Chapter 105 Fractures and Growth Deformities of the Radius and Ulna, Luxation of the Elbow
FRACTURES OF THE RADIUS AND ULNA
Anatomy
Radius
• The radius is the main weight-bearing bone of the antebrachium and is shorter than the ulna. The radius is composed of the head, neck, body, and distal extremity. The medullary canal is elliptical in shape owing to flattening of the radius.
• The radius is attached to the ulna by an interosseous ligament that helps to maintain their spatial relationship following fracture. The short radial collateral ligament runs from the styloid process of the radius to the radial carpal bone and provides medial support to the antebrachiocarpal joint.
Ulna
• The ulna is the longest bone in the body and is composed of the olecranon, trochlear notch, anconeus, body, and the distal extremity called the styloid process.
• The ulnar body tapers as it crosses caudal to the radius to articulate with the palmarolateral aspect of the carpus. The medullary canal of the ulna functionally ends about one-third from the distal end.
Vascular Supply
• The radial and interosseous arteries provide the main arterial supply to the antebrachium and are subject to injury from trauma or surgery.
• The radial artery travels along the palmaromedial aspect of the radius just under the flexor carpi radialis muscle.
General Preoperative Considerations
• Evaluate the thorax for pulmonary contusions, pneumothorax, and diaphragmatic hernia with thoracic radiography. Evaluate for traumatic myocarditis with electrocardiography.
• Examine the animal for concurrent injuries; inspect other limbs for fractures or other significant injury.
• Evaluate nerve function of the affected limb by testing reaction to a painful stimulus to the skin of the various dermatomes and by withdrawal of the limb.
• Initially place the limb in a Robert Jones bandage or splint to prevent further soft tissue damage and to prevent the fracture from becoming an open fracture.
General Objectives of Surgical Procedures
• Align and stabilize the fracture(s) to permit uncomplicated healing with normal joint and limb function.
General Postoperative Care and Complications for Radial and Ulnar Fractures
• Place the limb in a soft padded bandage for 3 to 10 days to reduce postoperative swelling. Provide more rigid external support if needed.
Complications
• Delayed and nonunion healing (see Chapter 122), osteomyelitis (see Chapter 121), and implant failure may occur.
• Joint fractures are prone to subsequent degenerative joint disease and callus that interferes with joint mobility if anatomic alignment and rigid stability have not been achieved.
• Joint stiffness can develop with articular fractures. Rigid stability of the fracture allows early, controlled use of the joint.
Olecranon Fractures
Technique
1. Place the patient in lateral recumbency, with the affected leg up, and prepare the limb for aseptic surgery.
3. Reflect the skin and subcutaneous tissue to expose the olecranon and proximal shaft of the ulna. Subperiosteally elevate the extensor and flexor carpi ulnaris muscles from the proximal shaft of the ulna.
5. Drive two K-wires or small intramedullary pins parallel from the tip of the olecranon across the fracture line and into the distal segment of the ulna (in very small animals, drive only one K-wire).
6. Drill a hole (perpendicular to the ulnar long axis) in the distal ulnar segment 1.5 to 2 times the distance from the olecranon to the fracture line.
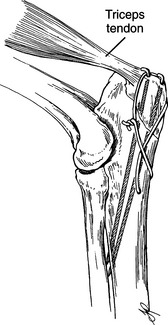
9. Bend the pins over and cut them off short. Cut the wires leaving two to four twists and bend the wire tips over (Fig. 105-1).
Trochlear Notch Fractures
Technique
Small and Medium-Sized Dogs; Cats; No Fracture Comminution Present
1. Repair the fracture with a tension band wiring technique, as described previously under Olecranon Fractures.
Large Dogs; Fractures with Comminution
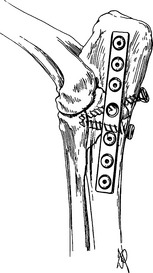
3. Contour a bone plate to the caudal or caudolateral side of the ulna and secure it to the ulna with bone screws (Fig. 105-2).
4. If comminution is not present, apply the plate with a compression technique. If comminution is present, apply the plate in a neutralization manner (e.g., no compression).
Radial Head Fractures
Technique
1. Place the patient in lateral recumbency, with the affected limb up, and prepare the limb for aseptic surgery.
2. Incise the skin, beginning at the proximal end of the lateral epicondyle of the humerus and continuing distally over the radial head to the proximal one-fourth of the radius.
3. Incise the subcutaneous tissue and the antebrachial fascia along the same line to expose the extensor muscles of the antebrachium.
4. Dissect between the ulnaris lateralis muscle and the lateral digital extensor. Cut the ulnaris lateralis tendon, leaving sufficient tendon for suturing. If necessary, incise the anconeus muscle from the lateral epicondyle of the humerus.
5. Reflect the lateral digital extensor muscle cranially with a Hohmann retractor to expose the fracture.
Radial Neck and Proximal Physeal Fractures
Objectives
• Stabilize the fracture in immature animals without fracture compression to help prevent premature closure of the growth plate.
Technique
2. Stabilize the fracture with two K-wires placed in cross-pin fashion from the lateral side. Start one pin just below the articular surface of the radius and drive it distomedially. Start the second pin distal to the fracture and drive it proximomedially.
Monteggia Fractures
Technique
1. Expose the ulnar fracture, as described under Olecranon Fractures and Trochlear Notch Fractures. Expose the ulna as far distally as needed.
2. Expose the radial head, as described under Radial Head Fractures, if the luxation cannot be reduced closed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree