CHAPTER 64 Ectoparasites of Horses
Equidae around the world are afflicted by ectoparasites. In addition to annoyance from these parasites, some are capable of transmitting infectious agents and inducing hypersensitivity reactions, toxic reactions, and even death, if exposure is overwhelming. Some of these ectoparasites are ubiquitous and found in most locations where horses and other livestock live; some are reportable in certain countries; and some are highly contagious, spreading easily from animal to animal. Increasing international movement of horses as well as other livestock makes it important for the veterinarian to be able to anticipate, recognize, and treat ectoparasitic conditions early, preventing spread of equine and livestock diseases.
TICKS
Epidemiology
Life cycles among tick species may require one, two, or three hosts and a few weeks to 2 years to complete, depending on environmental conditions. Details of life cycles and hosts can be found elsewhere.1 With multihost ticks, the larvae and nymphs usually require small vertebrate hosts, while the adults feed on larger animals. Tick infestations occur in spring or summer months (the exception being the winter tick, Dermacentor albipictus) or nonseasonally in the tropics. In warm climates, if rainy and dry seasons are distinct, ticks will be more active during the rainy season. Most ticks live in forests, grasslands, and scrub, infesting passing animals. Some live in the burrows or nesting areas of the host, enabling them to reach the host easily whenever conditions are favorable.
Pathogenesis
Infectious agents are readily transmitted by ticks for several reasons: (1) ticks feed multiple times throughout their life cycle; (2) many infectious agents are transmitted during tick maturation to the next stage in the life cycle; (3) ticks take relatively large blood meals, which are concentrated by secreting the host’s own fluids back into the host directly or as coxal secretions; and (4) immunosuppressive substances are present in the tick saliva that reduce host defenses, allowing the microbe to become established.1 Heavy tick infestations can result in poor nutritional and immunologic condition and even anemia from blood loss. Tick paralysis results from salivary proteins found in females of some tick species, which secrete the neurotoxic proteins during feeding. Just one tick may cause partial paralysis, but a more severe or extensive paralysis may result from larger numbers of ticks feeding. Foals and ponies are more likely to be affected.1,2
Clinical Findings
Clinical syndromes resulting from tick infestation include (1) mild to severe papulonodular dermatitis, with or without pruritus; (2) otitis externa; (3) systemic infection with tick-borne agents such as Babesia caballi or B. equi (Chapter 59), Anaplasma phagocytophilum (previously E. equi, Chapter 42), Borrelia burgdorferi (Chapter 35), Francisella tularensis, and Theileria annulata; (4) anemia and poor condition; and (5) flaccid, ascending motor paralysis, particularly in foals or ponies.1,3,4
Diagnosis
Finding ticks on the horse is diagnostic. Identification of ticks is useful in determining which control measures will be most effective. Keys to aid identification can be found in parasitology texts and elsewhere.5,6,7 When exotic ticks are suspected or tick management problems arise, consultation with governmental authorities or a parasitologist for proper identification is strongly recommended.
Pathologic Findings
Histopathologic findings for tick-induced papules and nodules range from eosinophilic and neutrophilic perivascular dermatitis with dermal edema to intraepidermal vesiculopustular dermatitis. Chronic, nodular lesions often contain large numbers of lymphohistiocytic cells forming lymphoid nodule or follicles.8,9
MITES
Psoroptic Mange
Epidemiology
Mites are readily transmitted by direct contact or contact with fomites. Psoroptic mange mites live on the skin surface and feed by puncturing the epidermis, causing serous exudation, erythema, crusting, and pruritus. The female mite lays eggs in the surface debris. Eggs hatch within 2 to 3 days and develop to maturity within 11 to 14 days. Off-host survival of adult mites is shortest during periods of high temperature and low humidity. On average, survival on premises is 2 to 3 weeks but may be longer depending on conditions.10
Chorioptic Mange
Etiology
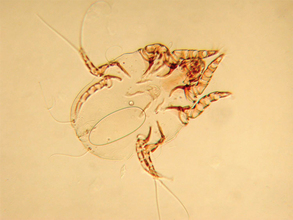
The most frequently diagnosed mange in horses, chorioptic mange is caused by the surface-living mange mite Chorioptes bovis (Fig. 64-1). As with the previously discussed mange mites, there is likely only one species of Chorioptes mites that infests several hosts.
Diagnosis
Diagnosis, by demonstrating the mite in superficial skin scrapings taken from multiple sites, can be difficult. Recommended techniques for catching these fast-moving mites include (1) using clear cellophane tape to pick up mites and crusts from the skin surface (although mites can be difficult to remove or position for identification, and parasitologists find such preparations frustrating); (2) adding insecticide to the oil used for the scrapings; and (3) vigorous brushing into a pan of soapy water. With the third technique, allow the mixture to settle out in a deep, narrow container. Decant and then centrifuge the settled material for microscopic examination of the pellet, or process the settled material as for fecal flotation.9,11 Field collections of crusts and debris can be placed in a blood sample tube for transportation to the laboratory for examination. In warmer weather the mites may only be obtained from scrapings of the coronary band.9
Therapy
Chorioptic mange can be difficult to treat because of its superficial location on the skin and mites’ ability to survive in the environment. Oral ivermectin is effective at reducing mite populations but cannot eliminate them.12 Effective topical treatments include a series of three whole-body baths, 5 days apart, using 1% selenium sulfide shampoo, and two treatments, 2 to 3 weeks apart, with 0.25% fipronil spray.13,14 Fipronil spray should be applied to all affected areas, including both the forelimbs and the hindlimbs from above the carpus and stifles, respectively, distally to the hoof and in sufficient quantity to dampen the hair and wet the skin. Other topical products that should be effective include 2% lime sulfur, organophosphate products, and synthetic pyrethroids. Ideally, the legs of heavily feathered animals should be clipped (owners often resist this for cosmetic reasons) and the legs thoroughly washed and skin debris removed before each parasiticidal application. Dips or washes may need to be repeated at 5- to 7-day intervals for 3 to 4 weeks. Care should be taken to apply these products to all areas vulnerable to infestation, including rear quarters, tail base, ventral abdomen and thorax, and even the head, if the horse is biting at or rubbing infected forelimbs with its head. One author suggests a combined approach using ivermectin systemically in combination with topical treatment.15 A key component to treatment is isolation of infested horses and treatment of the environment and fomites. All bedding should be removed from the stables, followed by thorough cleaning and treatment of premises with insecticide. If stalls or paddocks can be vacated for 3 or more weeks, there is less likelihood mites will survive in the environment. All bedding for infested horses should be replaced with fresh product daily, if possible, or on treatment days, at a minimum. Grooming and feeding equipment should be segregated, cleaned, and treated.
Demodectic Mange
Diagnosis
Microscopic examination of multiple deep skin scrapings or nodular contents should be sufficient to confirm diagnosis. Efforts should be made to detect underlying conditions making the animal susceptible to demodectic mange. Systemic glucocorticoid treatment is the most frequently implicated cause.9 However, endocrine diseases, other systemic diseases, nutritional factors, and immunosuppressed states should be considered.