5 Diseases of the Spinal Cord
LOCALIZATION OF AND FREQUENTLY ASKED QUESTIONS ABOUT SPINAL CORD DISEASES
See Tables 5-1 through 5-4.
Table 5-1 Clinical Signs of C1-C5 Spinal Cord Disease
Table 5-2 Clinical Signs of C6-T2 Spinal Cord Disease
| Other signs |
Table 5-3 Clinical Signs of T3-L3 Spinal Cord Disease
| Muscle tone | |
| Other signs |
Table 5-4 Clinical Signs of L4-S3/Cauda Equina Disease
| Muscle tone | |
| Other signs |
CONGENITAL AND HEREDITARY ANOMALIES AND DISORDERS
Atlantoaxial Instability
AAI can result from the following:
Dermoid Sinus
Dermoid sinuses have also been referred to as pilonidal sinuses and dermoid cysts.
Globoid Cell Leukodystrophy
Clinical signs are usually seen within the first few months of life, but can occasionally manifest after several years. Neurologic dysfunction, after it is clinically apparent, is progressive in nature. In dogs, the disease has two distinct clinical appearances. The first syndrome is dominated by a progressive upper motor neuron paraparesis. The second manifestation is primarily typified by evidence of cerebellar disease and is the most common clinical presentation in cats. Behavioral change, blindness, and hyporeflexia with muscular atrophy may also be seen in some animals. The clinical course of the disease is variable, ranging from one to several months, but is more rapidly debilitating in cats.
Myelodysplasia
Syringohydromyelia
DEGENERATIVE DISEASES
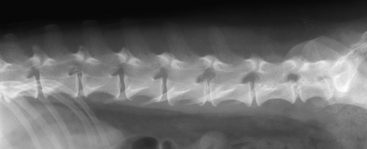
Intervertebral Disc Disease
The intervertebral disc is an anatomic structure located between each pair of vertebrae of the spinal column, with the exception of C1-C2, whose physiologic role is to provide resistance against deforming loads placed on the spinal column while simultaneously allowing for some flexibility. Each intervertebral disc consists of an outer annulus fibrosus, an inner portion called the nucleus pulposus, and two cartilaginous endplates.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree