12 Occupational Health of Animal Workers
Key Points for Clinicians and Public Health Professionals
Public Health Professionals
Human Health Care Providers
Veterinary Clinicians
TYPES OF ANIMAL WORKERS
More than 2 million people in the United States are engaged in a wide range of occupational activities that involve animals.1 These include approximately 750,000 persons involved with livestock confinement; 500,000 involved with dairy farming2; 200,000 workers employed in animal care and services as kennel attendants, groomers, stable hands, zoo keepers, and animal trainers3; and 125,000 researchers and animal handlers involved with laboratory animal research.4 Globally, as much as 49% of the world’s population is estimated to be involved in agriculture, which often involves animal husbandry and animal-associated health risks.5 Some of these workers are formally employed in full-time positions in animal-related care and may receive preventive health services (such as described in this chapter) through their workplace. However, many individuals who work part-time or full-time with animals may receive little or no preventive health services related to their work exposures. For example, staff at pet swap meets, pet store employees, volunteers at zoos and county fair animal exhibits, wildlife rehabilitators, wildlife biologists, volunteer animal rescue workers, individuals engaged in home slaughter of animals for family consumption, and subsistence (bushmeat) hunters may all face significant “occupational” health risks related to their contact with animals, yet may never receive preplacement examinations, prophylactic vaccinations, or follow-up surveillance examinations to prevent or detect work-related disease. If they do see a medical provider for care of a work-related injury or illness, that medical provider may not be aware of the range of health risks these workers face, and therefore the treatment or recommendations for prevention may not be optimal.
OCCUPATIONAL HEALTH APPROACH
The majority of occupational health services in the United States are provided by family physicians and other clinicians without specialized training.6 However, when using a team approach these individuals can learn to provide adequate occupational health services to animal workers.
The components of an occupational health approach are simple and adaptable to a wide range of work settings. They involve identification and control of hazardous exposures, medical services such as careful screening of workers at baseline, vaccination, surveillance of workers’ health, identification of sentinel health events, and management of necessary work restrictions and work-related problems. Although such preventive services may be viewed by some employers as an unnecessary expenditure of resources, they can be cost effective in the long run by preventing potentially compensable work-related illness and injury and promoting worker well-being. Box 12-1 illustrates this approach.
OCCUPATIONAL HEALTH TEAM
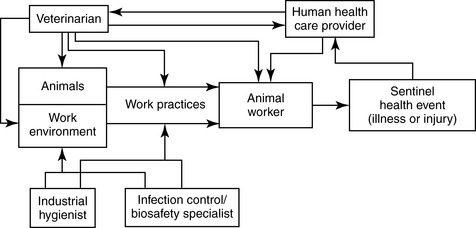
Because of the diversity of the hazards encountered by animal workers, providing effective occupational health services to such workers is best accomplished through a team approach. Such a team can include a medical provider to provide screening and management of medical problems, a veterinarian who is familiar with zoonotic disease risks, industrial hygienists to identify and evaluate hazardous exposures and help devise engineering and work practice controls to reduce them, and biosafety/infection control specialists to focus on zoonotic disease transmission risks. Figure 12-1 diagrams the ideal components of an occupational health team that provides preventive health care to animal workers.
HAZARD IDENTIFICATION
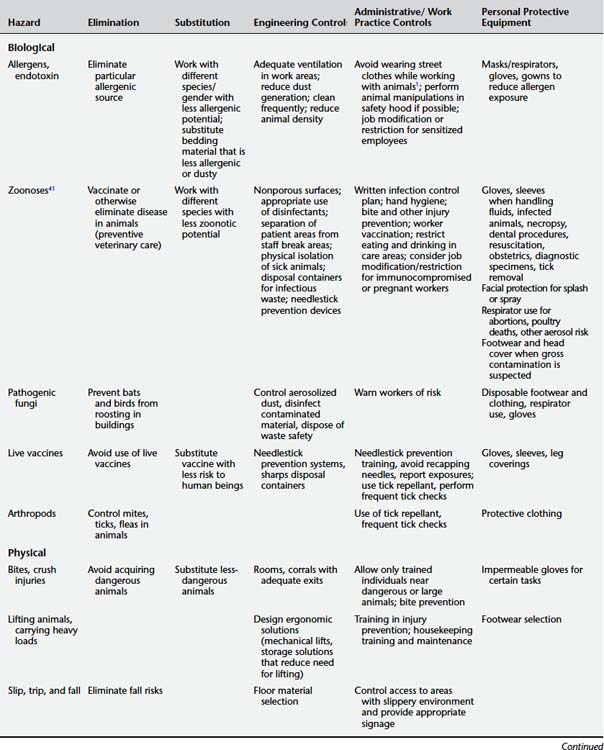
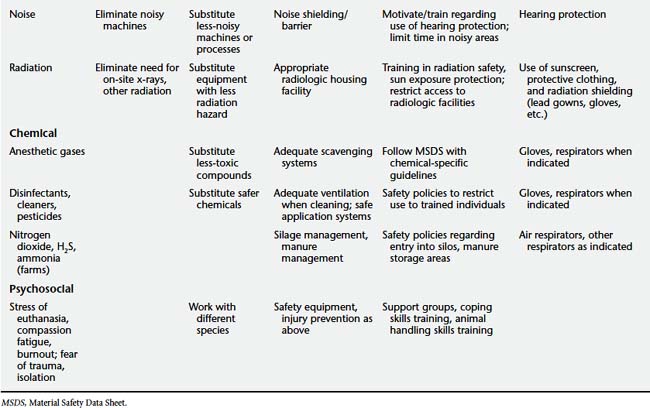
Animal workers face a wide number of potential occupational health hazards that can be classified as biological, chemical, physical, or psychosocial. These hazards and their control are listed in Table 12-1.
TABLE 12-1 Occupational Hazards Encountered by Animal Workers and Relevant Hierarchy of Control Strategies
Biological Hazards
Allergens
As discussed in Chapter 7, many animal proteins are potential allergens in human beings. Although guinea pigs, mice, rats, and cats are common causes of allergy, virtually any species, including primates, larger domestic animals (such as horses and cattle), and reptiles can also pose an allergic risk to workers.7,8 Exposure to insects such as roaches, flies, and mites as well as insect parts, shellfish (e.g., snow crabs, king crab, lobster, shrimp, scallops), and fish species (e.g., salmon, trout, pilchard, anchovy, hake) has also been associated with allergic reactions.9 Other animal-related sources of allergens in the workplace include molds and thermophilic bacteria that infect animal foods (including hay and prepared animal food) and cause asthma, rhinitis, dermatitis, and hypersensitivity pneumonitis.10
Not surprisingly, allergic reactions are a well-recognized health problem among animal workers.11 In some settings almost half of animal workers have been reported to develop allergy-related symptoms such as rhinitis, conjunctivitis, asthma, contact urticaria, and other types of allergic dermatitis.1,4,12,13 Risk factors for developing allergic responses to antigens include the intensity and duration of exposure to specific antigens4,13 and a history of atopy (allergic predisposition).14 Allergic exposures can pose a difficult problem for sensitized workers because even low levels of exposure to an allergen may provoke a response in a previously sensitized individual. In addition, personal protective equipment may not adequately protect them from further allergic reactions.
Zoonotic Pathogens
As described in Chapter 9, a large number zoonotic pathogens can pose a hazard to animal workers, who generally have increased exposures to zoonotic diseases compared with the general public. Many of these individual zoonotic diseases with occupational exposure potential are covered in Chapter 9. Selected pathogens of relevance to particular worker groups are described in the sections that follow. For example, occupational cases of Campylobacter and Chlamydophila psittaci infection have been documented among poultry workers15,16 and reported human plague cases have been reported among veterinary staff attending to infected cats.17 With the increasing focus on emerging infectious diseases, it should be remembered that many such diseases appear first or with greatest intensity in the occupational setting. The first recognized (index) human case for the epidemic of severe acute respiratory syndrome (SARS) that began in China was a chef who had extensive exposure to wild game animals in his work.18 Nipah virus, another deadly emerging viral pathogen, first broke out among Malaysian pig farm workers.19 Human outbreaks of Ebola virus infection in Africa are believed to originate at least in part from exposures to nonhuman primates and other wildlife during bushmeat hunting and butchering.20 A strain of highly pathogenic avian influenza (HPAI) has caused fatal work-related infection in a veterinarian, and human cases of H5N1 HPAI remain strongly associated with working in animal markets, poultry rearing, slaughtering, defeathering, and preparing infected birds for consumption.21 Rift Valley fever, another emerging viral disease, often occurs in human beings as an occupational disease among herdsmen engaged in activities such as assisting with cattle birthing and caring for sick animals.22
In addition to animal-human transmission, some zoonotic diseases can be “reverse zoonoses,” potentially transmitted from human beings to animals in the occupational setting. Examples include tuberculosis, which may be transmitted by human beings to nonhuman primates,23 elephants,24 and dogs.25
Live Vaccines
Accidental autoinoculation of live vaccines for diseases with zoonotic potential has been reported to result in worker infections. An example is the vaccine for Brucella abortus strain RB51.26 A 1995 survey of veterinarians found that 23% of large animal veterinarian respondents reported accidental self-inoculation with live Brucella vaccine.27
Endotoxin and Organic Dusts
Endotoxin is a biological hazard consisting of lipopolysaccharide compounds from the cell walls of gram-negative bacteria that can grow in animal bedding or feed. When the bedding or feed is disturbed, dusts are generated that can have endotoxin concentrations of 3000 nanograms per meter cubed (ng/m3), in excess of a proposed guideline2 of 9 ng/m3. Adverse respiratory effects such as bronchitis and airway obstruction have been reported in workers who inhale such dusts, especially when working in confined areas with less than adequate ventilation.28 Organic dusts from moldy grain used for animal feed can cause organic dust toxic syndrome (ODTS), a self-limited disease with symptoms including fever, cough, myalgias, headache, and shortness of breath.2
Pathogenic Fungi
A hazard related to work around areas of bird or bat droppings is the exposure to potentially pathogenic fungi including Histoplasma, Cryptococcus, and Blastomyces. Histoplasma capsulatum is a fungus that exists in two forms: a mold form in the soil environment and a yeast form that develops when human beings or other animals inhale or ingest the spores. Although many infected human beings are asymptomatic, some may develop complications ranging from mild flulike illness to chronic lung and eye infections and pericarditis.29 Skin infection can also occur. Immunocompromised individuals are at increased risk of severe disease. The nutrients in bird or bat guano can encourage the growth of spores in the environment. Therefore areas of pigeon and other bird roosting where bird droppings accumulate may be more likely to have high levels of H. capsulatum spores that can lead to inhalation or ingestion by human beings. Poultry litter can also contain Histoplasma spores. Farmers, construction workers, forestry workers, and other workers exposed to disturbed soil or poultry guano can be at risk of infection, especially if individuals are immunocompromised. Unlike birds, bats appear to shed infectious Histoplasma in their droppings. Caves and other areas where bat guano accumulates have been associated with human cases of histoplasmosis.30 The National Institute for Occupational Safety and Health (NIOSH) has published guidelines for reduction of occupational risk of Histoplasma infection that also can be applied to the risk of other fungal pathogens such as Cryptococcus and Blastomyces. These guidelines include the use of respiratory protection, disposable protective clothing and shoe coverings, and gloves that avoid skin trauma to reduce the risk of skin infection. The types of respirators that should be worn during occupational activities with exposures to spore-contaminated dusts depend on intensity of exposure. In low-risk situations (e.g., site surveys of bird roosts), disposable, filtering facepiece respirators may be adequate, whereas extremely dusty work such as removing accumulated bird or bat manure from an enclosed area such as a barn or attic may require full-facepiece, powered air-purifying respirators.31
Cryptococcus is another genus of potentially pathogenic fungi found in soil. Like Histoplasma, high concentrations of Cryptococcus spores can be found in soil enriched by bird droppings. Cryptococcus neoformans is found worldwide and can cause significant infections, including meningitis, in immunocompromised individuals. However, C. neoformans has not been extensively associated with occupational or environmental exposures. In contrast, Cryptococcus gatii infection (a species formerly thought to be confined to the tropics) has been tied to environmental and occupational exposures to disturbed contaminated soil in both human beings and domestic animals (including cats, a ferret, and a llama) in North America. In these recent outbreaks, human C. gatii infection has involved both chronic pulmonary manifestations as well as meningitis.32
Another fungus associated with environmental exposures is Blastomyces, which can cause chronic lung disease in human beings and other animals as well as extrapulmonary manifestations. The typical human case of blastomycosis related to occupational or environmental exposure is a male who works or recreates outdoors where there is wildlife activity. A history of a pet dog with the disease helps support the diagnosis because dogs appear to act as sentinels for environmental exposure risk.33
Chemical Hazards
Exposure to chemical hazards can occur in workers with animal contact, especially among laboratory animal research staff and veterinary workers. Anesthetic gases are a significant risk to veterinary personnel and are discussed below. Other chemicals include immobilizing agents, disinfectants, animal-related pesticides (see Chapter 8), rodenticides, and protocol-specific chemicals in animal research.34 These chemicals can cause a wide range of health effects from skin and mucous membrane irritation to neurological effects and adverse pregnancy outcomes (e.g., miscarriage from anesthetic exposures).35 A Materials Safety Data Sheet (MSDS) on the hazards, safe handling, and exposure management of specific chemicals should be available to all animal workers encountering chemicals in the workplace. Depending on the particular exposure, specific types of decontamination and acute medical care may be needed. In addition, inspection of the workplace should be considered in coordination with the industrial hygienist and other safety personnel.
Farm workers, especially those working in animal confinement facilities with large numbers of animals such as swine, may be exposed to pesticides as well as high levels of ammonia and hydrogen sulfide levels related to animal waste. These irritating chemical fumes can cause toxic chemical pneumonitis and bronchitis.10 Hydrogen sulfide, produced by decaying organic waste, is a mitochondrial toxin that can cause acute loss of consciousness, respiratory arrest, and death.36
Cattle silage can be a source of nitrogen dioxide toxicity causing “silo filler’s disease,” an acute syndrome characterized by pulmonary edema, respiratory distress, and death in sufficiently high exposures.37
Physical Hazards
Common physical hazards faced by animal workers include bites and crush injuries from animals; acute and chronic musculoskeletal strain from handling animals and equipment; slip, trip, and fall injuries; and, in certain settings, exposure to noise, extremes of temperature, and radiation.38
Psychosocial Stressors
Although there are many psychosocial benefits of human-animal interaction (see Chapter 5), animal workers may face particular psychosocial stressors. These can include fear of attack and injury; fear of infectious disease; emotional reactions to performing euthanasia, necropsies, slaughtering, or other procedures; compassion fatigue39; and professional burnout.40
HAZARD CONTROLS
Once workplace hazards are identified, the goal is to reduce exposures to these hazards. Taking an occupational health approach to such hazards involves using a hierarchy of controls that range from most effective to least effective methods to reduce the health risks to workers. This hierarchy is listed in Table 12-2. Many hazards can be eliminated at the source, or a less-dangerous substance or process can be substituted. Engineering controls include physical methods to reduce exposures such as improved ventilation and use of nonporous surfaces on counters that can be easily disinfected. Administrative and work practice controls involve job restrictions for susceptible persons, limiting individual worker exposure times in high-exposure areas, and preventive practices such as hand hygiene. Reliance on personal protective equipment such as gloves, gowns, and respirators is considered to be the least effective and often most cumbersome approach to hazard control.
TABLE 12-2 Hierarchy of Controls for Workplace Hazards
| Control Strategy | Effectiveness |
|---|---|
| 1. Eliminate the hazard | Most effective |
| 2. Substitute for the hazard |  |
| 3. Engineering controls | |
| 4. Administrative/work practice controls | |
| 5. Use of personal protective equipment (e.g., gloves, masks) | Least effective |
Table 12-1 shows examples of such controls for handling biological, chemical, physical, and psychosocial hazards in animal work. Obviously the most effective controls vary by the specific type of hazard, and the occupational health team must consider the most feasible type of control for each particular hazard. Although they may require a greater up-front investment, controls at the top of the hierarchy, such as elimination, substitution, or engineering controls, may be most cost effective at preventing work-related health problems. For example, eliminating a zoonotic disease (such as brucellosis) in an animal population through vaccination and other preventive veterinary care may be more cost effective over time than relying on personal protective equipment such as respirators and gloves for animal workers. Similarly, substituting a less-toxic cleaning agent (see Chapter 8) may be more cost effective in reducing health complaints of eye and throat irritation among exposed workers than the use of gloves and respirators.
OCCUPATIONAL MEDICINE SERVICES
Preplacement Screening
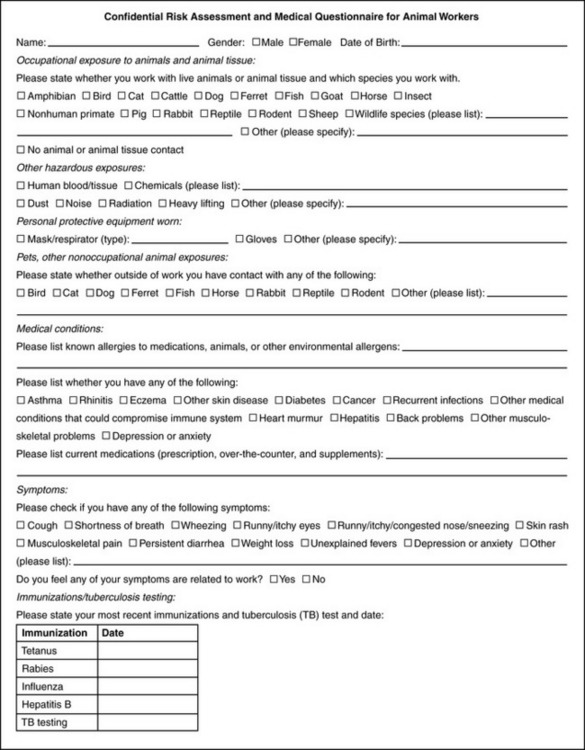
The content of the preplacement examination can vary depending on the particular job type and set of exposure risks but often involves a screening medical history, physical examination, and diagnostic testing, if indicated, to identify important preexisting conditions that might place an individual at increased risk of injury or illness, including immunocompromising conditions41 or history of allergy. A history of previous animal contacts and whether animals are kept in the home may provide useful information. The use of standardized history and physical forms may assist in this process. Figure 12-2 shows an example of an animal worker questionnaire that might be appropriate for a worker in an animal care facility or a veterinary practice.
If workers will be using respiratory protection involving N-95 respirators or other types of respirators, they should complete the Occupational Safety and Health Administration (OSHA) respirator questionnaire as part of the respirator medical clearance required under the OSHA Respirator Standard 1910.134 (available at http://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=STANDARDS&p_id=9783). If latex is used in the workplace, workers should be asked about any previous reactions to latex, including rash, hives, nasal or eye inflammation, breathing difficulties, or anaphylaxis.
Based on the findings of the preplacement examination, the medical provider can perform a risk assessment for the individual and decide whether the individual can safely do the job with or without accommodation. To do this, the medical provider may need to consult a veterinarian, biosafety professional, or other members of the occupational health team to learn more about specific risks of the job. For example, a person with valvular heart disease may need to be restricted from working in a research facility with pregnant sheep because of the risk of Q fever. A worker who developed allergy to mice or rats in a previous job may need to be restricted from future contact with such animals. In discussing disease risks with other professionals, it is important (although sometimes a challenge) to keep medical information about the worker confidential and prevent possible workplace discrimination because of a medical condition. If work restrictions are necessary, they can be indicated on a work status form that can be given to the employer to outline such restrictions without revealing confidential health information about the employee. In general, confidential health information on employees should not be shared with the employer, supervisor, or other management personnel by the human health clinician evaluating the worker.42
Vaccinations
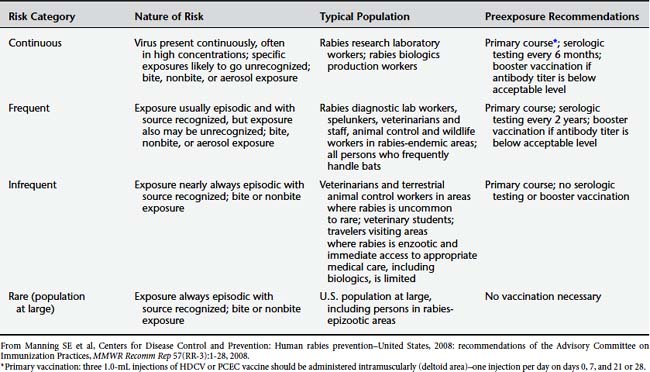
A number of preventive vaccinations may be indicated for animal workers. Previous vaccination history should be assessed at the preplacement evaluation and the need for additional vaccination determined. As with other aspects of the preplacement risk assessment, consultation with a veterinarian may be advisable or clear instructions conveyed to the health care provider regarding necessary vaccinations. All animal workers should be up to date with respect to tetanus vaccination. Table 12-3 lists vaccines to consider for particular groups of workers. Rabies vaccination is indicated for a number of workers.43 Table 12-4 shows recent recommendations for which individuals should receive preexposure rabies vaccine.
TABLE 12-3 Occupational Medicine Services for Animal Workers
| Category of Medical Service | Specific Medical Services Indicated | Types of Animal Workers Requiring Occupational Medicine Services |
|---|---|---|
| Preplacement screening | All | |
| Respirator clearance questionnaire, spirometry | Workers exposed to respiratory hazards, workers who will be using respirators | |
| Audiometry | Noise-exposed workers | |
| HIV and TB screening | Animal research and workers in contact with nonhuman primates | |
| Consider serum banking | Zoological, wildlife, or research workers; others with zoonotic exposures | |
| Vaccination | Rabies | See Table 12-4 |
| Tetanus (every 10 years) | All | |
| Annual influenza vaccine | All (especially poultry and swine workers) | |
| Anthrax | Laboratory workers routinely working with concentrations of anthrax or aerosol potential87 | |
| Q fever (consider)* | Laboratory workers, researchers working with pregnant sheep, slaughterhouse workers70 | |
| Hepatitis A and B, measles, polio | Workers in contact with chimpanzees and other nonhuman primates | |
| Training | Veterinary standard precautions, anesthetic safety, bite and injury prevention, OSHA training, safe chemical handling | All |
| Medical surveillance | Periodic questionnaire about allergy/respiratory symptoms | NIOSH recommendations in all animal workers with allergen exposures |
| Reassess zoonotic disease risk | All animal workers with change in medical status | |
| OSHA respirator questionnaire; spirometry; further evaluation in positive responses to questionnaire | Workers using respirators | |
| TB testing (skin test or interferon assay) | Animal workers with nonhuman primate and/or elephant contact (see Figure 12-2) | |
| Annual audiometry | Workers with noise exposures ≥85 dBA (8-hour average) | |
| Acute injury and illness management | Treat acute problem, determine if work related, identify sentinel health events indicating problem with hazard control and risk to other workers and/or patients Consider whether human being with a zoonotic disease is a sentinel for animal health problem as well as indicator of occupational risk to other workers | All |
| Herpes B exposure prophylactic treatment65 | Workers with exposure to nonhuman primates | |
| Confidential medical record management | Protect confidentiality of medical records | All |
HIV, Human immunodeficiency virus; TB, tuberculosis; OSHA, Occupational Safety and Health Administration; dBA, decibels (acoustic).
* Not commercially available in the United States. Persons wishing to be vaccinated should first have a skin test to determine a history of previous exposure. Individuals who have previously been exposed to C. burnetii should not receive the vaccine because severe reactions, localized to the area of the injected vaccine, may occur.
Training
Training at the time of job entry is recommended by the National Association of Public Health Veterinarians (NAPHV) for workers in veterinary facilities41 and is relevant for other animal workers as well. Aspects of such training include education about zoonotic disease risks, infection control practices, use of personal protective equipment, safe chemical handling techniques, and injury prevention, with emphasis on proper animal handling, restraints, and recognition of behavioral cues in animals. Such training should be provided by an individual familiar with the risks of a particular workplace and the safety policies in place, such as a safety officer. Training should be documented. Follow-up training in health and safety can take place on a regular basis with animal workers to identify and mitigate hazards, address institutional occupational health policies (including record keeping), address personal hygiene, provide points of contact for more information or for when to seek medical attention for work-related problems, review unit inspection standards, and evaluate future training needs.
Medical Surveillance
Depending on the degree of occupational risk, animal workers should receive periodic evaluations to detect evidence of work-related disease, reassess risk factors for occupational illness and injury, and ensure that vaccinations are current. Table 12-1 suggests medical surveillance that may be appropriate for different types of animal workers.
Questionnaires should ask about new health problems that have developed since the last examination, including symptoms of allergy or infection that could indicate increased risk of disease or the occurrence of work-related disease or injury. A key aspect of such history is whether the symptoms show a temporal relation with work exposures. Box 12-2 shows characteristic symptom patterns suggesting work-related occupational asthma. Similar temporal relations may occur with other occupational diseases.
BOX 12-2 Pattern of Symptoms of Work-Related Asthma
From National Institute for Occupational Safety and Health (NIOSH): NIOSH alert: preventing asthma in animal handlers, DHHS (NIOSH) Publication No. 97-116. http://www.cdc.gov/Niosh/animalrt.html.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree