CHAPTER 20 Inflammation of the Tubular Reproductive Tract of the Mare
A broodmare needs to produce consistently viable foals to be economically successful. In order to achieve this she needs to be in good physical condition, have regular estrous cycles, mate, conceive, maintain pregnancy, give birth, and raise a foal. If there is a breakdown in any of these areas, she will become considered a “problem” mare. Consideration of management practices and fertility of the stallion is therefore important before all the blame of subfertility or infertility is placed on the mare. The tubular part of the reproductive tract is composed of the vulva, vestibule, vagina, cervix, uterus, and oviducts. All work together to provide the most conducive environment for fertilization, embryonic development, and the birth of a healthy foal. Inflammation of one of these components affects the others.
VAGINITIS AND CERVICITIS
The mare’s reproductive tract resides in the caudal portion of the abdomen suspended from the body wall by the broad ligaments. As the number of estrous cycles and foals produced increases so does the laxity of these ligaments causing the reproductive tract to lie more cranial and ventral to the pelvis. Three major anatomic barriers protect the uterine environment: the vulva, labia, vulvovaginal fold (hymen), and the cervix.1,2 Fertility problems begin to arise in the mare when these anatomic barriers are compromised or fail. This leads to contamination of the reproductive tract by air, urine, or particulate matter, causing pneumovagina, vaginitis, cervicitis, and endometritis.
The vagina and uterus are believed by some investigators to have a normal bacterial flora considered to be nonpathogenic, whereas others assume that the uterus of the clinically normal mare is bacteriologically sterile.3 Whichever the viewpoint, clinical vaginitis and cervicitis is most commonly due to irritation from air, urine, particulate matter (bacteria), or chemicals including antibiotics and antiseptics and are usually associated with endometritis.4–6 The vulvovaginal fold, rather than the cervix, has been indicated as the major barrier to ascending bacterial contamination of the mare’s reproductive tract.3 Speculum examination reveals a hyperemic mucosa of the vaginal vault and cervix with or without exudate or urine crystals on the ventral aspect, depending on the cause. Treatment is focused on reconstructing the physical barriers to include Caslick’s procedure, perineal body reconstruction, repair of perineal lacerations and rectovaginal tears, and urethral extensions.1,4 These steps will remove the offending source of irritation or organisms allowing for the vaginitis and cervicitis to resolve. If the underlying problem is endometritis, intrauterine or systemic treatment with an appropriate antibiotic or discontinuation of uterine treatment of irritating antibiotics (enrofloxacin, ceftiofur) or antiseptics (Nolvasan, concentrated iodine solutions) resolves the secondary vaginitis as long as permanent damage such as adhesions has not occurred.7
ENDOMETRITIS
After fertilization occurs in the oviduct, it takes 5 to 6 days for the embryo to descend into the uterus.8 Therefore, in order for the embryo to continue to develop, the uterus needs to provide a conducive environment for growth, free of inflammation and contamination. Endometritis is an inflammation of the endometrium of the uterus. It has been described as being the third most important clinical problem in equine practice after colic and respiratory tract disorders.9 As previously described, endometritis is often seen in conjunction with vaginitis and cervicitis, when compromise to the physical barriers or contamination during breeding occurs,10–12 and is associated with infertility in the mare.13,14 Mares have been classified depending on their ability to clear their uterus in a certain amount of time when challenged with infection as susceptible or resistant.15 Normal/resistant mares are able to clear their uterus from infection or inflammation by three mechanisms: uterine contractions, lymphatic drainage, and an open cervix.16–19 Antibody-mediated uterine defense appears to be functional in susceptible mares, and although polymorphonuclear neutrophils (PMNs) are not dysfunctional, susceptible mares were found to have impaired phagocytosis as a result of insufficient opsonization in uterine secretions.10,20 The breakdown in uterine physical clearance mechanisms is currently believed to play a major role in susceptibility to persistent endometritis.16 Further identification of these mares has been established by using scintigraphy and ultrasonography in which impaired or reduced myometrial contractility in response to acute inflammation results in an accumulation of fluid and inflammatory products within the uterine lumen.10,21–24 Additional factors including vascular degenerative changes and dependent position of the mare’s uterus have also been implicated in interfering with effective clearance of the uterus.10,21,25
Based on the current literature, persistent endometritis can therefore be divided into (1) sexually transmitted diseases (STDs), (2) chronic infectious endometritis, (3) persistent breeding-induced endometritis, and (4) chronic degenerative endometritis (endometriosis).10
SEXUALLY TRANSMITTED DISEASES
Taylorella equigenitalis is the causative organism of contagious equine metritis (CEM). T. equigenitalis is a gram-negative coccobacillus that is transmitted venereally and is highly contagious in equines. CEM was first documented 25 years ago in Newmarket, England. CEM has now been reported in horses worldwide. In July 1977, CEM was reported on 28 breeding farms in the Newmarket area, with approximately 200 Thoroughbred mares and 23 stallions affected.26 By the conclusion of the 1978 breeding season, CEM was diagnosed in numerous countries, including the United States and Australia.27 T. equigenitalis has now been isolated in 14 countries, infecting both Thoroughbreds and non-Thoroughbreds.28
In 1978, two strains of the organism were isolated from Kentucky Thoroughbreds.29 One strain was sensitive to streptomycin and the other was resistant. In 1979, Missouri reported an outbreak of CEM in non-Thoroughbreds involving the streptomycin-sensitive strain.
Mares diagnosed with CEM reportedly exhibit shortened diestrous periods and copious mucopurulent vulvar discharges lasting up to 14 days. Stallions covering infected mares were asymptomatic. Numerous cultures were taken without isolating T. equigenitalis until fresh cultures were placed in transport medium and grown on chocolate blood agar incubated at 37° C in 5% to 10% carbon dioxide for 48 hours.30 T. equigenitalis was found to be sensitive to a wide range of antibiotics and antiseptics, including benzyl penicillin, ampicillin, and chlorhexidine, but was resistant to streptomycin.27
A code of practice was issued in 1977 to control the spread of CEM. The code was published in the United Kingdom and similar measures were taken in Ireland and France. The code stipulated a mare as high risk if she cultured positive for CEM, was covered by an infected stallion, or if she arrived from outside the United Kingdom. The code mandated that high-risk mares should have a negative clitoral culture before and after arrival at stud and a negative endometrial and clitoral culture during estrus prior to breeding. Low-risk mares were required to have a negative clitoral swab taken before or after arrival at stud, providing there was agreement with the stud farm manager.31 The code further stipulated that stallions should be cultured from pre-ejaculatory fluid, the penile sheath, the urethra, and the urethral fossa, and that all cultures should be sent to designated laboratories and incubated under microaerophilic and aerobic conditions. As a result of this code of practice, the incidence of CEM has decreased. Owing to strict importation regulations in the United States, CEM has not been reported in this country since 1983.32
Etiology
In 1978, the initial bacteriologic examination of swabs from the genitourinary tracts of infected animals revealed the CEM organism to be Haemophilus equigenitalis strain NCTC1/184 (61717/77). The organism was renamed Taylorella equigenitalis in 1984.33
Transmission
Spread of CEM is primarily by venereal contact. Contaminated equipment, instruments, and personnel that contact the genital tracts of mares and stallions contribute to the spread of the disease. A carrier state exists because T. equigenitalis persists indefinitely in the clitoral sinuses of mares and urethral fossae of stallions. T. equigenitalis has been isolated from foals born to infected mares.34 T. equigenitalis has been isolated also from an aborted fetus and placenta, but a repeated culture of the dam did not reveal the organism.35
Diagnosis
Cultures should be taken during early estrus from the endometrium or cervix. Cultures from the clitoral fossa and the three clitoral sinuses should be submitted. The clitoral sinuses are small and can be visualized when the clitoris is partially extruded and held downward. A small swab moistened with sterile saline can be used to sample the sinuses. Clitoral cultures can be obtained at any time during the estrous cycle and from pregnant mares. A stallion’s penis must be extended and samples taken from the urethral fossa, urethra, preputial folds, skin of the penis, and pre-ejaculatory fluid.28 Three negative cultures should be taken before the stallion is considered free of the disease.
Serology
Numerous serologic tests have been developed to detect antibodies to CEM in serum. The enzyme-linked immunosorbent assay (ELISA) and passive hemagglutination tests are superior for detection of infected mares.28 Antibodies can be detected within 40 days of infection. The tests are useful in identifying mares with active infections. Carrier mares and infected stallions have no humoral response, and serologic tests are of little value as screening tests. Taylorella asinigenitalis and B. ureolyticus have shown such similarity in morphology and phenotype that there have been problems in the identification and conformation of T. equigenitalis.36,37 The culture LightCycler PCR eliminates the confusion because it does not amplify B. ureolyticus DNA and discriminates from T. asinigenitalis.38 Therefore, it can be used in conjunction with culture to fulfill export criteria and improve specificity and sensitivity.
Control
The code of practice instituted in 1977 for the control of CEM has dramatically reduced the incidence of the disease. Sporadic outbreaks have occurred that can be traced to carrier animals.39 Carriers are considered high-risk animals and are treated and followed with extensive bacteriologic cultures until they are found to be negative. Continued vigilance against inapparent carrier animals has prompted countries, including the United States, to institute strict import regulations. Mares and stallions imported from countries not declared free of CEM must undergo quarantine and extensive testing at a designated quarantine station.39
Treatment
Intrauterine infusion of antibiotics combined with thorough cleansing of the clitoris, clitoral fossa, and clitoral sinuses is the treatment of choice in mares. Daily intrauterine infusions for 5 to 7 days with penicillin (5 to 10 million U), ampicillin, neomycin, and nitrofurazone have been reported to be successful.28 The clitoral body, the fossa, and the sinuses must be thoroughly scrubbed daily for 5 days with 4% chlorhexidine solution and packed with nitrofurazone or chlorhexidine ointment. Clitoral sinusectomy might be recommended in mares that continue to harbor CEM in the clitoral area following treatment.
ENDOMETRIOSIS
Endometriosis is a chronic degenerative condition of the endometrium.40,41 It occurs in older mares that have been exposed to repeated inflammatory conditions or aging.41 These severe changes can be a sequela of vesicovaginal reflux (urine pooling), chronic bacterial contamination, or delayed uterine clearance with inflammatory byproducts remaining in the uterine lumen. Unfortunately, the process has been found to be irreversible and untreatable and those mares that do get in foal have a harder time maintaining the pregnancy to term.
CHRONIC INFECTIOUS ENDOMETRITIS
Chronic endometritis is a major cause of equine infertility in older and multiparous mares. These mares become contaminated either during breeding or due to anatomic defects of the perineal and vulvar region leading to pneumovagina and fecal aspiration.42 The most common organisms found in persistent endometritis are Streptococcus zooepidemicus, Escherichia coli, yeasts (Candida spp. and Aspergillus spp.), Klebsiella pneumoniae, and Pseudomonas aeruginosa.43,44 Anaerobes have also been described as possibly playing a role.45 In addition, the unique property of S. zooepidemicus enables it to physically adhere to the endometrium in susceptible mares with an increased appearance noted in mares with category 3 endometria.46
It is thought that in some mares with delayed uterine clearance, defective uterine immune defense mechanisms may contribute to persistence of infection.47 Neutrophils need to migrate from the blood into the uterine lumen, phagocytose, and kill bacteria appropriately. Defects in the migration of blood-derived neutrophils have not been found in susceptible mares and factors in uterine secretions of susceptible mares have been determined to interfere with neutrophil phagocytosis rather than an innate phagocytic failure.17,48 Opsonization by uterine secretion is dependent on both complement and specific antibody; and although a deficiency in complement was suggested to contribute to uterine defense failure, hemolytic complement was recognized to be elevated in flushings from susceptible mares.49–52 Specific endometrial antibodies are important in the elimination of bacterial infection with their opsonic activity differing between susceptible and resistant mares.53–55
Cellular immunity has not received much attention in the equine uterus, although susceptible mares have normal macrophage function and no deficiency of T lymphocyte subsets.15 A deficiency in antigen processing and handling at the uterine level may be due to a lack of an appropriate increased response of macrophages.15
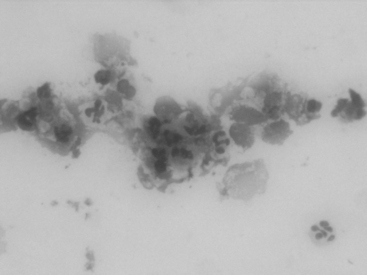
Documentation of inflammation in the uterine lumen and accurate proof of an infectious organism is imperative.56 In mares with infectious endometritis, the vaginal vault and cervix appear hyperemic on speculum examination with or without the presence of exudate. Rectal palpation may reveal a large relaxed uterus, and transrectal ultrasonography may show flocculent intraluminal fluid accumulation, the extent of which is dependent on the causative agent and severity. Endometrial cytologic examination is the diagnostic test of choice because it provides direct evidence of the presence of neutrophils in the uterine lumen. Any mare that has more than 5 neutrophils per high-powered field confirms active inflammation56 (Fig. 20-1). Cytologic samples can be acquired by a guarded endometrial swab; collecting cells from the cap of a calajan culturette; or a small sterile guarded atraumatic brush or small volume uterine flush. Care must be taken to roll, not smear, the cells so as not to damage them. A representative sample contains both endometrial and inflammatory cells, with the best results obtained from centrifugation of a small volume uterine flush.57 Blood contamination can produce a false positive cytologic finding. A guarded uterine culture confirms the causative organism and the antibiotic sensitivity patterns help to direct the treatment. The course of therapy undertaken will be determined by the cause of inflammation.
The goal of therapy for bacterial endometritis is to remove the offending bacteria and enhance uterine defense mechanisms, thereby decreasing the inflammatory process within the uterus. This has been accomplished with intrauterine infusions of antibiotics, antiseptics, and plasma; uterine lavage; ecbolics; and systemic antibiotic therapy. Therapy can be completed before or after breeding, depending on the severity of the infection. It is important to tailor the therapy to the individual case and to remember that no single treatment can be effective in all cases. With severe infections, multiple therapeutic approaches can be used to control the infection. This discussion attempts not to define a course of treatment but to illustrate successful and commonly used treatments. Every mare is an individual and the routine treatment of all mares with the same medication will not result in the best treatment.58
Intrauterine Therapy
A common form of therapy is intrauterine infusion of antibiotics, chemicals (antiseptics), and plasma.59 Intrauterine infusion concentrates medication locally in the infected endometrium as opposed to systemic treatment, which relies on blood concentration of the drug.
For intrauterine antibiotic therapy, a drug should be selected on the basis of sensitivity tests. Broad-spectrum antibiotics might not be as effective as bactericidal antibiotics. Bacteriostatic drugs require assistance from the mare’s defense system, which is likely compromised as indicated by the presence of infection.59 Drug combinations should be avoided because incompatibility often renders the drugs ineffective. The same is true of drug and antiseptic combinations.58
The antibiotics most commonly used for intrauterine therapy are penicillin, gentamicin, ampicillin, nitrofurazone, polymyxin B, Timentin, ticarcillin, the sulfonamides, and amikacin.58,60 Gentamicin, amikacin, ampicillin, and Timentin are the most effective against the majority of pathogenic organisms. Penicillin is thought to be one of the most effective antibiotics available for treating equine uterine infections.58
Antibiotics infused into the uterus are dissolved or suspended in sterile water or saline solution and infused directly into the uterus daily for 3 to 5 days or more during estrus.56
The size of the uterus, determined by transrectal palpation, should be used to determine the volume infused. The antibiotic can be suspended in volumes between 60 and 100 ml based on the assumption that this volume is optimal for coating the endometrial surface; however, the effects of such dilution on antibiotic efficacy are unknown. Present evidence suggests that most of the antibiotic introduced in this manner is expelled through the cervix soon after treatment.56,59,61
Intrauterine antibiotic therapy is not without risk. Indiscriminate use of antibiotics may alter the normal uterine flora and result in development of resistant strains of bacteria, yeast, and fungi.58,62 Some mares are sensitive to particular antibiotics.56 Caution must be used to ensure that therapy does not pose a greater threat than infection. The use of products not approved for intrauterine infusion can cause harmful effects in mares.58
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree