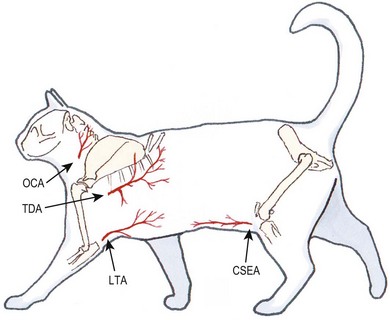
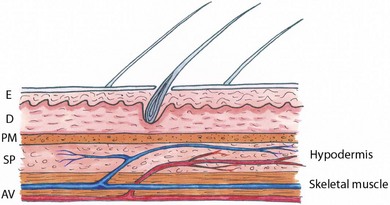
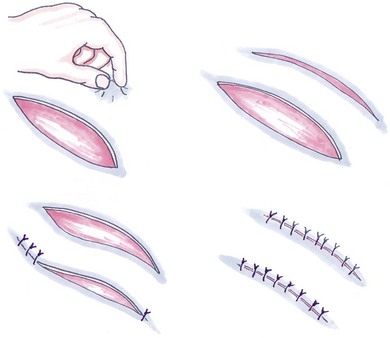
Chapter 19 Skin is composed of two layers, an outer epidermis consisting of stratified squamous epithelium and an inner dermis of dense connective tissue. The skin is loosely attached to the hypodermis composed of loose connective tissue, which in turn connects to underlying muscles.1 When considering using skin for flaps or grafts it is essential to have an understanding of the blood supply. Direct cutaneous arteries travel through intermuscular fascial planes and then run parallel with the overlying skin before connecting to the cutaneous circulation. Direct cutaneous arteries supply angiosomes composed of cutaneous musculature, subcutaneous tissue and skin. The cutaneous vascular system divides further into three interconnecting levels:1 Figure 19-1 Cutaneous vascular supply. Cross section of the skin and the vascular supply. Direct cutaneous artery and vein supplying an angiosome. AV, direct cutaneous artery and vein; D, dermis; E, epidermis; PM, panniculus muscle; SP, subdermal plexus. The subdermal plexus is the major route of arterial supply to the skin. Random flaps are dependent for their vascular support on the terminal branches of the cutaneous circulation and may be developed anywhere in the skin. Although the vascular integrity of random flaps is somewhat less consistent than axial pattern flaps, they remain a very reliable method of reconstruction. It may be beneficial to align the base of random flaps when possible in the direction of any known direct cutaneous vessels to take advantage of this additional vascular support. Although it is sensible to avoid narrow or excessively long flaps, there is no viability limit to the length of random flaps and predicted base width/flap length ratios are not relevant to flaps in the cat.2 Random flaps may be classified in a number of ways (Box 19-1). Single pedicle advancement flaps (Fig. 19-2) are probably the most commonly used local flap employed in veterinary medicine because of their simplicity and the lack of a significant secondary defect requiring closure. Advancement (or sliding) flaps are rectangular in shape and are created parallel to lines of tension with an attachment at the base opposite the edge covering the wound. Paired advancement flaps resulting in an H-pattern of closure can also be employed although they are more complex. They may have better viability than one large flap, otherwise there is little significant advantage (Fig. 19-3). The single relaxing or release incision is a bipedicle advancement flap by design (Fig. 19-4). Figure 19-2 Single pedicle advancement flap. Elevation of a single pedicle flap to reconstruct the cutaneous surface of the upper lip after resection of a large skin tumor. Figure 19-3 Paired single advancement flaps resulting in an H-pattern to close a large rectangular defect on the thorax of a cat. Figure 19-4 Bipedicle advancement flap. The releasing incision creates a flap with vascular supply on both ends of the flap. The resulting defect is left to heal by second intention. Rotation flaps are created by releasing the skin along an arc-shaped incision before moving it along the same axis. They are of limited use in feline reconstruction since relatively large areas of skin need to be raised to achieve wound coverage. The transposition flap is a rectangular pedicle graft, which instead of being moved along its long axis is rotated up to 90 degrees of the wound axis (Fig. 19-5). This is the most common type of rotating flap and is by far the most useful technique to close a variety of small sized problematic wounds. A modification of this flap is the front or hind limb fold flap. Figure 19-5 (A) 90 degrees rotating flap. Two parallel skin incisions are made at an equal distance from the nipples. The length of the flap depends on the length of the defect that needs to be covered. (B) A 90 degree transposition flap. These flaps are used to reconstruct large rectangular defects involving adjacent sites. Direct distant flaps are raised at a location remote from the skin defect and ultimately transferred to the recipient bed by approximating the wound with the donor site. This technique is used almost exclusively for reconstruction of wounds involving the middle or lower extremities and provides durable full thickness skin coverage without the need for skin grafts.3 Flaps are normally raised on the flank and the affected limb brought alongside to allow the flap to be sutured to the recipient bed. Flaps may be single pedicle (hinge; Fig. 19-6) or bipedicle (pouch; Fig. 19-7) grafts. The limb must then be secured against the flank over a ten to 14 day period while the flap attaches to the wound. The pedicle(s) are divided, often in two stages, to complete the transfer.4 Cats are generally well suited to this technique and tolerate the period of limb immobilization better than dogs because of their size, flexible limbs, and the availability of ample loose elastic skin. Distant flaps are multi-staged procedures and consequently are time consuming and expensive. The transplanted skin assumes the same hair growth as its donor site despite its new location. Some patients will not tolerate their limb being immobilized against their flank and this is particularly evident if the limb is positioned in an elevated position. Occasionally, moist dermatitis caused by skin-to-skin contact and moisture accumulation is encountered; transient muscle atrophy of the limb may be noticed in some cases. Figure 19-6 Single pedicle direct distant flap (hinge). These flaps are used to cover defects on the lower forelimb and hindlimb. The flap can be dorsally or ventrally employed depending on the location of the skin defect. An axial pattern flap is a pedicle graft based primarily or solely on the vascular supply of a direct cutaneous artery and vein.5 The vessels, of which terminal branches supply blood to the subdermal plexus, extend the length of the flap. Therefore axial pattern flaps have better perfusion compared to subdermal plexus flaps. Large axial pattern flaps can be safely elevated and transferred in a single-stage procedure for closure of major cutaneous defects. These flaps have excellent survival rates and they can be used to reconstruct wounds associated with less optimal conditions such as contamination, uneven surfaces, exposed bone, tendon, and cartilage. Axial or island pattern flaps are classified according to the vascular territory supplied by the direct cutaneous artery (angiosome). These vessels and territories including the thoracodorsal artery, lateral thoracic artery, omocervical artery, caudal superficial epigastric artery have been researched and mapped for clinical use as axial pattern flaps in the cat. Although the location and relative size of each angiosome are similar for both dogs and cats, the extreme elasticity of feline skin and the relative increase in body size to limb length often facilitates more distal coverage of limb wounds in cats.6 Axial pattern flaps sometimes require extensive dissection of the donor site for flap elevation; because of their relatively large size, axial pattern donor sites may require undermining and walking sutures to appose the defect created by the raised flap. The cosmetic appearance of the recipient bed differs from the donor site with regard to hair direction, color, length, glandular tissues, and amount of subcutaneous tissues. Free grafts are areas of skin that are completely detached from the donor site and hence lose their original vascular supply before being transferred to resurface a recipient site. In feline surgery the use of free skin grafts is confined almost exclusively to reconstruction of large skin defects of the extremities where few alternate options are available.7 Secondary healing of limb wounds can lead to unsightly scar tissue development and may also lead to impaired limb function if formed in the vicinity of joints. The use of random flaps is often restricted by the limited availability of adjacent skin. Direct flaps offer an alternative solution although the temperament of some cats may not always be conducive to this option. Free grafts lack vascular support in the period after transfer and must survive for at least the following 48 hours by absorbing protein-containing fluid from the recipient bed by capillary action, a process known as plasmatic imbibition. During this period the graft becomes attached to the underlying tissue by the development of an interposed fibrin seal that acts as a biological ‘glue’ and provides a scaffold across which capillaries from the recipient bed begin to anastomose with those of the exposed graft plexus to re-establish circulation (inosculation). New capillaries later grow into the graft and the vascular channels remodel (revascularization). Free skin grafts therefore require a vascularized recipient bed and preparation of the recipient bed is a major determinant of successful skin grafting. Fresh active pink granulation tissue is the ideal recipient bed and provides excellent vascular support and the growth factors necessary for these processes to occur. Granulation tissue is not, however, essential for graft survival and any well-vascularized tissue is theoretically capable of accepting and supporting a skin graft. Grafts can therefore be applied over surgically clean and fresh surgical wounds since periosteum, peritenon, and muscle normally have sufficient vascular supply to support skin grafts (Fig. 19-9). Figure 19-9 Free skin graft. A meshed graft was applied over a fresh surgical wound to cover a larger defect after a tumor had been resected. (Courtesy of Georgio Romanelli.)
Flaps and grafts
Surgical anatomy
Cutaneous vascular supply (Fig. 19-1)
Skin flaps
Random pattern or subdermal plexus flaps
Advancement flaps


Rotating/transposition flaps


Distant flaps

Axial pattern flaps (Fig. 19-8)
Free skin grafts

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree