Chapter 1 Mammals
Case 1.1
Physical examination
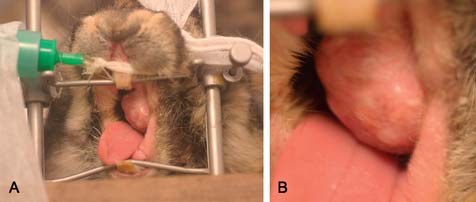
The rabbit appeared well and in good body condition. The mass in the left cheek was easily palpable and could be visualized on oral examination with an auriscope. The surface appeared smooth with no ulceration (Fig. 1.1). There was no pain associated with the mass. Dental roots could not be palpated. Oral examination (as far as it allowed) detected no evidence of dental disease. The mass did not appear excoriated or ulcerated. There were no other masses detectable in the abdomen or on the skin.
Therapy
The mass was removed using radiosurgery (Fig. 1.4). It was well encapsulated – histopathology confirmed it had been completely removed. The wound was sutured using 4/0 Vicryl (Ethicon) and covered with Orabase gel.
Postoperative medical management
 Antibiosis – trimethoprim–sulphonamide at 30 mg/kg BID for 7 days
Antibiosis – trimethoprim–sulphonamide at 30 mg/kg BID for 7 days
 Analgesia – meloxicam at 1 mg/kg BID for 5 days
Analgesia – meloxicam at 1 mg/kg BID for 5 days
 Support feeding using Critical Care (Oxbow) until feeding well for herself
Support feeding using Critical Care (Oxbow) until feeding well for herself
 Metoclopramide at 1 mg/kg BID subcutaneously until faeces passed normally – the rabbit was hospitalized until this stage
Metoclopramide at 1 mg/kg BID subcutaneously until faeces passed normally – the rabbit was hospitalized until this stage
Flecknell P. Anaesthesia and perioperative care. In: Flecknell E., Meredith A. BSAVA Manual of Rabbit Medicine and Surgery. second ed. Gloucester: British Small Animal Veterinary Association; 2006:154–165.
Harcourt-Brown F. Textbook of Rabbit Medicine. Oxford: Butterworth Heinemann; 2002.
Oglesbee B.L. The 5-Minute Veterinary Consult: Ferret and Rabbit. Ames: Wiley Blackwell; 2006.
Case 1.2
Physical examination
The rabbit appeared well on examination. There was hair loss and crusting around the eyes with evidence of a serous ocular discharge though there were no signs of conjunctivitis (Fig. 1.5). There were many scabs around the nose with associated purulent discharge (Fig. 1.6). These appeared partially to occlude the nares, resulting in an increased respiratory effort, and nose. Other than referred noise there were no abnormalities on thoracic auscultation. There was also crusting around the vent (Fig. 1.7). There were no other signs on examination.
Diagnostic plan
Initial therapy
By the time results returned (7 days) the lesions had worsened.
![]() 4. Why do you feel this was the case?
4. Why do you feel this was the case?
Harcourt-Brown F. Textbook of Rabbit Medicine. Oxford: Butterworth Heinemann; 2002.
Meredith A. Dermatoses. In: Keeble E., Meredith A. BSAVA Manual of Rabbit Medicine and Surgery. second ed. Gloucester: British Small Animal Veterinary Association; 2006:129–136.
Oglesbee B.L. The 5-Minute Veterinary Consult: Ferret and Rabbit. Ames: Wiley Blackwell; 2006.
Case 1.3
Clinical examination
On presentation, the rabbit was a good weight and bright and alert. Abnormalities included white exudate in the right ear canal, and thickening of the base of the ear. The left ear canal was stenotic and could not be visualized beyond the horizontal portion. There was scant dried ocular discharge associated with the right eye. The rest of the examination was unremarkable. A blood sample was collected for haematology, which was unremarkable, and chemistry analysis, which is presented in Table 1.1. The rabbit was then sedated for survey radiographs of the skull, and collection of a sample from the right ear canal for culture and sensitivity.
Table 1.1 Blood chemistry results of the rabbit
| Analysis | Results | Reference values |
|---|---|---|
| Albumin (g/l) | 3.24 | 2.4–4.6 |
| ALP (U/l) | 20 | 4–16 |
| ALT (U/l) | 54 | 48–80 |
| Bilirubin (mg/dl) | 0.2 | 0.0–0.7 |
| Calcium (mg/dl) | 12.0 | 5.6–12.5 |
| Phosphorus (mg/dl) | 5.2 | 4.0–6.9 |
| Creatinine (μmol/l) | 0.8 | 0.5–2.5 |
| BUN | 14 | 13–29 |
| Glucose (mg/dl) | 144 | 75–155 |
| Total protein (g/l) | 6.7 | 5.4–8.3 |
| Globulin (g/dl) | 3.46 | 1.5–2.8 |
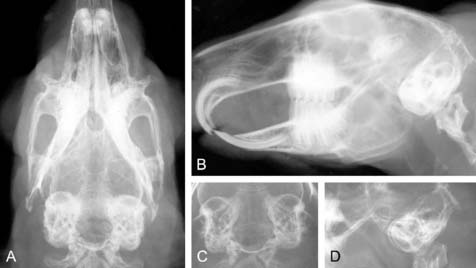
Radiography interpretation
 Radiographic quality and positioning is fair to good, which is important for interpretation of the skull, and in particular the tympanic bullae
Radiographic quality and positioning is fair to good, which is important for interpretation of the skull, and in particular the tympanic bullae
![]() 2. What is your interpretation of the blood chemistry and plasma protein electrophoresis values of the rabbit (Tables 1.1 and 1.2)?
2. What is your interpretation of the blood chemistry and plasma protein electrophoresis values of the rabbit (Tables 1.1 and 1.2)?
Table 1.2 Plasma protein electrophoresis of the rabbit
| Parameters (g/dl) | Level | Range |
|---|---|---|
| Total protein | 5.6 | 4–6 |
| Albumin | 2.89 | 1.7–3.6 |
| Alpha 1 globulins | 0.22 | 0.2–0.6 |
| Alpha 2 globulins | 0.69 | 0.2–0.8 |
| Beta globulins | 1.14 | 0.6–1.1 |
| Gamma globulins | 0.66 | 0.6–1.0 |
| A:G ratio | 1.07 | 0.8–1.3 |
Results
 Mild elevation of globulins, increase in beta globulins which may reflect an underlying acute inflammatory process
Mild elevation of globulins, increase in beta globulins which may reflect an underlying acute inflammatory process
 Mild elevation of alkaline phosphatase (ALP) is unlikely to be of significance
Mild elevation of alkaline phosphatase (ALP) is unlikely to be of significance
Please evaluate the clinical history, Fig. 1.8a–d, the results of the physical examination and clinical diagnosis laboratory tests.
![]() 3. List your differential diagnoses.
3. List your differential diagnoses.
![]() 4. List your therapeutic strategy, and suggestions for additional diagnostic testing, if indicated.
4. List your therapeutic strategy, and suggestions for additional diagnostic testing, if indicated.
Therapy (Table 1.3)
| Enrofloxacin, pending results of culture and sensitivity | 5–15 mg/kg PO S-BID |
| Endoscopic-guided flushing of the ear canal under anaesthesia | |
| Support feeding | Oxbow Critical Care, approximately 100 ml in small frequent feedings; decreases as rabbit’s appetite improves |
Additional diagnostic testing
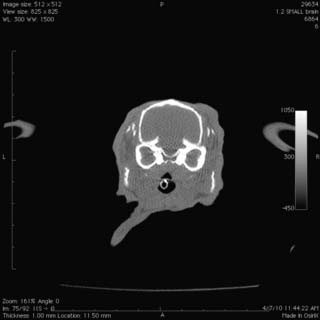
![]() 5. What is your interpretation of the computed tomography image presented in Fig. 1.9?
5. What is your interpretation of the computed tomography image presented in Fig. 1.9?
![]() 6. What are your recommendations for further therapy for this patient?
6. What are your recommendations for further therapy for this patient?
Chow E.P., Bennett R.A., Dustin L. Ventral bulla osteotomy for treatment of otitis media in the rabbit. J. Exot. Pet Med. 2009;18(4):299–305.
Deeb B.J., Carpenter J.W. Neurologic and musculoskeletal diseases. In: Quesenberry K.E., Carpenter J.W. Ferrets, Rabbits and Rodents, Clinical Medicine and Surgery. second ed. St Louis: Saunders; 2004:203–210.
Case 1.4
Radiology
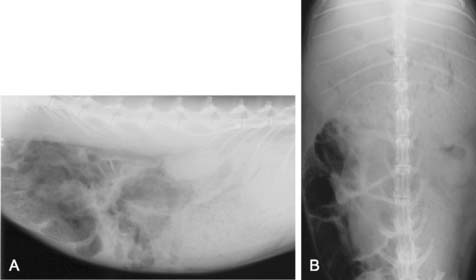
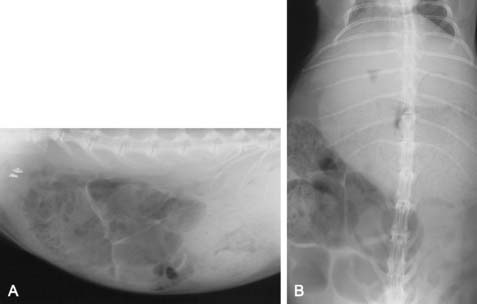
![]() 1. What is your interpretation of the radiographs in Fig. 1.10a, b? Note that patient size precluded inclusion of the entire abdomen in a single view.
1. What is your interpretation of the radiographs in Fig. 1.10a, b? Note that patient size precluded inclusion of the entire abdomen in a single view.
Clinical diagnosis laboratory examination
Blood was obtained from the lateral saphenous vein, and an in-house biochemistry was obtained, along with a blood film and haematocrit. Evaluation of the blood film, and the haematocrit were unremarkable (Table 1.4).
Table 1.4 Blood chemistry values of the rabbit
| Analysis | Results | Reference values |
|---|---|---|
| Albumin (g/l) | 4.4 | 2.4–4.6 |
| ALP (U/l) | 25 | 4–16 |
| ALT (U/l) | 1025 | 48–80 |
| Bilirubin (mg/dl) | 0.6 | 0.0–0.7 |
| Calcium (mg/dl) | 13.8 | 5.6–12.5 |
| Phosphorus (mg/dl) | 6.2 | 4.0–6.9 |
| Creatinine (μmol/l) | 2.1 | 0.5–2.5 |
| BUN | 30 | 13–29 |
| Glucose (mg/dl) | 235 | 75–155 |
| Total protein (g/l) | 6.0 | 5.4–8.3 |
| Globulin (g/dl) | 1.6 | 1.5–2.8 |
![]() 2. What is your interpretation of the findings of the results of blood analysis?
2. What is your interpretation of the findings of the results of blood analysis?
Therapy (Table 1.5)
| Analgesia | Buprenorphine: 0.01–0.05 mg/kg Butorphanol: 0.2–0.4 mg/kg Hydromorphone: 0.1 mg/kg As gastrointestinal disease can produce pain in rabbits, analgesia is an important part of therapy. Opioids appear beneficial for this purpose. While there is concern opioids may negatively impact the gastrointestinal tract, it should be kept in mind that pain and discomfort are potent inhibitors of motility |
| Fluid therapy | Place IV catheter and determine crystalloid fluid rate based on estimated dehydration with addition of maintenance requirements. Replace dehydration needs over 12 hours, as losses are assumed to be acute. Re-evaluate fluid needs every 8–12 hours |
| Motility modifiers | Cisapride: 0.5 mg/kg PO GID Trimebutine |
| Support feeding | Oxbow Critical Care 300 ml/24 hours in small frequent meals |
Radiology interpretation
 Increasing size of fluid-filled stomach; stomach is taking a more rounded appearance
Increasing size of fluid-filled stomach; stomach is taking a more rounded appearance
 Increasing amounts of gas in caecum and lower intestine, which is more apparent in the lateral view
Increasing amounts of gas in caecum and lower intestine, which is more apparent in the lateral view
At this point abdominal ultrasound and exploratory surgery were declined and euthanasia elected.
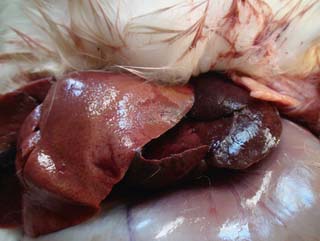
Post-mortem findings
The rabbit was euthanased and necropsy performed in-house (Fig. 1.12). The stomach was enlarged, and fluid-filled with mild serosal haemorrhages. The lower GI was partially filled with gas. There was no evidence of obstruction.
![]() 6. What additional lesions can you observe in the post-mortem image (see Fig. 1.12)?
6. What additional lesions can you observe in the post-mortem image (see Fig. 1.12)?
Case 1.5
Clinical history
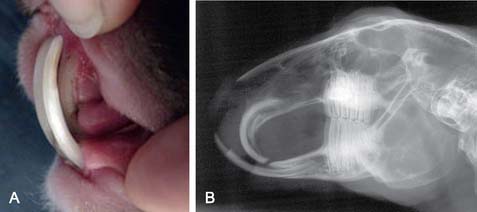
A 5-month-old rabbit weighing 1.8 kg was presented with the following clinical signs and symptoms:
• Decreased appetite and reluctance to eat hay or greens
• Visible overgrowth of the incisors that were protruding from the mouth.
Clinical diagnosis examination
Results
 Radiographs demonstrate elongation and malocclusion of the primary maxillary and mandibular incisors. Cheek teeth arcades are unremarkable
Radiographs demonstrate elongation and malocclusion of the primary maxillary and mandibular incisors. Cheek teeth arcades are unremarkable
![]() 3. List your differential diagnoses.
3. List your differential diagnoses.
Therapy (Table 1.6)
| Incisor extraction | |
| Assist feeding | Herbivore Critical Care (Oxbow Pet Products, Murdock NE) as needed after surgery and into healing period until eating well on own |
| Analgesia | Opioid as part of pre-anaesthesia and during immediate post-surgery period for up to 24 hours Buprenorphine: 0.06 mg/kg q6–8 h Hydromorphone: 0.10 mg/kg q6–8 h Meloxicam 0.4 mg/kg PO for 2–3 days post-surgery, and then PRN |
Discussion
Congenital jaw malformation is well described in rabbits and may represent a mandibular prognathism or maxillary brachygnathism. This malformation results in an abnormal occlusal plane and the inability of the incisors to wear normally upon each other, resulting in elongation, which can be extreme. Patterns of elongation vary but, in the rabbit, mandibular incisors typically elongate rostrally while maxillary incisors begin to curve caudally as they encounter the elongated mandibular incisors. Elongation may or may not result in perforation of soft tissues. Rabbits readily adapt to malocclusion and will continue to eat until the disease is severe. The best option for treatment of this condition is extraction of the incisors (Fig. 1.15). The technique is well described, and generally tolerated well. Prehension of food is performed with the lips and tongue; therefore rabbits are able to eat a normal diet, including hay. The loss of incisors, however, results in inability to cut larger food items into small pieces for prehension, for example whole carrots and large greens. These rabbits are also unable to cut naturally growing greens from the ground when foraging outdoors. These disabilities are minor and do not result in impacted quality of life.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree