Chapter 6. Minerals
Minerals have a variety of functions in the body. They activate enzymatically catalyzed reactions, provide skeletal support, aid in nerve transmission and muscle contractions, serve as components of certain transport proteins and hormones, and function in maintaining water and electrolyte balance. Significant interrelationships exist among many of the mineral elements that can affect mineral absorption, metabolism, and functioning. Specifically, excesses or deficiencies of some minerals can significantly affect the body’s ability to use other minerals in the diet. As a result, the level of most minerals in the diet should be considered in relation to other components of the diet, with a goal of achieving an optimal overall dietary balance. Although most of the minerals are discussed separately in this section, the importance of these interrelationships is addressed when they are of practical significance to the nutrition of dogs and cats. A summary of food sources and signs of mineral deficiency and excess is shown in Table 6-1.
| M ineral | D eficiency | E xcess | S ources |
|---|---|---|---|
| Calcium | Rickets, osteomalacia, nutritional secondary hyperparathyroidism | Impaired skeletal development; contributes to other mineral deficiencies | Dairy products, poultry and meat meals, bone |
| Phosphorus | Same as for calcium deficiency | Causes calcium deficiency | Meat, poultry, fish |
| Magnesium | Soft tissue calcification, enlargement of long bone metaphysis, neuromuscular irritability | Dietary excess unlikely; absorption is regulated according to needs | Soybeans, corn, cereal grains, bone meals |
| Sulfur | Not reported | Not reported | Meat, poultry, fish |
| Iron | Hypochromic microcytic anemia | Dietary excess unlikely; absorption is regulated according to needs | Organ meats |
| Copper | Hypochromic microcytic anemia, impaired skeletal growth | Inherited disorder of copper metabolism causes liver disease | Organ meats |
| Zinc | Dermatoses, hair depigmentation, growth retardation, reproductive failure | Causes calcium and copper deficiency | Beef liver, dark poultry meat, milk, egg yolks, legumes |
| Manganese | Dietary deficiency unlikely; impaired skeletal growth, reproductive failure | Dietary excess unlikely | Meat, poultry, fish |
| Iodine | Dietary deficiency unlikely; goiter, growth retardation, reproductive failure | Dietary excess unlikely; goiter | Fish, beef, liver |
| Selenium | Dietary deficiency unlikely; skeletal and cardiac myopathies | Dietary excess unlikely; necrotizing myocarditis, toxic hepatitis and nephritis | Grains, meat, poultry |
| Cobalt | Dietary deficiency unlikely; vitamin B 12 deficiency, anemia | Not reported | Fish, dairy products |
Minerals are inorganic elements that make up only about 4% of an animal’s total body weight; nonetheless, the essential minerals must be present in the diet to sustain life and maintain health.
CALCIUM AND PHOSPHORUS
Calcium and phosphorus are usually discussed together because their metabolism and the homeostatic mechanisms that control their levels within the body are closely interrelated. Calcium is a principal inorganic component of bone. As much as 99% of the body’s calcium is found in the skeleton; the remaining 1% is distributed throughout the extracellular and intracellular fluids. Phosphorus is also an important component of bone. Approximately 85% of the body’s phosphorus is found in inorganic combination with calcium as hydroxyapatite in bones and teeth. Most of the remaining portion of this mineral is found (in combination with organic substances) in the soft tissues.
The calcium in bone provides structural integrity to the skeleton and also contributes to the maintenance of proper blood calcium levels through ongoing resorption and deposition. The calcium in bone tissue is not in a static state but is constantly being mobilized and deposited as bone growth and maintenance take place and as the body’s needs for plasma calcium fluctuate. The level of circulating plasma calcium is strictly controlled through homeostatic mechanisms and is independent of an animal’s dietary intake of calcium. Circulating calcium has essential roles in nerve impulse transmission, muscle contraction, blood coagulation, activation of certain enzyme systems, maintenance of normal cell-membrane permeability and transport, and cardiac function.
Phosphorus that is present in bone is found primarily in combination with calcium in the compound called hydroxyapatite. Like calcium, this phosphorus lends structural support to the skeleton and is also released into the bloodstream in response to homeostatic mechanisms. The phosphorus that is found in the soft tissues of the body has a wide range of functions and is involved in almost all of the body’s metabolic processes. It is a constituent of cellular deoxyribonucleic acid (DNA) and ribonucleic acid (RNA), several B-vitamin coenzymes, and the cell membrane’s phospholipids, which are important for regulating the transport of solutes into and out of cells. Phosphorus is also necessary for the phosphorylation reactions that are part of many oxidative pathways for the metabolism of the energy-containing nutrients. Phosphorus is a component of the high-energy phosphate bonds of adenosine triphosphate (ATP), adenosine diphosphate, and cyclic adenosine monophosphate.
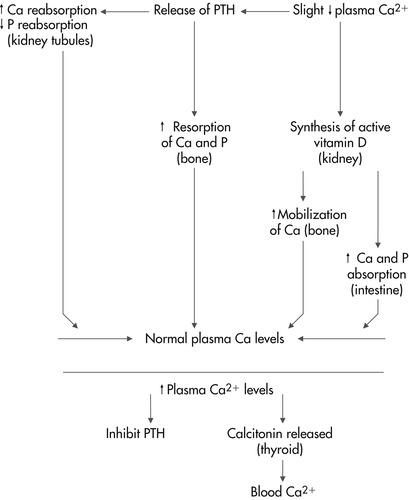
As mentioned previously, the body has several strictly controlled homeostatic mechanisms that are designed to maintain a constant level of circulating plasma calcium. These mechanisms involve parathyroid hormone (PTH), calcitonin, and active vitamin D (calcitriol). PTH is released into the bloodstream in response to a slight decrease in plasma calcium. This hormone stimulates the synthesis of active vitamin D in the kidneys and increases the resorption of calcium and phosphorus from bone. It also works on the kidney tubules to increase calcium reabsorption and decrease phosphorus reabsorption, resulting in increased retention of calcium in the body and increased losses of urinary phosphate. In turn, the active vitamin D produced by the kidneys in response to PTH acts at the site of the intestine to increase the absorption of dietary calcium and phosphorus. In conjunction with PTH, vitamin D also enhances the mobilization of calcium from bone by increasing the activity of osteoclasts. Overall, the net action of PTH is to increase the serum concentration of calcium and decrease the serum concentration of phosphorus. The net effect of active vitamin D is to increase levels of both serum calcium and phosphorus (Figure 6-1).
When the blood calcium level is normal, PTH secretion is inhibited through a negative feedback mechanism, and calcitonin, a hormone produced by the parafollicular cells (C cells) of the thyroid gland, is released. Calcitonin functions to reduce blood calcium levels by acting primarily to increase osteoblastic activity and decrease osteoclastic activity in bone tissue. The end result is a decrease in calcium mobilization from the skeleton. Calcitonin is also released in response to hypercalcemia and the release of certain hormones, such as gastrin. Under normal physiological circumstances, PTH and active vitamin D are the most important regulators of calcium homeostasis, with calcitonin playing a more minor role. However, calcitonin may be of increased importance in the normal homeostatic mechanisms of calcium regulation during growth, pregnancy, and lactation.
In addition to having common homeostatic mechanisms in the body, calcium and phosphorus also have an important relationship to each other within the diet. Once adequate levels of calcium and phosphorus have been included in the diet, it is important to consider the ratio of the amount of calcium to phosphorus. Excess dietary calcium forms an insoluble complex with phosphorus, resulting in decreased phosphorus absorption. Similarly, high levels of phosphorus or phytate in the diet can inhibit calcium absorption. Phytate is a phosphorus-containing compound found in the outer husks of cereal grains. Although this compound is high in phosphorus, the mineral is poorly available to the body. The recommended ratio of calcium to phosphorus in pet foods is between 1:1 and 2:1. 1 Feeding animals foods that have an improper calcium:phosphorus ratio or supplementing balanced foods with high amounts of either one of these minerals can lead to calcium or phosphorus imbalance. Such problems are usually manifested as skeletal disease in growing and adult animals (see Section 5, pp. 497-499 for a complete discussion).
Foods vary greatly in their calcium content. Dairy products and legumes contain high amounts, but cereal grains, meat, and organ tissues contain very little. The bioavailability of calcium in a food is influenced not only by the source of the mineral, but also by other dietary constituents and the animal’s life stage (see Chapter 13, pp. 111-113). Phosphorus, on the other hand, is widely distributed in foods. Foods that contain both phosphorus and calcium include dairy products and legumes. Fish, meats, poultry, and organ meats are also very rich sources of phosphorus. However, these foods are very deficient in calcium, and so their inclusion in the diets of dogs and cats must be balanced by a dietary source of calcium to ensure that an adequate calcium:phosphorus ratio is still maintained.
MAGNESIUM
Although magnesium is a macromineral, its amount in the body is much lower than that of calcium and phosphorus. Approximately 60% to 70% of the magnesium found in the body exists in the form of phosphates and carbonates in bone. Most of the remaining magnesium is found within cells, and a very small portion is present in the extracellular fluid. In addition to its role in providing structure to the skeleton, magnesium functions in a number of metabolic reactions; a magnesium-ATP complex is often the form of ATP that is used as a substrate in many of these processes. As a cation in the intracellular fluid, magnesium is essential for the cellular metabolism of both carbohydrate and protein. Protein synthesis also requires the presence of ionized magnesium. Balanced in the extracellular fluids with calcium, sodium, and potassium, magnesium allows muscle contraction and proper transmission of nerve impulses.
Magnesium is widespread in food sources and is abundant in whole grains, legumes, and dairy products. Naturally occurring magnesium deficiency is not common in dogs and cats. However, excess magnesium in the diets of cats has been implicated as a risk factor for struvite urolithiasis (see Section 5, pp. 362-365 for a complete discussion).
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree