CHAPTER 10 Emergency and Critical Care Issues
Initial Examination and Catheterization
Essentials to evaluate in all neonates are the presence or absence of a strong suckle reflex and whether they are nursing and sleeping. Constant crying occurs if they are prevented from nursing or do not ingest enough milk. Generally, pups and kittens sleep after nursing if a sufficient amount was ingested. Nutrition is crucial to neonatal health and should be addressed early (see Chapter 8).
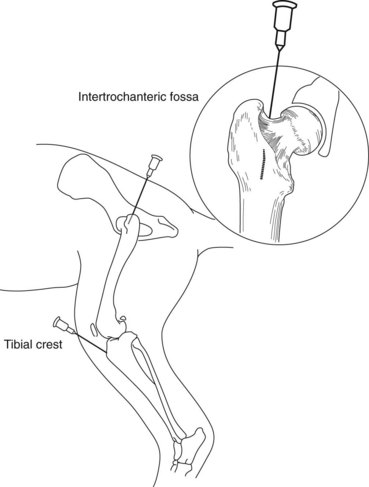
When venous access is required, the intravenous (IV) route is preferred and should be attempted first. Neonates often require very small gauge catheters (i.e., 24 g), which can burr easily when being driven through the skin. A small skin puncture with a 20 g needle (while the skin is kept elevated) can be made and then the catheter can be fed through the skin hole, which can prevent burring. If attempts at IV catheter placement fail, an intraosseous (IO) catheter should be placed. An IO catheter can be inserted in the proximal femur or humerus using an 18- to 22-g spinal needle or an 18- to 25-g hypodermic needle. An IO catheter can be used for fluid and blood administration. The area must be prepared in a sterile manner, and the needle is inserted into the bone parallel to the long axis of the bone (Figure 10-1). The IO catheter is gently aspirated to assure patency and then secured with a sterile bandage. Neonates, who have a large portion of “red” marrow compared with adults who have more “yellow” marrow consisting of fat, are ideal candidates for IO catheters. IV access must be established as soon as possible, ideally within 2 hours, and the IO catheter should be removed to minimize IO infection. IO catheter complications correlate with duration of use in humans.
Fluid Requirements
Fluid requirements are much higher in neonates than adults because of a higher percentage of total body water, a greater surface area to body weight ratio, a higher metabolic rate, a decreased renal concentrating ability, and decreased body fat. Although dehydration is common, overhydration is also a serious concern because the kidneys cannot dilute urine to rid the body of excess water. The best way to monitor for underhydration or overhydration is to have an accurate pediatric gram scale and weigh the patient frequently (ideally 3 to 4 times per day) (Figure 10-2). If possible, baseline thoracic radiographs are helpful. It can be difficult to diagnose fluid overload because the neonatal heart takes up so much of the thoracic cavity and normal neonate lungs have more interstitial fluid than adults. Baseline radiographs can be very helpful in serially monitoring for fluid overload. Other ways to monitor fluid therapy include checking hematocrit (HCT) and total solids. The HCT decreases in normal neonates from days 1 to 28, and total solids are lower than adults.
Laboratory Values (See Chapter 30)
Young puppies and kittens have a lower HCT than adults (Boxes 10-1 and 10-2). The HCT decreases from 47.5% at birth to 29.9% by day 28 in puppies. This decrease is normal and is thought to be the result of the change from a relatively hypoxic environment to an oxygen-rich environment. The HCT will start to increase by the end of the first month of life in healthy neonates. Kittens also have a HCT nadir at 4 to 6 weeks of 27%. Knowledge of this normal decrease in HCT is essential during treatment of any neonate, and during this time period, a rise in the HCT is usually indicative of significant dehydration.
BOX 10-1 Complete blood count: pediatric canine
From Silverstein DC, Hopper K (eds): Small animal critical care medicine, St Louis, 2008, Saunders/Elsevier.
BOX 10-2 Complete blood count: pediatric feline
From Silverstein DC, Hopper K (eds): Small animal critical care medicine, St Louis, 2008, Saunders/Elsevier.
Knowledge of the slight increases in bilirubin (0.5 mg/dl; normal adult range 0 to 0.4) and dramatic increases in liver enzymes at birth in puppies is essential when creating a differential diagnoses list (Boxes 10-3 and 10-4). In puppies, serum alkaline phosphatase (ALP; 3845 IU/L, normal adult range 4 to 107) and gamma-glutamyl transferase (GGT; 1111 IU/L, normal adult range 0 to 7) are over 20 times greater than adult values. In kittens, the ALP (123 IU/L, normal adult range 9 to 42) is 3 times that seen in adults. Serum blood urea nitrogen (BUN), creatinine, albumin, cholesterol, and total protein are lower in neonates than adults. Lower creatinine is thought to be due to decreased muscle mass, and lower BUN and cholesterol are due to immature liver function. Knowledge of these values is crucial to prevent a misdiagnosis of liver disease in the neonate (elevated liver enzymes and low levels of BUN, cholesterol, and albumin can all mimic liver dysfunction).
BOX 10-3 Biochemistry profiles: pediatric canine*
From Silverstein DC, Hopper K (eds): Small animal critical care medicine, St Louis, 2008, Saunders/Elsevier.
BOX 10-4 Biochemistry profiles: pediatric feline*
From Silverstein DC, Hopper K (eds): Small animal critical care medicine, St Louis, 2008, Saunders/Elsevier.
Radiographic interpretation can be challenging in pediatric patients if the veterinarian is not familiar with the normal anatomic differences in the young (see Chapter 21). The thymus can mimic a mediastinal mass or lung consolidation on thoracic radiographs. The heart can falsely appear enlarged and the lung parenchyma appears more opaque in neonates (because of higher water content). The liver appears to protrude further from under the rib cage than expected as a result of the absence of costochondral mineralization (making a misdiagnosis of hepatomegaly more likely). There is loss of abdominal detail because of the lack of fat and a small amount of abdominal effusion and this can be misdiagnosed as pathologic peritoneal effusion.
Although there are several significant differences in neonatal and pediatric pharmacology (see Chapter 27), cardiovascular drugs are the focus of this discussion. Cardiovascular drugs (e.g., epinephrine, dopamine, dobutamine, and so on) can be quite difficult to dose in neonates because of the individual variations in maturity of the autonomic nervous system. The autonomic nervous system is not mature until up to 8 weeks in neonates, and maturity occurs at different rates in individuals. Response to treatment and continuous monitoring of hemodynamic variables is essential when using these drugs. Elevations in heart rate after administration of dopamine, dobutamine, or isoproterenol cannot be predicted until 9 to 10 weeks of age, and the response to atropine or lidocaine is decreased in the neonate.
A normal neonate’s respiratory rate is about 2 to 3 times higher than an adult’s because of higher airway resistance and higher oxygen demand (Box 10-5). Drugs that depress respiration should be avoided in neonates. Neonates have a lower percentage of contractile fibers in their myocardium than adults and do not have the ability to increase cardiac output by increasing contractility (i.e., stroke volume). Since cardiac output is equal to stroke volume multiplied by heart rate, the neonate’s heart rate must be increased to increase cardiac output. Since the neonatal heart depends on a high heart rate to increase cardiac output, drugs that depress heart rate should be avoided. Although opioids are very good for analgesia because of their reversibility, the animal must be monitored closely, since these drugs have a propensity to depress heart and respiratory rates.