Chapter 71 Diseases of the Liver and Biliary Tract
DIAGNOSTIC STRATEGY FOR LIVER DISEASE
Overview of the Diagnostic Strategy
Clinical Signs
Nonspecific Signs
Signs of Abnormal Bilirubin Excretion
Coagulopathy
Hepatic Encephalopathy
Signalment and History
Physical Examination
Skin and Mucous Membranes
Abdominal Palpation
Routine Laboratory Evaluations
Because clinical findings in hepatobiliary disease often are vague, hepatic disease may not be suspected until biochemical tests identify elevated liver enzyme activity or other evidence of hepatic dysfunction (e.g., hyperbilirubinemia or hypoalbuminemia). Liver function studies such as serum bile acid (SBA) concentrations are used to achieve the following:
Findings consistent with liver disease on routine laboratory tests are described below.
Complete Blood Count
Urinalysis
Liver Enzymes
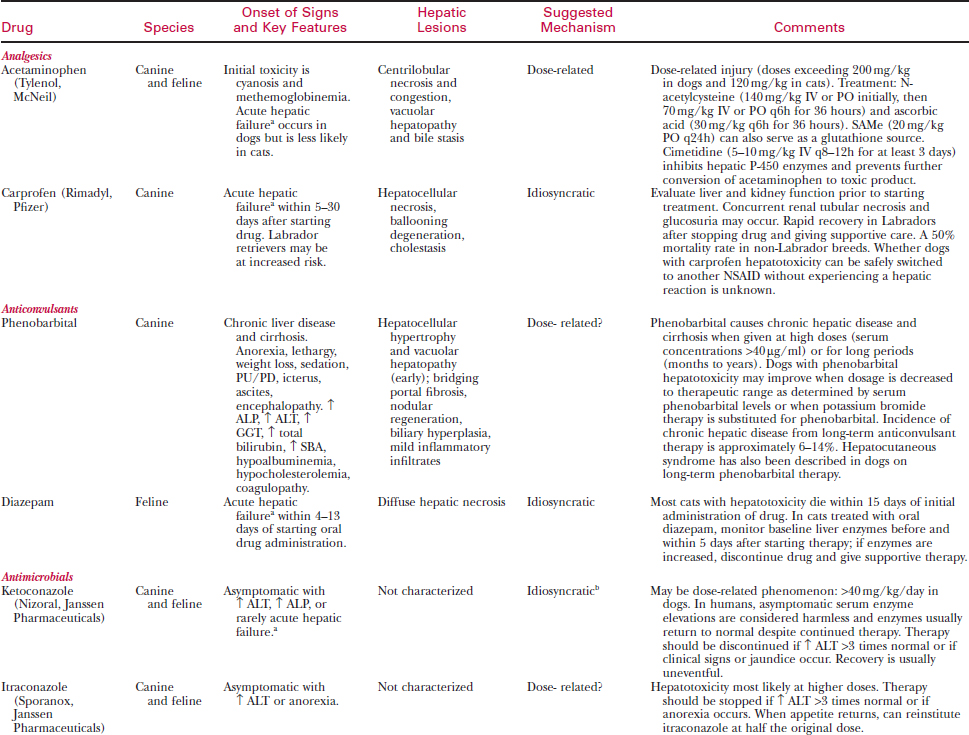
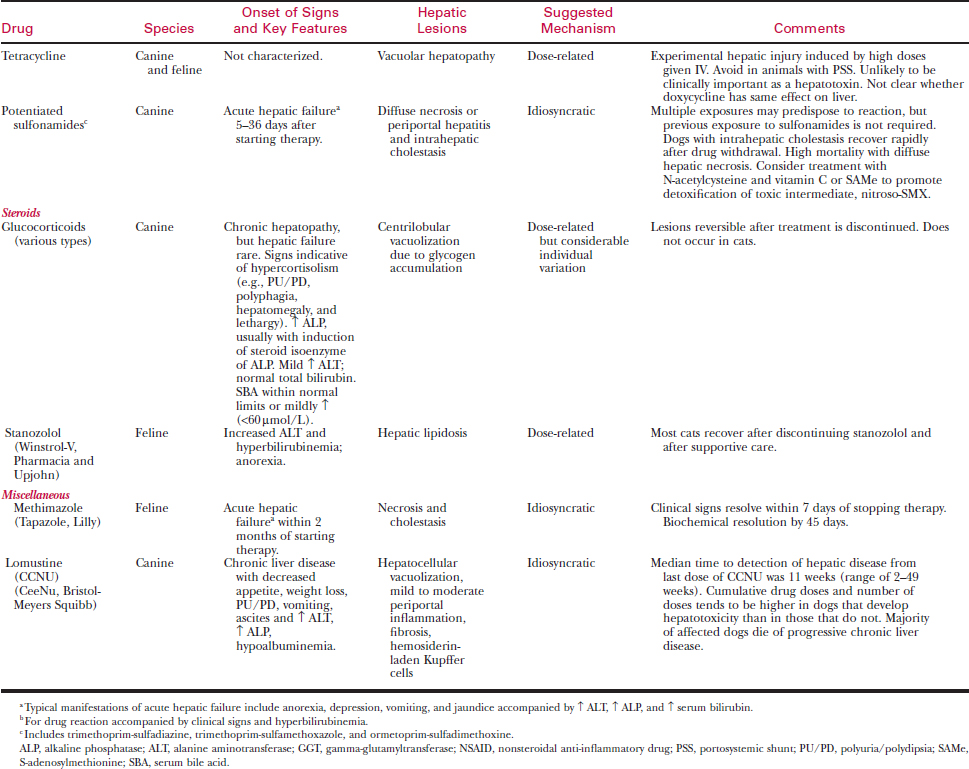
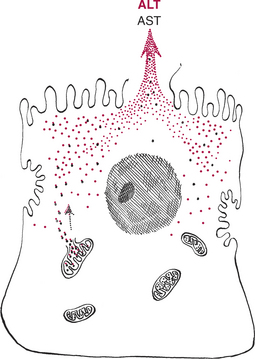
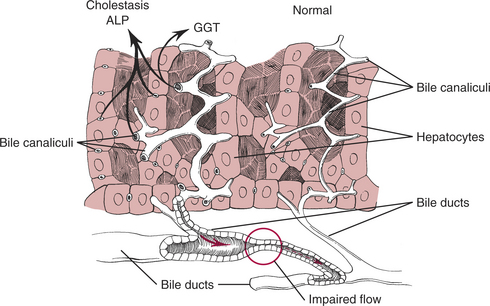
Evaluation of serum liver enzyme activity is used as a screening test to detect liver disease. Increases in liver enzyme activity are not specific for the underlying hepatic disorder. However, liver enzymes can be used to categorize the underlying pathophysiologic mechanism. Increases in liver enzyme activity may occur secondary to hepatocellular injury and leakage (Fig. 71-1), or due to increased production stimulated by bile retention (cholestasis) or drug induction (Fig. 71-2).
Alanine Aminotransferase
Increased alanine aminotransferase (ALT) activity indicates hepatocyte injury with leakage of enzyme from the cytoplasm of the hepatocyte (see Fig. 71-1). The magnitude of ALT increase generally correlates with the number of injured hepatocytes.
Aspartate Aminotransferase
Hepatocyte injury is associated with increased AST activity secondary to leakage from mitochondria and cytoplasm of hepatocytes (see Fig. 71-1).
Alkaline Phosphatase
Increases in serum alkaline phosphatase (ALP) activity are due to accelerated production of this enzyme, stimulated by cholestasis or drug induction (see Fig. 71-2). ALP is a membrane-associated enzyme present in many tissues; however, only liver, bone, and corticosteroid-induced isoenzymes contribute to serum ALP activity. Serum ALP activity in normal dogs and cats is usually due to the liver isoenzyme. An increase in this type of ALP activity indicates intrahepatic or extrahepatic cholestasis.
Gamma-Glutamyltransferase
This membrane-associated enzyme is present in many tissues. Increased serum gamma-glutamyltransferase (GGT) activity usually reflects cholestasis and increased production by hepatocytes (see Fig. 71-2).
Other Biochemical Tests
Bilirubin
Albumin
Globulin
Glucose
Cholesterol
Liver Function Tests
Serum and Urine Bile Acids
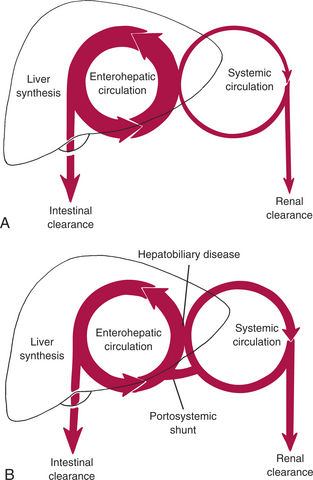
The normal physiology of bile acid metabolism is shown in Figure 71-3A In health, bile acids are confined to the enterohepatic circulation, and systemic concentrations are low. SBA concentrations increase in the systemic circulation with all types of liver disease (Fig. 71-3B). Because the liver has a large reserve capacity for synthesis of bile acids, even severe hepatic dysfunction does not cause decreased SBA concentrations.
Fasting Serum Bile Acid Concentration
Postprandial Serum Bile Acid Concentration
Urine Bile Acids
Recently, urine bile acids (UBAs) have been investigated as a diagnostic tool in dogs and cats. Normally only small amounts of bile acids are present in the urine. Liver disease and increased SBA result in increased excretion of bile acids in the urine. Potential advantages of UBA over a random FSBA are that UBA may reflect an average value over time, ease of sample collection, and lack of interference from oral ursodiol administration.
Blood Ammonia Concentration
Ammonia Tolerance Test
Parameters of Hemostasis
Coagulation Tests
Abdominal Fluid Analysis
Diagnostic Imaging
Survey Radiography
Abdominal radiographs are useful to evaluate for the following:
If hepatic neoplasia is suspected, take thoracic films to evaluate for pulmonary metastases.
Ultrasonography
Liver Cytology
Liver Biopsy
Biopsy Methods
Ultrasound-Guided Needle Biopsy
Laparoscopy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree