3 Microbiology
Microorganisms in the body metabolize nutrients. The presence of the normal bacterial population in a given area of the body prevents growth of abnormal bacteria that presumably could cause harm. Areas of the body that always harbor some bacteria are the skin, nasal cavity, mouth and throat, vagina, end of the urethra, penile and preputial mucosa, and intestinal tract. Control of microorganisms in the body requires use of antibiotics (see Chapter 2).
I. TYPES OF ORGANISMS
A. BACTERIA
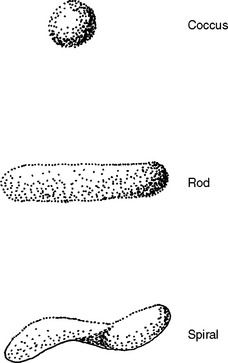
Bacteria can be classified by shape, by atmosphere in which they grow, or by staining characteristics. Common bacterial shapes are rods, cocci, and spirals (Figure 3-1). Aerobic bacteria are those that require air to reproduce; anaerobic bacteria are those that do not reproduce in air.
Gram staining is a differential staining with safranin, which stains some bacteria pink, and crystal violet, which stains some bacteria purple. A specimen is smeared on a glass slide and dried and fixed with heat. The slide is stained with crystal violet, then washed and treated with iodine. Then the slide is decolorized with alcohol or acetone and the slide stained with safranin. Those bacteria classified as gram-positive (gram+) do not decolorize and so retain the purple color; those classified as gram-negative (gram-) stain pink with safranin.
Bacteria show this differential staining because of differences in their cell wall. All bacteria have a rigid cell wall composed of compounds called peptidoglycans and lipopolysaccharides. These compounds control movement of water and other molecules in and out of the bacterial cell, protecting the nucleus and organelles within. The nucleus contains the genetic material of the cell, and the organelles generate energy, synthesize protein, and metabolize nutrients within the cell. Gram+ bacteria have a thick peptidoglycan layer. Gram- bacteria have a thin peptidoglycan layer and thick lipopolysaccharide layer (Figure 3-2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree