11 Foodborne Illness
The Centers for Disease Control and Prevention (CDC) estimates that each year in the United Sates 76 million persons experience foodborne illness, leading to 300,000 hospitalizations and 5000 deaths. Although most of these cases are attributable to infectious etiologies, exposure to foodborne toxins occurs as well.1 Companion animals are also believed to commonly experience foodborne illness, with signs including acute gastritis or diarrhea, although the actual incidence of animal foodborne illness is not known.
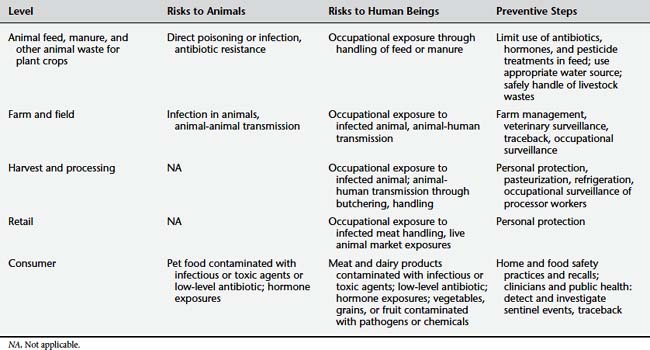
In the United States the Foodborne Diseases Active Surveillance Network of the CDC (FoodNet) performs active surveillance for nine pathogens in selected states (Campylobacter, Cryptosporidium, Cyclospora, Listeria, Salmonella, Shiga toxin–producing Escherichia coli [STEC] O157, Shigella, Vibrio, and Yersinia). Clinicians can access recent reports at http://www.cdc.gov/FoodNet/reports.htm. Despite ongoing prevention efforts on the part of both public health and agricultural health authorities, the rates of Campylobacter, Listeria, Salmonella, Shigella, STEC O157, Vibrio, and Yersinia infections do not appear to have declined in recent years, whereas the rate of cryptosporidiosis has increased. The rate of Salmonella infection was the furthest from public health goals. It is clear that controlling or eliminating foodborne illness will require comprehensive efforts from farm to fork.2 The production of safe, healthy food for the expanding world population has increased the complexity and globalization of the process. There are multiple potential interactions between human and animal health at a number of steps of the food chain (Table 11-1).
Dog and cat food sales were close to $17 billion in the United States in 2008 (Figure 11-1).3 Although many human health care providers may be unaware of the magnitude of the pet food industry, the human health relevance of foodborne illness in companion animals is becoming more evident. Human outbreaks of salmonellosis have been linked to contact with contaminated pet food. Similarly, the outbreak of melamine contamination in human infant formula in China was presaged by an outbreak of disease in cats and dogs traced to a similar melamine contamination of pet food imported from the same country.
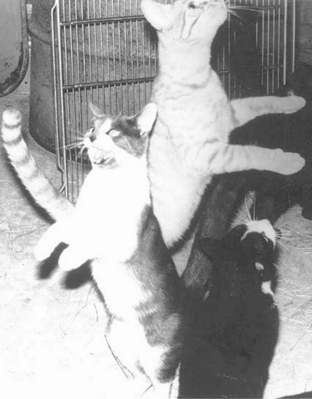
Figure 11-1 Bipedal posture used to request food.
(From Beaver BV: Feline behavior, ed 2, St Louis, 2003, Saunders Elsevier.)
Key Points for Clinicians and Public Health Professionals
Public Health Professionals
Human Health Clinicians
RISKS ALONG THE FOOD CHAIN
Foodborne risks and food safety can be thought of conceptually in terms of a chain of production from animal feed or plant fertilizer to consumer.4,5 At each stage in the chain there are certain risks for both human beings and other animals. At each stage are also opportunities for prevention and control. The Center for Veterinary Medicine of the Food and Drug Administration (FDA) has recommended applying hazard analysis and critical control point (HACCP) principles to the food manufacturing processes to detect and reduce risks.6
Animal Feed and Plant Fertilizer
The first stage of food production involves supplying safe feed for food animals and safe fertilizer for plant crops. The two concepts are interrelated. Animal feed may include both plant and animal products, and plant fertilizer may contain livestock manure and other animal wastes.7 At this stage of the production chain, the health risks are primarily to the food animals, with some risk also to agricultural workers directly handling animal feed and fertilizer. Risks to animals include both toxic and infectious agents. Examples of toxic exposures have included dioxin contamination in pigs8 and poultry; exposure of cattle to the fire retardant PBB (polybrominated biphenyl) through inadvertent contamination of feed; and heavy metal poisoning from cadmium, lead, or mercury contamination of fertilizers applied to crops and pastures.9 Infectious agents threatening the human and animal food supply include bovine spongiform encephalopathy, which appeared in cattle and other animals after being fed meat and bone meal prepared from animals infected with transmissible spongiform encephalopathy (TSE) (see Chapter 9). This risk has been greatly reduced through animal feeding bans. Less clear cut are the risks from the use of antibiotics and hormones in animal feed. Such additives may be used to reduce infection and increase meat or dairy product production (growth promoters).10 There is evidence that these practices can increase the development of antibiotic-resistant pathogens.11 However, most animals treated with such agents show no ill effects and may have increased meat and dairy product output.
Not all animals who have ingested either toxicants or infectious agents show evidence of disease and therefore may pass the risks along the food production chain. A pathogen that has proved difficult to control is Salmonella, many strains of which are adapted to a wide number of animal hosts (see Chapter 9). There is evidence that Salmonella may enter the food supply chain through rendered animal protein used as animal feed.6
Occupational exposure to animal feed and manure fertilizers can result in disease in agricultural workers and persons engaged in small-scale (backyard) food production. Manure used as fertilizer on fields may come from animals who shed pathogens in their feces. Such contaminated feces can then be a risk to workers. For example, contact with infected chicken manure for use in a backyard garden has been linked to a fatal human case of avian influenza.12 Commercial farm workers who have direct contact with infected human or animal wastes used as fertilizer on crops may also be at risk of infection.13 Another hazard of animal feed to workers is allergic and other reactions to grain, which can include “farmer’s lung,” grain mite allergy, and endotoxin exposure (see Chapters 7 and 12). Stored silage can be a source of toxic nitrogen dioxide. This gas forms nitric acid when in contact with the respiratory mucosa and creates acute lung damage, known as silo filler’s disease. This is also a risk for livestock housed near silage; outbreaks of respiratory disease and death in cattle from silo gases have been reported (Figure 11-2), potentially providing warning to human beings of the toxic risk (see Chapter 12).14
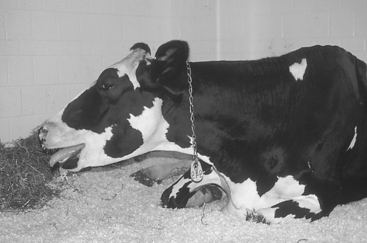
Figure 11-2 Open-mouth breathing in a 5-year-old cow.
(From Divers TJ, Peek SF: Rebhun’s diseases of dairy cattle, ed 2, St Louis, 2008, Saunders Elsevier.)
Farm and Field
In the farm environment, animal-animal, animal-human, and human-animal transmission of infectious agents can occur. In addition to the feed and manure exposures listed, environmental exposures (e.g., water, mosquitoes, and other vectors) and contact with wildlife can introduce pathogens into the food chain if meat is consumed raw or undercooked or if dairy products are unpasteurized. For example, a recent multistate outbreak of salmonellosis in Serrano peppers was traced to contaminated irrigation water in Mexico.15 Rift Valley fever is an example of a vector-borne disease in which infected cattle can then pose an occupational risk to abattoir (slaughterhouse) workers.
Harvest and Processing
Although most processing of animal meat in industrialized countries occurs in specialized facilities with infection control policies and adequate refrigeration, food animals in other countries are slaughtered in backyards or households, farmyards, or open air markets. In these settings biosecurity is low, meat inspection and refrigeration are often not available, and the potential for infection consequently is greater. In addition, hunting for subsistence bushmeat consumption as well as hunting of deer, waterfowl, and other game often involves both slaughter and dressing of the wild animal carcass in a field or other improvised location. Such activities, even in developed countries, may take place without availability of running water or the use of gloves or other types of personal protection. Transmission of simian viruses has been documented in bushmeat hunters,16 and toxoplasmosis, tularemia, and brucellosis have been reported in U.S. hunters who field-dressed their carcasses without personal protection. In these informal settings there is generally no process of organized inspection or medical surveillance of at-risk individuals. Recently there has been a call for improved surveillance of bushmeat hunters17 to detect emerging pathogens and other foodborne diseases that could trigger disease outbreaks in human beings. Occupational medicine surveillance of farmers and workers in processing facilities and marketing retail chains can help detect sentinel health events in human beings (e.g., a Q fever or brucellosis outbreak),18 indicating the presence of the disease in the livestock as well and a likely problem with food safety (see Chapter 12).
To reduce the possibility of disease transmission, dairies generally use pasteurization methods on waste milk fed to calves. Although milk pasteurization for human consumption occurs at the farm level in farms that produce milk and milk products, most U.S. dairies ship milk for human consumption to processing plants, where it is pasteurized and then shipped to distributors.19 Pasteurization practices may vary between farms and regions. Although there is a consumer market for unpasteurized dairy products, which are considered by some to be more “natural,” such products have resulted in a number of foodborne illness outbreaks.20,21
Retail
In the retail sector, handling of meat carries a risk of pathogen exposure similar to that faced by workers in abattoirs, although exposures tend to be lower and reported disease cases are fewer. If vegetables (e.g., peppers contaminated with Salmonella and spinach contaminated with E. coli)22 and fruit (e.g., raspberries with Cryptosporidium)23 have been contaminated with pathogens from animal manure, there is some risk of retail workers becoming sickened by handling such produce.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree