administered but have not proved effective in shortening the course or severity of the disease. Bacteremia should be ruled out before corticosteroids are administered. Bone Neoplasia Osteosarcoma is the most common primary bone neoplasm in dogs, accounting for approximately 85% of skeletal malignancies; 75% of osteosarcomas originate in the appendicular skeleton (Tables 36-1 and 36-2). The front limbs are affected twice as often as the rear limbs. In dogs less than 15 kg, 60% of tumors originate in the axial skeleton. (Withrow and Vail, 2007). Primary osteosarcoma of extraskeletal tissues is rare but has been reported (mammary, subcutaneous, spleen) (Withrow and Vail, 2007). A genetic cause of osteosarcoma appears likely based on experimental and clinical studies (Withrow and Vail, 2007). Osteosarcoma has been associated with fractures and metallic implants and may also occur within radiation fields following radiation treatment of soft tissue sarcomas. Osteosarcoma is the most common tumor of the axial skeleton. Of 116 axial osteosarcomas evaluated, the most common sites of occurrence were the mandible (27%), maxilla (22%), spine (15%), cranium (14%), ribs (10%), nasal cavity and paranasal sinuses (9%), and pelvis (6%) (Withrow and Vail, 2007). Because osteosarcoma is the most commonly diagnosed bone tumor, it is used as the model for evaluation, diagnosis, treatment, and prognosis of bone tumors in this section. Although the work-up needed to diagnose neoplasia is similar for all bone tumors, treatment and prognosis vary depending on tumor type (see Tables 36-1 and 36-2). Osteosarcoma accounts for 70% to 80% of primary bone tumors in cats. Osteosarcoma occurs more commonly in the hindlimbs of cats and may have a lower rate of metastasis than in dogs. Cats rarely have evidence of metastasis at presentation (Withrow and Vail, 2007). Multiple cartilaginous exostosis (MCE) is a histologically benign disease of cats that occurs after skeletal maturity, in contrast to dogs, in which the disease occurs before growth plate closure. MCE is likely of viral origin in cats, most of which test positive for feline leukemia virus (FeLV) antigenemia. Large and giant breed dogs have the greatest incidence of appendicular bone neoplasia. The median age of dogs with osteosarcoma is 7 years. A small early peak is seen in dogs 18 to 24 months of age. Large size is a greater determinant of risk than breed, although Greyhounds, Rottweilers, and Great Danes have been shown to be at increased risk (Rosenberger et al, 2007). Males may be slightly more commonly affected than females (1.1 to 1.5 : 1). Primary bone tumors of the axial skeleton are more common than appendicular tumors in small breed dogs. The median age of affected animals is 8.7 years. The mean age of osteosarcoma in cats is 8 to 10 years. No apparent breed or sex predilection has been identified in either species. Radiographs of affected bones and the thorax should be evaluated. Radiographic signs of osteosarcoma include cortical and trabecular bone lysis, periosteal bone proliferation, and soft tissue swelling (Fig. 36-5). Thoracic radiographs should include a dorsoventral or ventrodorsal view and both lateral recumbent views (i.e., right and left lateral views). These radiographs should be carefully evaluated for evidence of tumor metastasis. Alternatively, contrast-enhanced computed tomography (CT) of the thorax can replace survey radiographs; CT is more sensitive than radiography in detecting small metastatic lesions. Although radiographic signs associated with primary bone neoplasia cannot be differentiated from those associated with fungal osteomyelitis, coupling radiographic signs with signalment and history can help determine whether neoplasia should be considered likely. Ultimately, histopathology is necessary for confirmation. If limb-sparing surgery is being considered, magnetic resonance imaging (MRI) should be used to determine the extent of the disease.
Other Diseases of Bones and Joints
General Considerations and Clinically Relevant Pathophysiology
Diagnosis
Diagnostic Imaging
Panosteitis
Diagnosis
Diagnostic Imaging
Medical Treatment
Craniomandibular Osteopathy
General Considerations and Clinically Relevant Pathophysiology
Diagnosis
Diagnostic Imaging
Medical Management
General Considerations and Clinically Relevant Pathophysiology
Diagnosis
Diagnostic Imaging
Differential Diagnosis
Medical Management
General Considerations and Clinically Relevant Pathophysiology
Diagnosis
Signalment.
Diagnostic Imaging
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Other Diseases of Bones and Joints