CHAPTER 77 Infectious Causes of Abortion
The female goat is normally a very fertile animal1,2; however, goats have a high incidence of abortion when compared with other farm animals. Infectious causes of abortion play an important role and could be a major source of economic loss in a goat herd. In an abortion outbreak, the safest approach is to assume that all causes of abortion are infectious in nature and to proceed from there.3,4 Several microbial agents have been incriminated as causes of abortion in the goat, but the most common ones are Chlamydia psittaci, Toxoplasma gondii, Campylobacter spp., Mycoplasma spp., Coxiella burnetii, and Brucella melitensis. In the United States, chlamydiosis and toxoplasmosis are the most frequently identified infectious causes of caprine abortion.5,6 In a study of 1784 abortion and stillbirth specimens submitted during a 10-year period, T. gondii, Campylobacter spp., and C. psittaci caused about 25% of all abortions in sheep.7 Many of the organisms that cause abortion in sheep also cause abortions in goats, with the exception of campylobacteriosis, which is rare in goats in North America.6
The lesion common in all cases of infectious abortion is placentitis. Because of placentitis, the fetus either dies due to inability to exchange nutrients through the placenta, or becomes infected and dies.4 Economically and emotionally, midterm or late abortions are of great concern to the owner, whether the animal is on a commercial or hobby farm, because the fetuses are lost and the unproductive female must be maintained until next breeding season or sold at a loss. A prolonged period of uterine disease and infertility may follow and in cases of infectious abortion, the disease threatens the rest of the herd.8
This section reviews the most common infectious causes of fetal loss in the goat.
CHLAMYDIOSIS
Chlamydiosis is the most common cause of infectious abortion in goats in the United States.4,9 The disease is also one of the major causes of reproductive wastage in sheep breeding.10 The disease has been described in Scotland, England, and in the western United States.11 Chlamydia also causes pneumonia, keratoconjunctivitis, epididymitis, and polyarthritis in sheep and goats.8,10,12,13
Etiology
C. psittaci, a gram-negative, intracellular organism that contains both RNA and DNA, is the agent responsible for chlamydiosis.5 This organism was established as the causative agent of enzootic abortion of ewes in the late 1950s.14
The antigenic strains found in goats appear to be closely related to those in sheep. Antigenic type 1 is implicated in abortions, birth of stillborn or weak kids, and in neonatal chlamydial pneumonia, whereas type 2 isolates cause polyarthritis and conjunctivitis in adult goats.15–17 Serotype 2 has been recently reported as an abortion-inducing strain in ruminants as well.10 There is no cross protection between these two antigenic types.15
Epidemiology and Pathogenesis
Pigeons and sparrows can serve as reservoirs for the organism, and it has been suggested that ticks or insects may play a role in transmission of the disease.16,17 C. psittaci can persist in the feces of infected animals, which may explain why the infection carries over from one kidding season to the next.10,14 Aborting does shed large numbers of organisms from the uterine discharge, fetus, and placenta, particularly during the first 3 weeks after abortion. Elimination of chlamydiae from the uterus is complete within 3 months.18,19 Inflammation and necrosis caused by multiplication of the chlamydiae prevent normal transfer of nutrients across the placenta, and the fetus dies and is aborted.5 Does exposed to C. psittaci for the first time in the first half of gestation abort that pregnancy, whereas susceptible does exposed for the first time during the last half of pregnancy usually abort during the subsequent pregnancy.20 Regardless of the time of infection in the female, the organism does not begin to proliferate and attack the placenta until about day 90 of gestation.21 Even though chlamydiae have been isolated from the semen of experimentally infected rams for up to 29 days after inoculation, venereal transmission during breeding has not been investigated.16,17
There is no evidence of infertility during the subsequent breeding season in aborting does, and immunity after an abortion lasts about 3 years. Older does may abort because of chlamydiae repeatedly.4,9 Outbreaks of abortion among goats by co-infection with Coxiella burnetii have also been reported.22
Clinical Signs
In the United States, 25% to 60% of does in endemically infected herds that are kidding for the first time abort.9 Abortions usually occur during the last month of gestation but can occur as early as day 100 of gestation.4,8,18,19 Does are not normally ill but may show a bloody vaginal discharge 2 to 3 days prior to abortion. The fetus may be autolyzed or fresh. Some weak newborns are seen, and a few does may retain the placenta.4,9 Pathologic changes in the fetus are nonspecific. The fetus may be delivered in a fresh state but may be autolyzed if retained in the uterus for a day or two. The placenta shows regional to generalized placentitis (white to yellow necrotic areas) involving the cotyledons and intercotyledonary space.4,9
Diagnosis
Diagnosis is based on a history of abortion along with clinical signs and demonstration of characteristic inclusion bodies in impression smears of placenta, fetal tissue, or uterine discharge. A definitive diagnosis is made by culturing the organism from the placenta or fetal tissue.4,9,12,13 Serologic testing is also a valuable aid in diagnosis. Ewes, does, and cows have significant rises in antibodies against chlamydial antigen after abortion.23 Paired blood samples from the doe, 2 to 3 weeks apart, are necessary for serologic tests.4,13,14 Antibodies may be detected in fetal serum as well. The tests of choice are the enzyme-linked immunosorbent assay and the indirect inclusion fluorescent antibody test.23 Titers in the range of 1:32 to 1:256 suggest chlamydial infection. A fourfold increase in antibody titer between paired serum samples is significant.14
When chlamydiosis is suspected, the following samples should be submitted for diagnostic evaluation14:
Treatment and Control
Limited success has been achieved in controlling an outbreak by treatment of all females with tetracycline in the last 4 to 6 weeks of gestation.4,9,13 Suppression of the organism may prevent additional placental damage and also reduce shedding of chlamydiae by treated does. Large herds are commonly treated with oral tetracycline (400 to 500 mg per head per day) for 2 weeks.5,24 This would be a reasonable approach for fiber-producing does. In dairy herds, it is more customary to treat individual nonlactating does by injection of long-acting oxytetracycline at a dose of 20 mg/kg IM every 10 to 14 days.5 Other authors have given the drug twice a week in the last 4 to 6 weeks of gestation.4,9,13 Considering the management difficulties and cost associated with prevention, the most effective protocol appears to be one injection of long-acting oxytetracycline at 6 to 8 weeks prior to parturition, followed by a second injection 3 weeks after parturition.17
Enzootic abortion is of such serious economic consequence in some countries that compulsory government vaccination programs have been implemented.11 A killed vaccine for sheep is available in the United States and can be used in goats (extra-label use) but may cause a local as well as a systemic reaction for several days (marked soreness and stiffness).6,25 The vaccine is usually available only in combination with Campylobacter bacterin or Campylobacter and Escherichia coli bacterin (Campylobacter fetus–Chlamydia psittaci–Escherichia coli bacterin*).6,25 The vaccine should be given IM or SC 8 weeks prior to breeding and followed in 4 weeks with a second vaccination.25 Even though trials in sheep have shown that protection from abortion lasts for about 3 years, annual revaccination is recommended.25,26 Vaccination helps to prevent abortion, but it does not eliminate infection.5 Aborting does should be removed from the herd for at least 3 weeks, and the fetus and placenta should be burned or buried. Care must be taken to prevent contamination of feed and water. No feed should be given on the ground, and feeders should be designed to prevent goats from getting into them.11
Zoonotic Potential
Chlamydia psittaci is contagious to humans. During kidding season, pregnant women assisting with parturition may become infected and abort. An influenza-like syndrome has also occurred in men assisting with lambing in infected flocks.5 Veterinarians and farmers attending normal parturition, dystocias, or abortions should wear plastic gloves to limit exposure to uterine fluids. The same precautions apply when collecting fetuses or placentas for disposal or diagnostic evaluation. Pregnant women should avoid contact with the herd during the kidding season.5
TOXOPLASMOSIS
Toxoplasmosis is one of the most common parasitic infections in goats, other livestock, and humans worldwide.27,28 Toxoplasmosis is a major cause of abortion in sheep in New Zealand and England and is known to cause reproductive losses in goats and other animals.29
Etiology
The protozoan Toxoplasma gondii is the agent that causes abortion, mummification, stillbirth, and birth of weak kids in goats as well as in sheep.5,27
Epidemiology and Pathogenesis
Cats are pivotal in the transmission of T. gondii.30 They become infected by ingestion of infected rodents and birds, which can lead to excretion of large numbers of environmentally resistant oocytes. Transplacental infection can develop in cats, and kittens infected in utero can shed T. gondii oocytes after birth.30 Cats often defecate and bury their feces in the hay and food bins of barns. Does become infected by ingestion of food or water contaminated with oocytes from feces of infected cats. The organism enters the blood and spreads to other tissues within 2 weeks of ingestion of oocytes. In pregnant does, toxoplasmas can invade and multiply in the placenta and then spread to the fetus, causing abortion, fetal death, resorption of the fetus, stillbirth, birth of a live but weak kid, or birth of a normal kid, depending on the stage of pregnancy.27 Nothing is known about the breed susceptibility to toxoplasmosis in goats. Although T. gondii can be found in goat semen, it is doubtful that venereal transmission is important in causing abortion.28
Clinical Signs
Goats appear to be more susceptible to toxoplasma infection than sheep.31 Abortion can occur in does of all ages but primarily in does that acquire infection during pregnancy. Abortion may be repeated in the next gestation.28 The incidence of abortion in a flock may vary from 3% to 30%. Ewes and does infected prior to breeding do not abort. Those infected 30 to 90 days after breeding usually have fetal resorption or mummification. Most observed abortions occur in the last trimester of gestation, 2 to 3 weeks before term, after infection during the latter half of gestation.8 The does themselves are generally clinically normal at the time of abortion.28
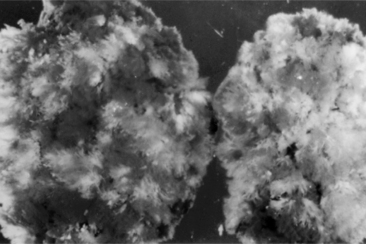
Abortion occurs because of necrosis of the placenta, particularly the cotyledons, or fever in the doe. The intercotyledonary areas of the placenta are usually normal, with the cotyledons having white to yellow focal areas of necrosis and calcification up to 1 cm in diameter (Fig. 77-1). These lesions are clearly visible when the cotyledons are washed in saline. The lesion is characteristic of only toxoplasmosis and can be used in the field as a diagnostic tool.4,8,13,28, On the other hand, C. burnetii, Brucella spp., and Chlamydia spp. usually cause placentitis that includes the intercotyledonary region.29
Diagnosis
Rapid diagnosis of infectious abortion in goats is important. Several tests are available for diagnosis. A presumptive diagnosis can be made from placental lesions alone; however, placenta often is not available for examination because it may be decomposed.31
The preferred diagnostic procedure is determination of T. gondii antibody in fetal fluids or presuckling serum. Their presence indicates transplacental toxoplasma infection.32 The absence of T. gondii antibody does not preclude the possibility of infection, however. It is important to ensure that serologic examination of kids is done before colostrum is given because the amount of antibody in colostrum is several times greater than that in serum and may cause high neonatal antibody titers.28 The presence of high antibody titers in doe serum is not necessarily diagnostic of recent infection because titers may remain high into the next breeding season. However, absence of antibodies is considered to be conclusive evidence that toxoplasmosis was not the cause of abortion.5,28 The modified agglutination test can be used to detect antibody in fetal and maternal serum. The modified agglutination test is easy to perform and more sensitive than other tests.32 The enzyme-linked immunosorbent assay and the indirect fluorescent antibody tests have also been used.28
Positive diagnosis of toxoplasmosis requires isolation of the organism from the placenta or fetal brain, lung, and muscles.32 The samples for isolation studies should be shipped on ice but not frozen.28
Treatment and Control
Control of toxoplasmosis is based on preventing exposure of goats to cat feces. Cats should be prevented from defecating in feeders or in hay. Fetal membranes and dead fetuses should be buried or incinerated to prevent infection of cats and other animals.30 Cats should not be allowed near pregnant sheep and goats, but in practice this is difficult.28,30 A vaccine that contains a strain of tachyzoites (S48) that do not persist in tissues of sheep is available in Europe and New Zealand, but it is not available in the United States. Ewes vaccinated with the S48-strain vaccine remain immune for at least 18 months.30 Breeding goats that have been exposed to T. gondii infection are likely to be relatively resistant to the effects of re-exposure during subsequent pregnancies and are less likely to abort again from this cause and therefore should not be culled.33
Zoonotic Potential
Fetal membranes and dead fetuses from sheep or goats that abort should be handled with caution by persons wearing gloves to prevent infection in humans.30 Toxoplasmosis has been reported in human beings after drinking raw goat milk. Therefore, goat milk should be pasteurized or boiled before human consumption. This is particularly true for its use in infants, who are more susceptible to toxoplasmosis than adults.34
Q FEVER
Query or Queensland fever is a zoonotic infection affecting a variety of animal species and human beings. It can be the cause of abortion in sheep and goats5,35 and has been reported in Canada, the United States, and many other countries.4,5,8,35,
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree