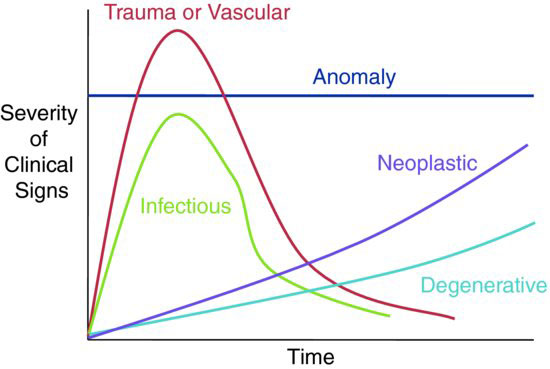
Information regarding the number of animals involved on the farm, nutritional and water access, exposure to other species, breeding activity, vaccination and anthelmintic use, previous medical issues, and response to any therapies should be obtained. The Sign-Time Graph (Figure 65.1) may be used with the historical information on duration and severity of clinical course and can help delineate possible etiologies.
Figure 65.1 The Sign-Time Graph for determining etiologic classification of neurologic disease by severity of onset and progression of clinical signs.
Neurologic evaluation should begin with a distance examination of posture, balance, ambulation, ability to negotiate obstacles, and behavior. Based on the results of the initial distance evaluation, a thorough neurologic examination may be performed to provide more specific information. Gloves should be worn during examination and handling of all animals with potential neurologic disease. Clinical signs noted may provide lesion localization based on the following criteria:
- Cerebrum: Symptoms may include a depressed mental state, cortical blindness normal pupillary light response (PLR), circling/leaning, yawning, head pressing, opisthotonus, seizures, bizarre behavior.
- Vision: Blindness may be from cerebral or brainstem origin (central) or may originate between the optic chiasm and the globe itself (peripheral). The menace response is commonly used to test for vision, but it must be carefully executed and interpreted. First, the examiner must not generate wind currents, which induce blinking due to corneal sensation. Additionally, the menace response is learned and therefore is not present in the early neonatal period. Vision testing is best performed using an obstacle test in ambulatory animals. The PLR is used in blind animals to determine if the blindness is central or peripheral. Centrally blind animals have normal PLR, while peripherally blind animals have an absent PLR.
- Cerebellum: Symptoms may include ataxia without paresis, mental alertness, intention tremors, nystagmus, truncal sway, base-wide stance, hypermetria, picking up feet and slamming them down hard, excellent muscle tone, falling over backwards, no conscious proprioceptive deficits, lacking menace response but having normal vision.
- Brainstem and Central Vestibular System: Symptoms may include depression, mania, ataxia and paresis, cranial nerve deficits (Figure 65.2), irregular respiration, head tilt, eyelid droop, circling, hemiparesis, nystagmus, ataxia with weakness, recumbency (lesion side down) with contralateral limbs hyperextended and hyperreflexic, loss of appetite.
The following symptoms may exist:
- Common cranial nerve signs include muscular atrophy, dropped jaw, inability to chew, ptyalism, loss of facial sensation (test ear and nose [V—trigeminal n.])
- Droopy eye, ear, lip muzzle deviation (VII—facial n.)
- Food retention in mouth (VII—facial n., XII—hypoglossal n.)
- Head tilt (VIII—abducent n.)
- Abnormal tongue tone and movement (XII—hypoglossal n.)
- Abnormal swallowing (IX—glossop- haryngeal n., X—vagus n.)
- Common cranial nerve signs include muscular atrophy, dropped jaw, inability to chew, ptyalism, loss of facial sensation (test ear and nose [V—trigeminal n.])
- Peripheral Vestibular System: Though patients are usually not depressed, they may exhibit head tilt, ear droop, leaning, circling all toward lesion, horizontal nystagmus, ataxia without weakness, bright, alert, good appetite.
- Spinal Cord: Symptoms may include paresis, ataxia, dysmetria, recumbency, normal mental status.
- Reflexes: Flexor, patellar, triceps, and crossed extensor reflexes may be tested. When reflexes are exaggerated and upper motor neuron (UMN) lesion is indicated, reduced reflexes indicate a lower motor neuron (LMN) lesion.
- C1-C5: Altered head and neck movements, CP deficits and ataxia/weakness of all four limbs (Figure 65.3), recumbency, truncal sway, knuckling, stumbling, all four limbs hyperreflexive (UMN)
- C6-T2: CP deficits and ataxia/weakness to all four limbs, recumbency, hyporeflexive front limbs (LMN), hyperreflexive hind limbs (UMN)
- T3-L3: CP deficits and ataxia/weakness to hind limbs, hyperreflexive hind limbs (UMN)
- L4-S2: CP deficits and ataxia/weakness to hind limbs, hyporeflexive to hind limbs (LMN)
- S2-Cd: Loss of anal tone, urinary bladder dribbles (LMN bladder)
- C1-C5: Altered head and neck movements, CP deficits and ataxia/weakness of all four limbs (Figure 65.3), recumbency, truncal sway, knuckling, stumbling, all four limbs hyperreflexive (UMN)
- Peripheral Nerves: Symptoms include weakness, paralysis, decreased muscle tone, muscle atrophy.
- Obturator: The patient cannot adduct hind limbs—splay hind legs.
- Sciatic: extended stifle, flexed hip, flexed or extended hock or fetlock
- Femoral: flexed stifle, extended hip, crouching stance in young calves
- Peroneal: extended hock, flexed fetlock
- Tibial: partially knuckled fetlock, flexed hock
- Suprascapular: short-strided gait, abduction of the leg and shoulder during weight bearing, atrophy of supraspinatus and infraspinatus mm.
- Radial: Symptoms include dropped elbow to complete forelimb paralysis. High damage includes cannot bear weight, flexed elbow and fetlock. Low damage includes can bear weight, flexed fetlock.
- Obturator: The patient cannot adduct hind limbs—splay hind legs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



