Chapter 109 Fractures of the Femur
Surgery of the femur usually is performed to repair fractures. Biopsy of tumors or cysts and obtaining samples for bone cultures are less common reasons for femoral surgery. The femur is the bone most commonly associated with traumatic fractures in the dog. Surgical repair of femoral injuries may be divided into surgery of the proximal, diaphyseal, and distal femur.
PROXIMAL FEMUR
Anatomy
• The proximal femur includes the femoral head, the femoral neck, the trochanters, and their attachments to the femoral shaft.
• The ligament of the head of the femur runs from the fovea capitis of the femoral head to the acetabular fossa.
• The articular surface and epiphysis of the femoral head are separated from the femoral neck by the capital physis.
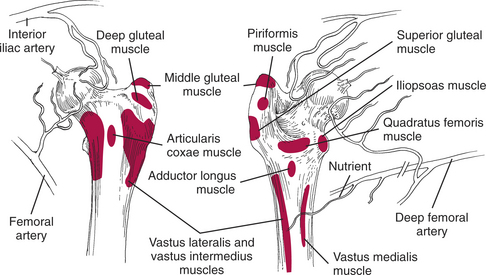
• The primary blood supply to the epiphysis of the femoral head is through vessels running longitudinally in folds of the joint capsule (Fig. 109-1).
• The greater trochanter is the point of attachment for the deep and middle gluteal muscles and the piriformis muscle (see Fig. 109-1).
• The trochanteric fossa is the site of insertion of the internal obturator, external obturator, and the gemelli muscles.
• The lesser trochanter on the medial aspect of the proximal femur is the site of insertion of the iliopsoas muscle.
• The third trochanter (lateral and distal to the greater trochanter) is the site of insertion of the superficial gluteal muscle and the origin of the quadratus femoris muscle and part of the vastus lateralis muscle.
• The proximal femur is the site of origin of the vastus lateralis, vastus medialis, vastus intermedius, quadratus femoris, and adductor longus muscles and of the proximal part of the adductor magnus and adductor brevis muscles.
• The deep muscles of the femur are covered by the tensor fasciae latae and biceps femoris muscle confluence.
• The sciatic nerve runs caudal to the hip on top of the gemelli, internal obturator, and quadratus femoris muscles. It is covered by the biceps femoris and the superficial gluteal muscles.
• The femoral artery, nerve, and vein are very superficial in the femoral triangle on the medial aspect of the proximal to midfemur.
• The nutrient artery for the femur enters caudally just distal to the greater trochanter as a branch of the medial circumflex femoral artery.
PROXIMAL FEMORAL FRACTURES
Preoperative Considerations
• Give intraoperative broad-spectrum antibiotics intravenously (at induction of anesthesia; repeat if necessary) if the surgery will take longer than 2 hours.
Surgical Procedure
Equipment
• Orthopedic instruments, as required (e.g., for fracture fixation, ostectomy, subtrochanteric derotational osteotomy), including:
Common (Craniolateral) Approach
Technique
2. Make a linear or slightly curved skin incision centered over the cranial aspect of the greater trochanter, starting near the dorsal midline and ending on the cranial aspect of the proximal one-third of the femur.
3. Incise the subcutaneous tissue to expose the tensor fasciae latae muscle. Incise two layers of the fasciae latae along the cranial border of the biceps femoris muscle to expose the underlying vastus lateralis muscle.
4. Extend the fascial incision proximally through the gluteal fascia along the cranial border of the superficial gluteal muscle.
5. Bluntly dissect the loose connective tissue between the vastus lateralis muscle and the gluteal muscles to allow insertion of self-retaining retractors to expose the joint capsule.
6. Using a scalpel, incise through the joint capsule from the acetabulum, longitudinally along the femoral neck, to the proximal femur at the insertion of the vastus lateralis muscle.
Femoral Neck/Capital Physeal Fracture Repair
Technique
2. Retrograde a K-wire of appropriate size through the femoral neck fracture surface to exit the lateral surface of the proximal femur.
3. If a compression (lag) screw is used, drill a gliding hole through the center of the femoral neck to exit the lateral surface of the proximal femur.
4. If multiple K-wires are used, preplace them all through the femoral neck, using the same technique as described in Step 2 above.
5. Withdraw the wires from the lateral surface until the pinpoints are flush with the fracture surface.
8. Advance one K-wire into the femoral head without penetrating the articular surface (Fig. 109-2, left).
9. If a compression screw is used, insert a drill sleeve into the gliding hole and drill into the femoral head. The articular cartilage should not be penetrated. Measure and tap the hole and place a screw of suitable length. Compress the fracture without penetrating the articular surface with the screw (Fig. 109-2, right).
10. If K-wires are used, drive these individually into the head without penetrating the articular cartilage.
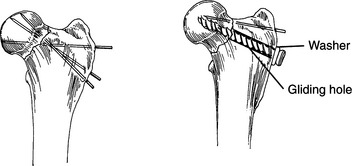
Figure 109-2 Fixation of femoral neck fractures. Left, Multiple Kirschner wires; right, compression screw and Kirschner wire.
Trochanteric Osteotomy
This technique is used for exposure of the hip joint as part of open reduction of coxofemoral luxation or as an approach to acetabular fractures (see Chapters 107, 108).
Technique
3. Incise the proximal origin of the vastus lateralis muscle and elevate the muscle to expose the trochanteric osteotomy (or fracture) site, or the femoral neck fracture site.
5. If a trochanteric osteotomy is planned, pass a curved Kelly forceps under the deep gluteal insertion.
6. Using the curved Kelly forceps as a guide, direct the osteotome (or pull the Gigli wire through), and osteotomize the trochanter off the proximal femur, leaving the medial and deep gluteal muscles attached to the osteotomized bone.
Trochanter Fracture Osteotomy Repair
Technique
1. Drill a hole transversely through the femur at least 1 cm distal to the osteotomy (fracture) site.
3. Clamp the proximal fragment in its anatomic position with a small-fragment bone reduction forceps.
4. Drive two appropriate-size K-wires from the proximal end of the trochanter, across the osteotomy (fracture) line, and into the femur until they are seated in compact bone.
5. Pass one free end of the orthopedic wire proximal to the pins and under the gluteal tendons (Fig. 109-3).