5 Immunology
Infection occurs when an organism becomes lodged in the host and begins to reproduce. There is a variable length of time from when infection occurs to when the animal starts to show clinical signs of disease; this is called the incubation period. Infected animals may be capable of infecting other animals during this time by expelling organisms into the environment with their breath or in body fluids. The acute period is the time during which clinical signs of the infection are at their height, and the decline period is the time during which signs are subsiding. The convalescent period is that time during which the animal’s body completely expels the organism and repairs body tissues damaged by the infection.
I. IMMUNOLOGY
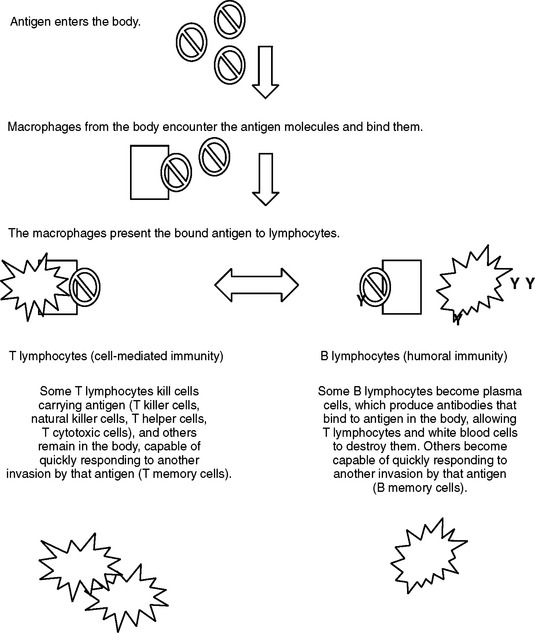
The body responds to the presence of an antigen in several ways (Figure 5-1). As an antigen enters the body, it is picked up by an immune cell called a macrophage. The macrophage binds to the antigen and presents it to another immune cell, a lymphocyte. There are two populations of lymphocytes and two types of response to the presence of the antigen, called the cell-mediated response and the humoral response.
Cell-mediated immunity is due to activation of T lymphocytes. Many different types of T lymphocytes are activated by the presence of the antigen, including T cytotoxic cells, T killer cells, natural killer (NK) cells, T helper cells, and T memory cells. Most of these cell types act by destroying the macrophage and attached antigen or destroying infected cells of the body that contain the antigen. T memory cells recognize the antigen and then go into “reserve,” remaining latent in the body until that animal is exposed to that same antigen another time.
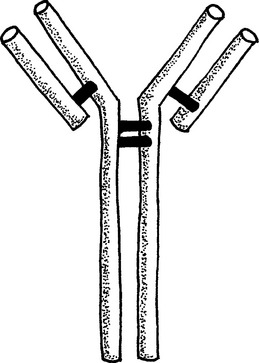
In dogs, four types of antibodies are produced. All antibodies are large, Y-shaped proteins (Figure 5-2). Immunoglobulin M (IgM) is produced first. It is a very large protein, which increases the speed with which it is recognized by phagocytic cells. Concentrations of IgM against a specific antigen fall fairly quickly. IgG is produced next. Concentrations of IgG get very high and remain high a long time after exposure of the animal to the antigen. IgE is the smallest of the antibody molecules and does not achieve high concentrations in the body. IgA is produced on surfaces that are exposed to the antigen directly, such as the mucous membranes of the respiratory tract, mouth, and urogenital tract. Concentrations of IgA are very high in secretions from these surfaces.
II. VACCINATION
The type of organism and amount of organism to which the animal is exposed alter the immune response and generation of adequate protection against subsequent exposure. If the “dose” of organism to which the animal is exposed is too small, there will be only a short-lived immune response and no memory cells will be formed. If the “dose” is too high, the immune system may be overwhelmed and the animal may become ill, still without generating an adequate response. Some organisms do not elicit a strong immune response; for example, bitches infected with canine herpesvirus do not have high concentrations of antibodies against herpesvirus for very long after exposure because the virus is not a very strong or reactive antigen.
The frequency with which animals need to be vaccinated to allow them to maintain a protective concentration of antibodies in serum varies with age of the animal, the type of vaccine used, and the animal’s responsiveness to the vaccine. At birth, puppies have few circulating antibodies in their bloodstream. Only about 3% of the antibodies they need to protect them from disease cross the placenta and are present at the moment of birth. Antibodies ingested passively in colostrum protect puppies until they can generate their own immune response at about 4 weeks of age. Puppies usually are immunized several times, with a 2- to 4-week interval, to ensure a good immune response. The factors that can prevent a good response are (1) our inability to recognize exactly at what time the animal becomes capable of responding to an antigen introduced by vaccination and (2) the presence of antibody from the dam, which will neutralize antigens introduced with the vaccine. Immunization of puppies is therefore a balancing act in which we try to promote the pup’s own immune response without allowing the concentration of antibody derived from the dam to fall so low as to risk the pup being exposed to disease without adequate protection. Because there is no good way to know whether or not a pup has responded to vaccination or whether it still has protection against disease from its dam, it is not recommended to expose pups to strange people or dogs much before vaccination at about 8 weeks of age. For most vaccines, it is recommended that pups be immunized at 8, 12, and 16 weeks of age. Some people prefer to begin vaccinating their pups at 6 weeks of age; the manufacturer’s recommendation always should be followed. The occasional puppy does not respond to vaccination; measurement of antibody concentration in serum 2 weeks after the final vaccination in the series may allow a veterinarian to determine whether the puppy is adequately protected or should receive another vaccination before the annual booster as an adult.
Puppies are capable of generating an immune response to more than one organism at a time. Some people worry about vaccinating pups too frequently and “overwhelming” their system. Anecdotal reports cite instances of autoimmune disease from too frequent vaccination; one lecturer stated that 1 of every 2500 dogs develops autoimmune destruction of red blood cells (autoimmune hemolytic anemia) after vaccination. There is no scientific documentation of this phenomenon. Vaccination failure may occur. This is defined as failure of the animal to generate a protective immune response after immunization (Table 5-1). It is thought that some animals may have a genetic predisposition to vaccination failure; no genetic test for such is available at this time.
Table 5-1 Types of Vaccine Failure
| Type of Vaccine Failure | Possible Causes |
|---|---|
| Failure to induce antibody production | Antigen dose is too small |
| Passive immunity present from dam, neutralizing antigen introduced in vaccine | |
| Mixing of vaccines, allowing component in one vaccine to inactivate another vaccine | |
| Genetic predisposition to vaccination failure | |
| Failure to induce long-lasting immunity | Antigen dose is too small |
| Killed vaccine product | |
| Induction of disease in vaccinated animal | Organism in vaccine not completely killed or modified |
| Animal infected with another virus at vaccination, allowing modified or killed virus to reproduce | |
| Vaccine contaminated with another microorganism | |
| Killed or modified product mutated | |
| Induction of antibodies that are not protective against the disease | May have antibodies in the bloodstream that cannot protect against invaders at the body surface |
| Induction of antibodies against the wrong virus |
It is understood that if enough animals are vaccinated, the overall incidence of disease will decline and animal health will improve (“herd health”). However, some animals respond poorly to vaccination and owners question whether it is necessary to regularly vaccinate their individual animal to help maintain health of the dog “herd” in their area.
Too frequent vaccination has been hypothesized to cause an actual decrease in the ability of the body to respond to immunization; high concentrations of antibody in an adult animal may neutralize vaccine just like passive antibodies do in puppies. Dogs may be allergic to adjuvants or preservatives in vaccines, some to a life-threatening extent. Occasionally the dog acquires the illness from the vaccine; it is reported that 1 in 10,000 to 50,000 dogs (depending on the type of organism used in the vaccine) develops disease from canine distemper vaccine (see Table 5-1). Formation of a mass or localized hair loss may occur at the site of vaccination. Some authors contend that too frequent administration of vaccinations may induce autoimmune disease in dogs, in which the immune system destroys normal body cells, such as red blood cells. In cats, tumor formation at the site of some vaccinations is a well-documented phenomenon. For these reasons, several alternatives to annual vaccination have been proposed.
The American Animal Hospital Association (AAHA) has suggested that vaccination every 3 years is probably adequate for most adult pet dogs. Dogs that have greater exposure to disease should be vaccinated more frequently. The AAHA breaks down vaccines into two classifications: core and noncore (Table 5-2). Core vaccines are those that should be given regularly to all dogs. Noncore vaccines are those that need not be given to all dogs but may be necessary in an individual dog or kennel, depending on likelihood of exposure. In 2004 the Food and Drug Administration approved the first 3-year core vaccine, Duramune Adult, from Fort Dodge Animal Health, which is intended for vaccination of adult dogs against canine distemper, parvovirus, and adenovirus.
Table 5-2 Core and Noncore Vaccines for Dogs
| Vaccine | Associated Disease | Incubation Time* |
|---|---|---|
| CORE VACCINES | ||
| Canine distemper virus (CDV) | Fever, diarrhea, squinting, nasal discharge, later neurologic signs | 9 days to 12 wk |
| Canine adenovirus-2 (CAV-2) | Hepatitis; vomiting, diarrhea, weight loss | 7 days |
| Canine parvovirus | Sudden onset bloody diarrhea, dehydration | 4-8 days |
| Rabies virus | Dumb (paralytic) and furious forms | 14 days to 6 mo |
| NONCORE VACCINES | ||
| Parainfluenza virus | Upper respiratory infection (“kennel cough”) | 3-6 days |
| Bordetella bronchiseptica | Upper respiratory infection (“kennel cough”) | 3-10 days |
| Borrelia burgdorferi | Lyme disease = lameness that often affects more than one limb, lack of appetite, fever | 2-5 mo |
| Canine coronavirus | Diarrhea | 1-4 days |
| Leptospirosis | Renal failure = increased thirst and urination, weight loss, lethargy | — |
| Giardia | Diarrhea (see Chapter 4) | — |
| Lives in Environment | Vaccine Type | Miscellaneous |
| 1 hr | Modified live Recombinant | Highly recommended. Incidence of disease dramatically lower in countries that vaccinate. Can use distemper-measles vaccine for temporary protection in young dogs in affected facilities (rarely done) |
| Days | Modified live Killed | Disease is caused by CAV-1. Excellent cross-protection by immunizing with CAV-2; no risk of introducing disease. Almost always available as part of a combination vaccine with CDV and parvovirus. |
| Years: Easily killed with bleach | Killed | Puppies may have neutralization of vaccine from passive maternal antibodies until as old as 16 wk of age; final vaccination of pups of susceptible breeds when as old as 20 wk probably no longer is necessary, due to increased efficacy of available vaccines. Pups in affected facilities may benefit from vaccination when older than 16 wk. |
| 24 hr | Killed | Required by law. Must be administered by a veterinarian or their designate. Frequency of vaccination varies by municipality. |
| 2 wk | Modified live | Usually combined with canine distemper or with Bordetella. Vaccination often required by boarding facilities. |
| 3 wk | Killed Modified live | Often combined with parainfluenza. Required by boarding facilities. Intranasal form generates immune response more quickly than does injected form of vaccine. Requires booster every 6-12 mo. |
| Cannot survive without a host | Killed Recombinant | Recommended for dogs with a high risk of exposure. Animals that live in New England and in the Mississippi Valley are at increased risk. Side effects of the recombinant vaccine are less severe and occur less frequently than with use of the killed vaccine. |
| 40 hr | Killed Modified live | Puppies less than 6 wk of age may die from infection but often do not. Older animals have mild signs that clear spontaneously. Routine vaccination for coronavirus has not been shown to decrease incidence of infectious viral diarrhea in shelters or kennels and is not recommended. |
| — | Killed | Many serovars of Leptospira are found in the United States. Most vaccines contain the serovars canicola and icterohemorrhagie; if the animal is exposed to another serovar, it is not protected from disease. Anecdotal reports suggest that incidence of allergic reactions to the vaccine in young pups (< 12 wk of age) and small breed dogs is high. |
| — | Killed | Vaccination prevents the animal from shedding oocysts into the environment but does not clear infection from affected animals. Routine use is not recommended. |
* Incubation time is the time from animal exposure to signs of disease.
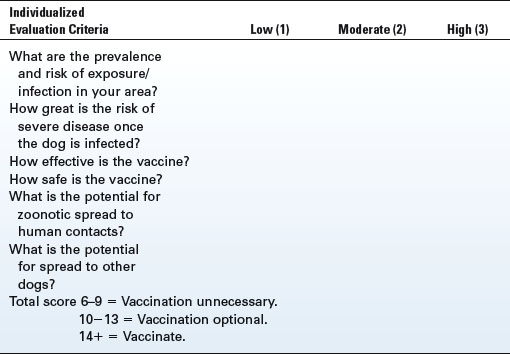
Several tools have been described that can assist veterinarians and owners in deciding the frequency of immunization for their dogs. Issues to consider include the health and lifestyle of the animal, the probability of exposure, the susceptibility to disease if the animal is exposed, the severity of the disease in question, the safety and effectiveness of the vaccine, and public health concerns (can this disease be spread from animals to people?).
The Vaccinometer was developed by Dr. Larry Glickman of Purdue University (Table 5-3). It is intended for use by veterinarians to help them determine necessity of vaccination in a given situation. The company Merial has developed a tool that uses lifestyle considerations to determine which vaccines should be given (Table 5-4). Breeders and pet owners are strongly encouraged to discuss vaccination frequency with their veterinarian.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree