Radiographic technique for the skull86
4.1. RADIOGRAPHIC TECHNIQUE FOR THE SKULL
4.2. BREED AND CONFORMATIONAL VARIATIONS OF THE SKULL AND PHARYNX
CRANIAL CAVITY
Views
Normal appearance
4.3. VARIATIONS IN SHAPE OF THE CRANIAL CAVITY
4.4. VARIATIONS IN SHAPE OF THE FORAMEN MAGNUM
4.5. VARIATIONS IN RADIOPACITY OF THE CRANIUM
4.6. VARIATIONS IN THICKNESS OF THE CALVARIAL BONES; CALVARIAL MASSES
4.7. ULTRASONOGRAPHY OF THE BRAIN
MAXILLA AND PREMAXILLA
Views
4.8. MAXILLARY AND PREMAXILLARY BONY PROLIFERATION OR SCLEROSIS
4.9. MAXILLARY AND PREMAXILLARY BONY DESTRUCTION OR RAREFACTION
4.10. MIXED PROLIFERATIVE–OSTEOLYTIC MAXILLARY AND PREMAXILLARY LESIONS
MANDIBLE
Views
Normal appearance
4.11. MANDIBULAR BONY PROLIFERATION OR SCLEROSIS
4.12. MANDIBULAR BONY DESTRUCTION OR RAREFACTION
4.13. MANDIBULAR FRACTURE
4.14. MIXED PROLIFERATIVE–OSTEOLYTIC MANDIBULAR LESIONS
TEMPOROMANDIBULAR JOINT
Views
Normal appearance
4.15. TEMPOROMANDIBULAR JOINT NOT CLEARLY SEEN
4.16. ABNORMALITIES OF THE TEMPOROMANDIBULAR JOINT
EAR
Views
Normal appearance
Positive contrast canalography
Fistulography
4.17. ABNORMALITIES OF THE EXTERNAL EAR CANAL
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



Head and neck
4.2 Breed and conformational variations of the skull and pharynx87
Soft tissues of the head and neck105
4.36 Thickening of the soft tissues of the head and neck105
4.37 Variations in radiopacity of the soft tissues of the head and neck105
4.38 Contrast studies of the nasolacrimal duct (dacryocystorhinography)106
4.39 Ultrasonography of the eye and orbit106
4.40 Contrast studies of the salivary ducts and glands (sialography)109
4.41 Ultrasonography of the salivary glands109
4.42 Ultrasonography of the thyroid and parathyroid glands110
4.43 Ultrasonography of the carotid artery and jugular vein110
4.44 Ultrasonography of lymph nodes of the head and neck110
4.45 Cervical oesophagus111
4.46 Nasal dermoid sinus cyst111
A basic radiographic examination of the head and neck should include laterolateral and dorsoventral (DV) and/or ventrodorsal (VD) views. The DV is usually easier to position than the VD, as facial landmarks can be seen. Great care should be taken to achieve accurate positioning, and to facilitate this, general anaesthesia is usually required. A high-definition film–screen system or digital algorithm should be used, and a grid is not necessary. Positioning for views (c), (e) and (h) may be achieved using soft ties or a perspex positioning frame.
Additional specialized views are used to highlight specific areas of the head.
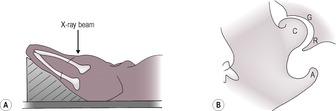
a. Lateral oblique view, with rotation of the skull about its long axis; for a left 30° dorsal–right ventral oblique or a right 30° dorsal–left ventral oblique, the skull is rotated about its long axis towards the DV position, and for a left 30° ventral–right dorsal oblique or a right 30° ventral–left dorsal oblique, it is rotated towards the VD position. Used to separate symmetrical head structures such as the jaws, dental arcades, tympanic bullae and frontal sinuses but requires two identically positioned radiographs, one for each side. For the teeth, the mouth may be open to reduce superimposition.
b. Sagittal oblique (left 20° rostral–right caudal oblique or a right 20° rostral–left caudal oblique), in which the nose is tilted up from a true lateral position, each demonstrating the dependent temporomandibular joint (TMJ) (Fig. 4.8).
c. Rostrocaudal (RCd) closed mouth, to skyline the frontal sinuses or cranium or to demonstrate the nasal cavities end on. The animal lies in dorsal recumbency with the head flexed, and using a vertical X-ray beam, the area of interest being profiled correctly using the light beam diaphragm.
d. Caudorostral (CdR) horizontal beam view for frontal sinuses. The animal is in sternal recumbency with the head raised to profile the frontal sinuses. This view may be used to demonstrate fluid lines within the sinuses.
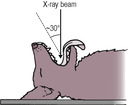
e. Rostro 30° ventral–dorsocaudal oblique with open mouth and vertical head and X-ray beam, to demonstrate the tympanic bullae (also known as RCd open mouth; see Fig. 4.9).
g. Intraoral DV (occlusal) for the nasal cavity, maxilla and premaxilla. Requires non-screen film or a thin, flexible cassette.
h. Open mouth VD (ventro 20° rostral–caudodorsal oblique) with open mouth, horizontal hard palate and X-ray beam angled dorsocaudally for demonstration of the nasal cavity; an alternative to (g) but allowing more caudal structures such as the cribriform plate to be included; especially useful in cats. Placing a sandbag under the neck may help in positioning (Fig. 4.12).
j. Special views for teeth (see p. 01).
k. Lesion-oriented oblique view – to skyline areas of deformity such as swellings.
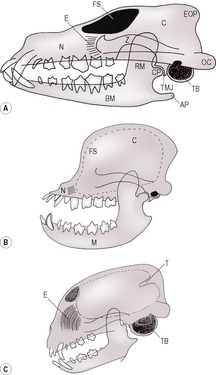
Breeds of dog can be divided into three groups:
1. dolichocephalic breeds, in which the nasal cavity is longer than the cranium (e.g. Irish Setter).
2. mesaticephalic breeds, in which the nasal cavity and cranium are of approximately equal length (e.g. Labrador).
3. brachycephalic, breeds in which the nasal cavity length is greatly reduced (e.g. Bulldog).
There are marked conformational variations in the skull, particularly between different breeds of dog but also to a lesser extent between different breeds of cat (Fig. 4.1). Brachycephalic breeds have a short maxilla, although the mandible may remain relatively long. The nasal cavity is correspondingly reduced in size, and the teeth may be crowded and displaced. The cranium is more domed, and the occipital protuberance and frontal sinuses are less prominent than in the longer-nosed breeds. The fontanelle and suture lines may remain open. On CT or MRI, many of these dogs are seen to have ventriculomegaly, i.e. subclinical hydrocephalus. Brachycephalic breeds of dog also show soft palate thickening, increased submandibular soft tissue mass and caudal displacement of the hyoid apparatus. Skull, facial and cranial indices have been described that express skull (facial or cranial) width as a percentage of length; brachycephalic dogs have higher indices than mesaticephalic and dolichocephalic dogs, especially for the facial area.
In cats, the cranium is relatively large and the tentorium osseum between the cerebral hemispheres and cerebellum is prominent on the lateral view. The tympanic bullae are large and contain a characteristic inner bony shell that divides the bulla into two portions, ventromedial and dorsolateral.
a. Laterolateral.
b. Dorsoventral or ventrodorsal.
c. Lateral oblique.
d. Rostrocaudal.
e. Lesion-oriented oblique.
The normal calvarium has slightly variable opacity, giving a copper-beaten appearance, due to variations in its thickness as it conforms to cerebral sulci and gyri. In small, dome-headed breeds such as the Chihuahua, the fontanelle and suture lines may remain open throughout life.
1. Breed-associated – brachycephalic breeds of dog and cat tend to have a domed calvarium; many have ventriculomegaly (subclinical hydrocephalus).
2. Congenital hydrocephalus (Fig. 4.2) – exaggeration of the domed shape, with thinning of the bones of the calvarium. The calvarial bones may have a more uniform radiopacity than normal, lacking the usual copper-beaten appearance, and the fontanelle and suture lines are likely to remain open.
4. Trauma – usually flattening or concavity of the calvarium seen on a lesion-oriented oblique view; fracture lines may be visible.
5. Thinning and caudal bulging of the occipital bone is seen in Cavalier King Charles Spaniels with caudal occipital malformation (Chiari syndrome), which is usually associated with syringohydromyelia, diagnosed using MRI.
6. Thickening and irregularity of the calvarium is seen in idiopathic calvarial hyperostosis of Bullmastiffs (see 4.6.2).
1. Abnormal dorsal extension (keyhole shape) seen in occipital dysplasias; usually toy and miniature breeds of dog; may be associated with hydrocephalus and/or atlantoaxial malformations. Seen on a well-penetrated RCd view.
1. Decreased radiopacity of the cranium.
b. Localized.
– Superimposed gas shadows in external ear canals.
– Normal suture lines or vascular channels.
– Fracture lines.
– Neoplasia.
– Pneumocephalus – usually ventricular.
2. Increased radiopacity of the cranium.
a. Localized.
– Trauma leading to periosteal new bone formation; subperiosteal haematoma in the nuchal crest area, which then mineralizes.
– Neoplasia – osteoma or multilobular tumour of bone (MLTB – see 4.6.3 and Fig. 4.3; well-defined, dense bony masses); osteochondroma or multiple cartilaginous exostoses (in cats, often involve the skull; rounded, well-mineralized juxtacortical masses); osteosarcoma (often predominantly proliferative in the skull).
– Overlapping fracture fragments.
– Foreign body reaction.
– Calcification of a meningioma or hyperostosis of overlying cranial bone (especially in cats).
– Myelographic contrast in the ventricular system and subarachnoid space – characteristic pattern following brain sulci.
3. Mixed or mottled radiopacity of the cranial bones – usually due to a mixture of bone production or soft tissue mineralization and osteolysis.
a. Neoplasia – primary bone and soft tissue tumours tend to have varying proportions of bone destruction and bone proliferation or soft tissue mineralization. Examples are osteosarcoma, which tends to be predominantly proliferative at this site but with some destruction, and MLTB (osteochondrosarcoma), which is a dense mass with speckled mineralization and little osteolysis of underlying bone, most often involving the temporo-occipital region (see 4.6.3 and Fig. 4.3).
b. Osteomyelitis – especially following trauma, and may be associated with meningitis.
– Bacterial.
– Fungal (e.g. cryptococcosis*) – predominantly osteolytic.
1. Thinning of the bones of the calvarium.
a. Normal variant in small, brachycephalic breeds of dog, possibly due to subclinical hydrocephalus.
b. Hydrocephalus (congenital or arising at a young age) – usually with a domed calvarium, open suture lines and fontanelle and a homogeneous ‘ground glass’ radiopacity. If there are open sutures, it may be possible to examine the brain ultrasonographically (see 4.7). Acquired hydrocephalus is unlikely to produce bony changes.
c. Erosion by an adjacent mass.
2. Increased thickness of the bones of the calvarium.
a. Normal variant in some breeds (e.g. Pit Bull Terrier).
b. Healed fracture.
d. Hyperostosis (thickening and sclerosis) of the calvarium in young Bullmastiffs approximately 6–9 months of age – usually self-limiting and regresses at skeletal maturity; unknown aetiology, although it has some similarities to craniomandibular osteopathy and human infantile cortical hyperostosis. Affects mostly males but also reported in females and there may be a familial component. Femoral periostitis was also described in one dog.
e. Meningioma in cats – may cause localized hyperostosis adjacent to the tumour; often best seen on a RCd view.
f. Acromegaly in cats.
g. Hypervitaminosis A in cats may give rise to occipital new bone (see 5.4.8).
3. Bony masses on the calvarium.
a. Malignant neoplasia, for example osteosarcoma, chondrosarcoma, MLTB (also known as multilobular osteochondrosarcoma, chondroma rodens). Varying degrees of associated osteolysis. MLTB is an uncommon canine tumour that arises almost exclusively on the skull, mainly on the calvarium, maxilla and mandible. It is slow-growing and locally invasive, often recurring after excision. Metastasis may occur. Radiographically, it appears as a dense, mineralized mass with a nodular or stippled pattern and a variable degree of underlying osteolysis (Fig. 4.3).
b. Benign neoplasia (e.g. osteoma) – rare in small animals.
d. Healing or healed trauma (e.g. fracture, subperiosteal haematoma).
e. Severe, localized osteomyelitis.
Ultrasonographic examination of the brain is possible if there is an open fontanelle, and so can often be performed in young dogs and sometimes in adults of brachycephalic breeds. The brain itself appears hypoechoic and loosely granular in texture, while the interior of the cranial cavity is outlined by a well-defined echogenic line. It may be possible to identify the lateral ventricles as small anechoic foci, usually bilaterally symmetrical in size, shape and position. MRI and CT are, however, superior imaging techniques for imaging of intracranial structures.
Blood flow in the basilar artery (located by colour Doppler) can be evaluated via the cisterna magna. Flow in the ventrally located rostral or middle cerebral arteries can also be measured if there is an open fontanelle. Because absolute flows can be influenced by the angle between the incident sound and the artery, it is more usual to measure the resistive index (RI), which is the ratio of the difference between peak systolic and end diastolic velocities (Vs and Vd, respectively) and the peak systolic velocity:
The normal RI in the basilar artery in dogs is 0.56–0.75. RI correlates strongly with intracranial pressure, hence increased RI reflects raised intracranial pressure. Care should be taken in interpreting RI in animals under general anaesthesia or with cardiovascular disease.
1. Increased size of the lateral ventricles.
a. Breed-associated; most brachycephalic breeds of dog have larger lateral ventricles than non-brachycephalic breeds.
b. Hydrocephalus.
– Congenital.
– Acquired due to obstructive lesions such as tumours causing increased production of cerebrospinal fluid or preventing its caudal flow.
2. Increased RI.
a. Hydrocephalus.
b. Intracranial mass lesions.
c. Intracranial bleeding.
d. Brain oedema.
e. Inflammatory brain disease.
f. Raised systolic blood pressure.
a. Laterolateral (right and left sides are superimposed).
b. Lateral oblique.
c. Intraoral DV.
d. Intraoral DV with beam angled laterally for maxillary teeth.
e. Open mouth VD (ventro 10° rostral–dorsocaudal oblique) (Fig. 4.12).
1. Osteomyelitis – usually a mixture of bone proliferation and destruction.
a. Secondary to dental disease.
b. Secondary to chronic dacryocystitis and may be associated with cystic dilation of the nasolacrimal duct; dacryocystorhinography is indicated (see 4.38).
c. Bacterial.
d. Fungal.
3. Healing or healed maxillary or premaxillary fracture.
1. Malignant neoplasia – all types may show some degree of bone proliferation but some are predominantly osteolytic. The osteolysis varies from localized and sharply marginated in appearance to diffuse; teeth in the area may be displaced, eroded or lost. The histological nature of the mass cannot be predicted from the radiographs.
b. Malignant melanoma; commonest oral tumour in dogs.
c. Fibrosarcoma.
d. Primary bone tumours, primarily osteosarcoma.
e. Other oral sarcomas (e.g. leiomyosarcoma).
f. Nasal cavity neoplasia eroding the surrounding bony case.
2. Non-malignant, odontogenic tumours – these do not metastasize but are locally invasive and therefore often radiographically indistinguishable from malignant tumours.
a. Acanthomatous ameloblastoma (acanthomatous epulis, basal cell carcinoma, adamantinoma) – dogs only.
b. Ameloblastoma.
c. Amyloid-producing odontogenic tumour.
d. Complex and compound odontoma – include organized or disorganized dental tissue (see 4.12.2. and Fig. 4.7).
e. Other rare odontogenic tumours.
3. Dentigerous or non-eruption cyst – expansile, radiolucent lesion containing tooth elements.
4. Periodontal disease and dental abscessation – radiolucent halo of osteolysis around the affected tooth root(s) (see 4.30.1 and 4.30.2 and Fig. 4.17).
5. Renal secondary hyperparathyroidism (rubber jaw, osteodystrophia fibrosa) (Fig. 4.5) – osteopenia secondary to chronic renal disease, especially renal dysplasia in young animals. The skull is affected primarily, and bones become osteopenic with a lace-like trabecular pattern and prominence of the nasal turbinates and soft tissue structures such as the soft palate. Bone mineral loss is especially marked around the teeth, with ill-defined haloes of rarefaction giving the impression of floating teeth. Rarely, primary or nutritional secondary hyperparathyroidism in adult animals may cause the same signs.
6. Nasolacrimal duct cysts – discrete radiolucency with a fine, sclerotic margin, communicating with the nasolacrimal duct on dacryocystorhinography (see 4.38).
8. Maxillary bone epithelial cyst – discrete osteolytic lesion, seen mainly in young dogs and not communicating with the nasolacrimal duct.
9. Maxillary giant cell granuloma – discrete osteolytic lesion, seen mainly in young dogs and not communicating with the nasolacrimal duct.
10. Fractures – check involvement of teeth, especially permanent tooth germs in young animals.
1. Periodontal disease and dental abscessation – radiolucent halo of osteolysis around tooth root(s) and surrounding sclerosis.
2. Neoplasia – mixed osteolysis and new bone production; tumours of dental origin also contain highly opaque dental tissue.
a. Laterolateral (mandibles are superimposed over each other).
b. Dorsoventral or ventrodorsal (partly obscured by maxillae).
c. Lateral oblique.
d. Intraoral VD.
e. Intraoral DV with beam angled laterally for mandibular teeth.
The mandibles of brachycephalic breeds are markedly curved when seen on the lateral view, suggesting an attempt at shortening in order for the incisor teeth to approach those of the premaxilla (Fig. 4.1b). In elderly cats, the mandibular symphysis appears irregular on the intraoral view.
1. Craniomandibular osteopathy (Fig. 4.6) – florid periosteal new bone that remodels with time; immature dogs, primarily small breeds such as the West Highland White Terrier, Cairn Terrier and Scottish Terrier but occasionally large breeds; usually involves the mandible and/or the tympanic bullae but also sometimes the calvarium and frontal bones. The new bone is mainly palisading in appearance (see 1.6.1), and osteolysis is absent. Clinical signs often wax and wane, with bouts of pyrexia as well as swelling of the affected mandible(s); difficulty eating if the new bone encroaches on the TMJs.
2. Osteomyelitis – usually a mixture of bone proliferation and destruction.
a. Secondary to dental disease or fracture.
b. Bacterial.
c. Fungal.
3. Neoplasia – more often predominantly osteolytic (see below) but can be proliferative; some are exclusively proliferative (e.g. osteoma). For MLTB, see 4.6.3 and Figure 4.3.
4. Healing or healed mandibular fracture.
5. Canine leucocyte adhesion deficiency – young Irish Setters (see 1.24.9).
6. Acromegaly (cats).
3. Dentigerous or non-eruption cyst; especially affecting PM1, with focal areas of mandibular osteolysis seen unilaterally or bilaterally; Boxers may be predisposed.
4. Periodontal disease and dental abscessation – radiolucent halo of osteolysis around the affected root(s) (see 4.30.1 and Fig. 4.17). In severe cases may lead to pathological mandibular fracture.
6. Mandibular giant cell granuloma – discrete osteolytic lesion seen mainly in young dogs.
1. Trauma.
a. Symphyseal injury – most common in the cat; high rise syndrome (falling from a height) typically results in symphyseal separation and splitting of the hard palate, in conjunction with limb and soft tissue injuries.
b. Fractures of the body of the mandible – check involvement of teeth, especially permanent tooth germs in young animals.
c. Fractures of the ramus (also, depressed factures of the zygomatic arch may impinge on the ramus, causing problems opening the mouth).
d. Fractures involving the TMJ; may cause subsequent TMJ ankylosis, especially in cats.
2. Pathological fracture.
a. Through an area of severe periodontal disease or a dental abscess, especially in toy breeds of dog.
b. Osteolytic tumour, for example squamous cell carcinoma, melanoma, lymphoma (especially cats).
c. Renal secondary hyperparathyroidism.
See 4.10. In cats especially, it is difficult to differentiate mandibular osteomyelitis from neoplasia, as both may produce osteolysis (sometimes with pathological fracture), sclerosis, periosteal new bone and erosion of teeth.
The TMJ is a transversely elongated condylar synovial joint formed between the condylar process of the mandible and the mandibular fossa of the temporal bone. The fossa has a caudoventral extension, the retroarticular process, which prevents caudal luxation of the joint. The TMJ does not lie truly transversely but is angled slightly in a caudolateral to rostromedial direction. There is considerable variation in the precise orientation of the TMJ between breeds and individuals, with the joint lying more obliquely in brachycephalic animals. Accurate radiographic demonstration of the joint can be challenging due to these anatomical variations and to superimposition by other structures.
a. Sagittal oblique (with mouth open and closed, Fig. 4.8). An angle of 10–30° in mesaticephalic and dolichocephalic breeds and an angle of 20–30° in brachycephalic breeds have been found to be optimal. Slight lateral rotation of about 10° may also help to prevent superimposition over the base of the skull.
b. Ventrodorsal or DV.
On the sagittal oblique views, the mandibular condyle should be smoothly rounded, fitting closely into the glenoid (the smooth concavity in the petrous temporal bone), immediately rostral to the tympanic bulla.
2. Technical factors.
a. Underexposure.
b. Underdevelopment.
3. Trauma.
a. Fracture.
b. Luxation or subluxation.
4. Periarticular new bone.
a. Healing or healed fracture.
b. Osteoarthritis.
c. Ankylosis following trauma – especially cats after mandibular trauma; may be bilateral. Pseudoankylosis without radiographic changes can occur due to fibrosis as a result of haemarthrosis.
e. Canine leucocyte adhesion deficiency (young Irish Setters – see 1.23.7).
5. Destruction of articular surfaces.
a. Infection – may extend from infection of the external or middle ear or from a para-aural abscess or wound.
b. Neoplasia – primary bone tumour or invading soft tissue tumour; variable amounts of new bone too.
1. Irregular articular surfaces.
a. Trauma.
– Fracture; may lead to ankylosis secondary to haemarthrosis or callus, especially in cats.
– Luxation or subluxation; usually unilateral, with condyle displaced rostrally and deviation of the mandible to the contralateral side; rarely, fracture of the retroarticular process allows caudal luxation.
b. Osteoarthritis – narrowing of joint space and periarticular osteophytes may also be seen.
c. Infection – may extend from infection of the external or middle ear or from a para-aural abscess or wound.
d. Neoplasia – primary bone tumour or invading soft tissue tumour; variable amounts of new bone too.
2. Temporomandibular joint dysplasia – flattening ± abnormal angulation of the articular surfaces and absence of the retroarticular process are seen in some cases; especially the Basset Hound and Irish Setter. May be clinically silent in some dogs, especially the Cavalier King Charles Spaniel. On an open mouth VD view, the coronoid process of the mandible may be seen to impinge on the zygomatic arch, resulting in open mouth jaw locking. If the condition is unilateral, the impinging coronoid process is on the side contralateral to the TMJ dysplasia. Subluxation of the mandibular condyle may sometimes be seen by comparing open and closed mouth sagittal oblique radiographs.
b. Lateral oblique, skylining the dependent tympanic bulla.
c. Open mouth RCd for tympanic bullae (Fig. 4.9).
d. In the cat, a special view, the rostro 10° ventral–dorsocaudal oblique, has been described for the tympanic bullae (Fig. 4.10) and is technically easier than the RCd open mouth view used in dogs.
The normal external ear canals are seen as bands of gas lucency lateral to the tympanic bullae. The external ear canals and the pinnae may create confusing shadows on lateral and oblique radiographs. The walls of the tympanic bullae are seen as thin and regular bony structures, the cat also having an inner bony septum that divides the bulla incompletely into ventromedial and dorsolateral compartments.
The use of positive contrast medium has been described for assessment of the integrity of the tympanic membrane and for evaluation of stenotic ear canals. A small amount of non-ionic contrast medium such as iohexol is instilled into the ear canal and massaged. Presence of contrast medium in the bulla indicates rupture of the tympanic membrane, although false negative results may arise due to plugging of the ear canal with inflammatory debris.
If a para-aural abscess with discharging tracts is present, fistulography may be used to look for connection with the ear.
1. External ear canal not visible.
a. Overexposure, overdevelopment or severe fogging of the film.
b. Congenital absence of the ear canal (atresia).
c. Occlusion of the canal by wax, debris or purulent material.
d. Traumatic separation of the ear canal, usually between the annular and auricular cartilages; may give rise to otitis media and para-aural abscessation ± discharging sinuses.
e. Previous surgical ablation of the canal.
f. Occlusion of the canal by a soft tissue mass within or outside the canal.
– Neoplasm.
– Inflammatory polyp.
– Para-aural abscess.
2. Narrowing of the external ear canal.
b. Compression of the canal by a para-aural mass or swelling.