Hernia Fixation Devices
While the mesh can be secured exclusively with transfascial sutures using conventional materials, a combination of transfascial sutures and hernia fixation devices (tacks or anchors) technically simplifies placement of the patch. The dimensions of available hernia fixation devices are sufficiently diminutive that their predominant or exclusive use for mesh fixation is controversial in people and definitely ill-advised in adult horses. As for mesh materials, the number of choices of hernia fixation devices is expanding. Suitable devices can be acquired from reputable endosurgical supply companies.
Suture Passer
A number of devices to retrieve preplaced mesh sutures and to facilitate placement of transfascial sutures are available. The BERCI Fascial Closure Instrument (Karl Storz GmbH & Co, Tuttlingen, Germany) seems the most robust of currently available devices (Figure 25.2). A less expensive, albeit less durable alternative, is the Carter-Thomason CloseSure® System (Inlet Medical, Eden Prairie, MN).
Figure 25.2 The BERCI fascial closure device. Durable construction of this suture passer is compatible with use in adult horses. Inset: open jaws of the suture passer.

Surgery
Portals
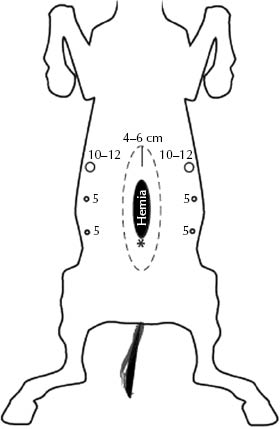
The author’s preference is to establish initial abdominal access with a 5-mm cannula using a modified open (Hasson) technique on the midline, 4–5 cm beyond the intended cranial limit of the prosthesis. After creating pneumoperitoneum (10–12 mmHg generally suffices), one 12- or 15-mm telescope portal and two 5-mm (or 10 mm if larger laparoscopic instruments are used) instrument portals are created ∼12–15 cm lateral to the hernia edges on one side, and a 10-mm telescope and two 5-mm (or 10-mm) instrument portals are made on the opposite side (Figure 25.3) under endoscopic observation with a 5-mm telescope. The initial ventral midline approach permits the creation of the subsequent six portals under visual control, as far lateral as possible, which facilitates subsequent manipulations. The large (12–15 mm) cannula is used both for the introduction of the hernia patch and the telescope. The corresponding 10-mm cannula on the opposite side of the abdomen is also used as a telescope portal, and the 5-mm cannulas are used for instruments. A 30° forward-oblique viewing telescope is particularly helpful for this procedure.
Figure 25.3 Telescope and instrument portal locations for laparoscopic incisional hernioplasty. A 12/15 mm portal serves as a telescope and prosthesis inserting port, and two 5-mm instrument portals are placed at a generous distance (∼12–15 cm) lateral to the palpable edge of the hernia defect. This arrangement is duplicated with a 10-mm telescope and two 5-mm instrument portals on the opposite side (if one prefers, 10-mm instrument portals can be used bilaterally). A telescope and two instrument portals on each side of the hernial ring facilitate dissection of retroperitoneal fat and positioning, tensioning, and securing the prosthesis. The asterisk represents the umbilicus.
Anatomy
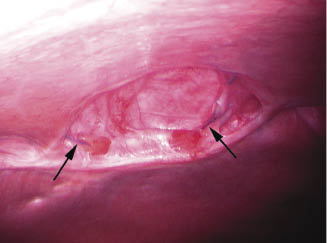
The pertinent anatomy is relatively straightforward; the principal hernia margins are generally visually evident, and external digital palpation and transabdominal external palpation of laparoscopically placed instruments can be used to confirm the nature of the principal body wall defect and any previously unrecognized defect(s) (Figure 25.4).
Figure 25.4 Laparoscopic appearance of an incisional hernia defect measuring 10 × 15 cm. Suture material remaining from a previous hernioplasty attempt is visible (arrows).
Mesh Hernioplasty
A tracing of the intended location of a prosthesis of sufficient size to exceed the defect by 4–5 cm in all directions is made on the ventral body wall skin using a sterile surgical marker by outlining a sterile template duplicating the dimensions of the prosthesis.
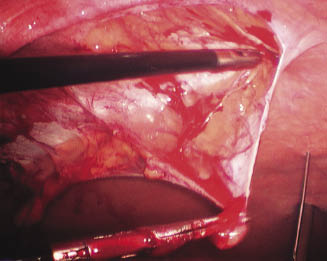
If necessary, bowel–body wall adhesions are divided with endoscopic scissors. Laparoscopic scissors, with judicious use of monopolar cautery, are used to dissect retroperitoneal fat from the surface of the underlying internal rectus sheath 6–7 cm circumferentially from the palpable hernia ring (Figure 25.5). (This distance can be estimated with transabdominally placed spinal needles.) Dissection of retroperitoneal fat on the left side of the defect is conducted via portals on the right side of the abdomen and vice versa. There appears to be no untoward effect of leaving the dissected fat in situ. The intraperitoneal lining of the hernia sac is thin, contains little or no fat, and is best left intact.
Figure 25.5 Circumferential dissection of retroperitoneal fat from the area to be occupied by the prosthesis. A transabdominally placed spinal needle (lower right) marks the extent of dissection required for the intended size of the hernia patch.
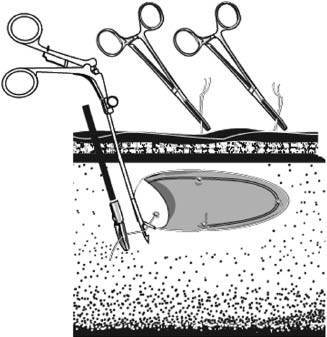
An appropriately sized prosthetic mesh has four simple interrupted sutures of 2 nylon with long tails attached placed at cranial, caudal, and midlateral edges. The prosthesis is rolled tightly and, to minimize the chances for contamination of the prosthesis by contact with the skin, is introduced into the abdominal cavity via one of the larger cannulas (the choice of a 12- or 15-mm cannula is based on the dimensions and composition of the prosthesis). The patch is unrolled and correctly oriented within the abdomen. Four 5- to 8-mm stab incisions are made in the skin and are extended to the level of the external rectus sheath corresponding to the anticipated final location of the borders of the patch. The suture passer is used to retrieve the suture ends through each of the stab incisions, taking care to incorporate approximately 1 cm of body wall in each (Figure 25.6). Traction on the ends of the sutures elevates the patch to its intended position on the undersurface of the internal rectus sheath, and once it is assured that the mesh is appropriately positioned, each of the four sutures is tied.
Figure 25.6 Schematic representation of the technique used to position mesh. Sutures of 2 nylon preplaced at the cranial, caudal, and midlateral edges of the prosthesis are retrieved by percutaneous introduction of a suture passer, exteriorized, and tied at the level of the external rectus sheath.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


