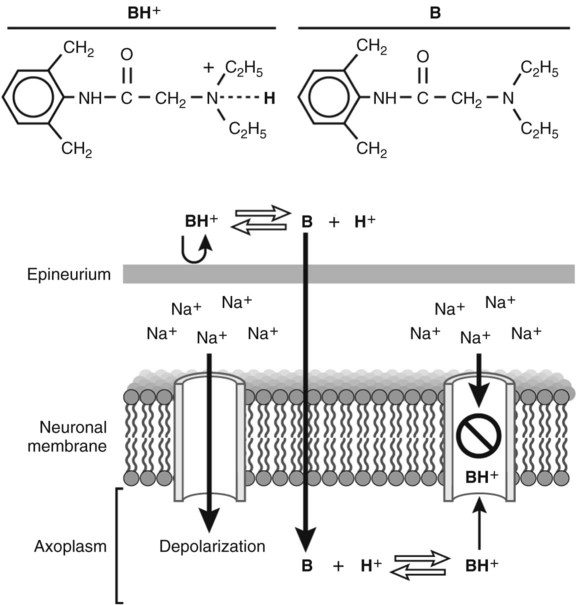
4 I Mechanism of membrane and impulse conduction A Local anesthetics are membrane-stabilizing agents B The drugs enter and occupy (by polar association) the membrane channels through which sodium (Na+) ions normally move C The most immediate and apparent effect is the prevention of the inflow of Na+ blocking subsequent ionic flow D Nerve cell depolarization is prevented, thus retarding or stopping the conduction of nerve impulses A The salt of the local anesthetic base is an ionizable quaternary amine with little or no anesthetic properties of its own 1. Local anesthetics are formulated as salts because salts are water soluble 2. Salts are not lipid soluble B Once the salt of the anesthetic base is deposited into tissues, it dissociates, and the anesthetic base (B) is liberated as follows: C The free anesthetic base is absorbed at the outer lipid nerve membrane. The anesthetic base combines with a hydrogen ion inside the nerve cell and blocks Na+ channels (Fig. 4-1). D Effect of tissue pH; the acid ionization constant (pKa) values of local anesthetics are usually between 8 and 9 (except for benzocaine: 2.9) IV Classification and function of nerve fibers (Table 4-1) TABLE 4-1 Classification of Nerve Fibers B Myelinated B-fibers: preganglionic sympathetic C Nonmyelinated C-fibers transmit V Sensitivity to local anesthetic effects (least resistant to most resistant) A C-fibers >Aδ-fibers > Aα-fibers B Sensation disappears in the following order: pain, cold, warmth, touch, joint, deep pressure C Motor function can be maintained after all sensation is lost A Potency is related to lipid solubility: local anesthetics with high lipid solubility have more potent effects B Latency is the time between injection and the peak effect 1. Binding affinity to receptor protein; local anesthetics with greater protein-binding ability have a longer duration of action; can bind to the receptors in Na+ channel reliably (bupivacaine, ropivacaine > tetracaine > lidocaine > procaine) 2. Doubling the concentration of local anesthetic increases the duration of analgesia by approximately 30% (proportional to the logarithm of the concentration) D Recovery time is the time it takes for normal sensation to return VII Ampules of hydrochloride salts can be autoclaved at 120° C for 20 to 30 minutes without affecting potency A Vasoconstrictors delay absorption, reducing toxicity and increasing the margin of safety B Vasoconstrictors increase intensity and prolong anesthetic activity (up to five times) C Use of vasoconstrictors may cause disturbances of the circulation (e.g., toes, penis, ears) D Vasoconstrictors can increase risk of cardiac arrhythmias and ventricular fibrillation A Increases tissue penetration (may double), resulting in a larger total area being desensitized B Often produces a rapid onset of analgesia C Usually shortens anesthesia time because of increased absorption, unless a vasoconstrictor is also used D May enhance systemic absorption and toxicity E Is not a substitute for precise, accurate technique; fascial planes are barriers to diffusion F Dose: use five turbidity-reducing units per milliliter of local anesthetic solution I Ester-linked drugs (Table 4-2) TABLE 4-2
Local Anesthetic Drugs and Techniques
Overview
General Considerations
Local Anesthetics
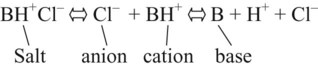
Fiber Name
Anatomic Location
Fiber Type and Diameter
Function
Sensitivity to Block
A-FIBERS
MYELINATED
Aα
Efferent and afferent to muscles and joints
6-22 µm
Motor, proprioception
+
Aβ
Efferent and afferent to muscles and joints
6-22 µm
Motor, touch, proprioception
++
Aγ
Efferent to muscle spindle
3-6 µm
Pain, temperature, muscle tone
++
Aδ
Sensory roots
1-4 µm
Pain, temperature, muscle tone
+++
B-FIBERS
Preganglionic sympathetic
<3 µm myelinated
Vasomotor, visceromotor
++++
C-FIBERS
Postganglionic sympathetic, sensory roots
0.4-1.2 µm nonmyelinated
Vasomotor, visceromotor, pain, temperature, touch
++++
Drugs Used for Vasoconstriction
Drugs Used To Hasten the Time of Anesthesia Onset
Specific Local Anesthetic Drugs
Agent (Generic Name)
Trade Name (Registered by)
Chemical Name
Potency Ratio (Procaine = 1)
ESTERS
Procaine
Novocain (Winthrop Stearns)
Para-aminobenzoic acid ester of dimethylaminoethanol
1 : 1
Tetracaine
Pontocaine (Sanofi)
Para-butylamino benzoyl- dimethylaminoethanol-HCl
12 : 1
Benzocaine
+ Butamben
+ Tetracaine
Cetacaine (Cetylite Industries)
Ethyl 4-aminobenzoate (benzocaine)
4-aminobenzoic acid butyl (butamben)
AMIDES
Lidocaine
Xylocaine (AstraZeneca)
Diethylaminoacet-2,6 xylidide
2 : 1
Mepivacaine
Carbocaine (Winthrop Laboratories)
1-methyl-2′,6′-pipecoloxylidide monohydrochloride
2.5 : 1
Bupivacaine
Marcaine (Breon Laboratories)
1-butyl-2′,6′-pipecoloxylidide-HCl
8 : 1
Ropivacaine
Naropin (AstraZeneca)
S-(-)-1-propyl-2′,6′-pipecoloxylidide-HCL monohydrate
8 : 1
Lidocaine
+ Prilocaine
EMLA cream (AstraZeneca)
Propylamine-2-methyl- propionanilide hydrochloride (prilocaine)
Drug
Toxicity Ratio (Procaine = 1)
Dose (%)
Stability
Comment
ESTERS
Procaine
1 : 1
1-2 for infiltration and nerve block
Aqueous solutions are heat resistant, decomposed by bacteria
Hydrolyzed by liver and plasma esterase
Tetracaine
10 : 1
0.1 for infiltration and nerve block; topically 0.2
Crystals and solutions should not be autoclaved
Slow onset of anesthesia (5-10 min); 2 hr duration; for eye instillation
Benzocaine
+ Butamben
+ Tetracaine
Keep away from flames, high temperature, alkali or alkaline earth metals, oxidizing agents
Never use for injection; rapid onset (30 sec); 30-60 min duration; may cause methemoglobinemia (mostly cats)
AMIDES
Lidocaine
0.5% 1 : 1
1% 1.4 : 1
2% 1.5 : 1
0.5-2.0 for infiltration and nerve block; topically 2-4
Aqueous solutions are thermostable; multiple autoclaving possible
Excellent penetrability; rate of onset twice as fast as procaine; 2 hr duration with epinephrine
Mepivacaine
Less toxic than lidocaine
1-2 for infiltration and nerve block
Resistant to acid and alkaline hydrolysis; can autoclave multiple times
Absence of vasodilator effects makes addition of a vasoconstrictor unnecessary
Bupivacaine
Greater margin of safety than lidocaine
0.25 for infiltration;
0.5 for nerve block;
0.75 for epidural block
Stable compound
Intermediate onset, lasting 4-6 hr
Ropivacaine
Greater margin of safety than bupivacaine
0.2 for infiltration;
0.5 for nerve block;
0.75 and 1.0 for epidural block
Stable compound
Intermediate onset, lasting 4-6 hr
Lidocaine
+ Prilocaine
(Do not spread out; apply a thick layer of medicine)
Possibility of skin trouble, deterioration of methemoglobinemia ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree