34 GLUCOSE
1 Why does delayed processing or analysis of a blood sample result in a lower glucose concentration?
2 If blood samples cannot be processed within an hour of collection, how can the glucose concentration in the sample be maintained?
3 What are the disadvantages of using sodium fluoride tubes?
Besides inhibiting enolase in the glycolytic pathway, fluoride inhibits other enzymes, including the glucose oxidase of some glucose assays. Thus the NaF sample may not be an acceptable sample for determining glucose concentration.
4 Why does a blood glucose concentration not equal a plasma/serum glucose concentration?
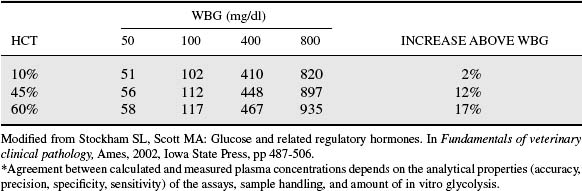
The differences between blood glucose and plasma or serum glucose concentration typically will be slight, but differences can be caused by erythrocytosis, sample processing errors, or differences in assay methods. Erythrocytosis will increase the difference because the glucose concentration in erythrocytes is lower than in plasma/serum. The concentration of glucose in the plasma H2O and erythrocyte H2O is the same, but there is less H2O in erythrocytes (most volume is occupied by hemoglobin) and thus less glucose in erythrocytes per unit volume. The greater the erythrocyte concentration in blood, the greater will be the difference between blood glucose concentration and plasma glucose concentration (blood glucose concentration will be lower). Plasma concentrations were calculated in Table 34-1 using the following conversion formula:
Table 34-1 Calculated Plasma Glucose Concentrations in Blood Samples with Given Whole-Blood Glucose Concentrations (WBG) and Hematocrit (Hct) Values*
8 In health, how similar are plasma/serum glucose concentrations and cerebrospinal fluid glucose concentrations?
10 What are the three major changes or alterations in physiologic processes that produce a hyperglycemia?
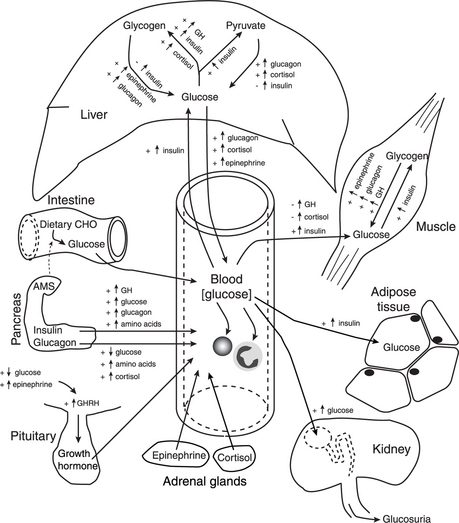
Increased glucose intake can result from ingestion of carbohydrate meal or the infusion of a glucose-containing fluid (e.g., 5% dextrose). Strictly speaking, increased glucose production is limited to increased gluconeogenesis within hepatocytes. However, hepatic glycogenolysis can also result in the release of glucose into blood. Decreased glucose uptake by peripheral tissues can result in a mild hyperglycemia by itself, but increased glucose uptake or increased glucose production can enhance the severity of the hyperglycemia. Figure 34-1 illustrates how these processes are influenced by activities of hormones and other factors.