Chapter 65 Diseases of the Esophagus and Disorders of Swallowing
OVERVIEW
Clinical Signs
Regurgitation
Dysphagia, Odynophagia, Ptyalism, and Exaggerated Swallowing
These signs are most likely to occur with oropharyngeal and proximal esophageal disorders.
Diagnosis
Signalment
The signalment may suggest certain breed predispositions for esophageal disease (Table 65-1). The age at onset is also important because regurgitation caused by a vascular ring anomaly or congenital idiopathic megaesophagus usually begins at the time of weaning.
Table 65-1 PROFILES FOR ESOPHAGEAL DISEASE BASED ON SIGNALMENT
| Age | |
| Young | Vascular ring anomaly; idiopathic megaesophagus; foreign body |
| Mature | Esophageal neoplasia |
| Breed | |
| Abyssinian | Acquired myasthenia gravis |
| Akita | Acquired myasthenia gravis |
| Boston terrier | Vascular ring anomaly (PRAA) |
| Bouvier | Dysphagia due to hereditary muscular dystrophy (oropharyngeal dysphagia and megaesophagus) |
| Cocker spaniel | Cricopharyngeal achalasia |
| Collie | Familial canine dermatomyositis (oropharyngeal dysphagia and megaesophagus) |
| English bulldog | Vascular ring anomaly (esophageal compression by left subclavian artery and brachiocephalic artery) |
| Esophageal deviation cranial to the heart (normal variant) | |
| German shepherd | Idiopathic megaesophagus |
| Vascular ring anomaly (PRAA) | |
| Acquired myasthenia gravis | |
| Giant axonal neuropathy | |
| Golden retriever | Idiopathic megaesophagus |
| Acquired myasthenia gravis | |
| Cricopharyngeal dysphagia | |
| Great Dane | Idiopathic megaesophagus |
| Vascular ring anomaly (PRAA) | |
| Greyhound | Idiopathic megaesophagus |
| Irish setter | Idiopathic megaesophagus |
| Vascular ring anomaly (PRAA) | |
| Jack Russell terrier | Congenital myasthenia gravis |
| Labrador retriever | Idiopathic megaesophagus |
| Hereditary myopathy (megaesophagus) | |
| Miniature schnauzer | Idiopathic megaesophagus |
| Newfoundland | Idiopathic megaesophagus |
| Acquired myasthenia gravis | |
| Rottweiler | Spinal muscular atrophy (megaesophagus) |
| Shar-Pei | Idiopathic megaesophagus |
| Hiatal hernia | |
| Esophageal deviation cranial to the heart (mild regurgitation) | |
| Smooth fox terrier | Congenital myasthenia gravis |
| Springer spaniel | Cricopharyngeal achalasia |
| Polymyopathy (megaesophagus) | |
| Congenital myasthenia gravis | |
| Wire-haired fox terrier | Idiopathic megaesophagus |
| Terriers | Acquired myasthenia gravis |
| Siamese cat | Idiopathic megaesophagus |
PRAA, persistent right aortic arch.
History
Physical Examination
Radiography
Endoscopy
Treatment
Treatment of esophageal disease is discussed under each specific disorder. General management of esophageal disease involves fluid therapy as needed (see Chapter 5), management of complications such as secondary aspiration pneumonia (see Chapter 163), and in severe cases, nutritional support by tube gastrostomy (see Chapter 3).
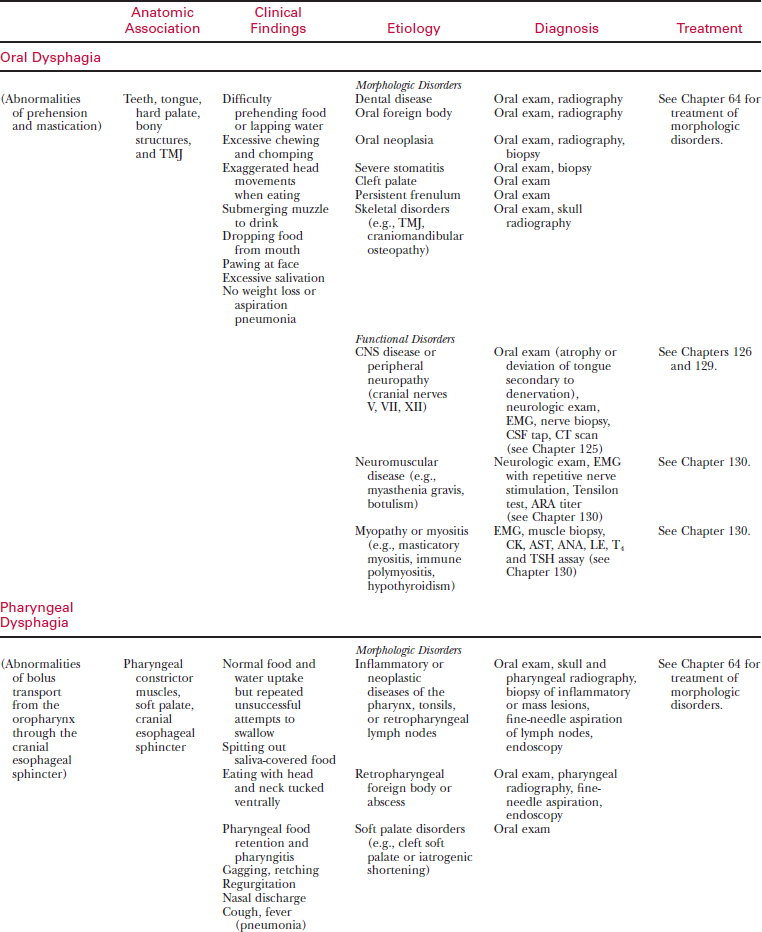
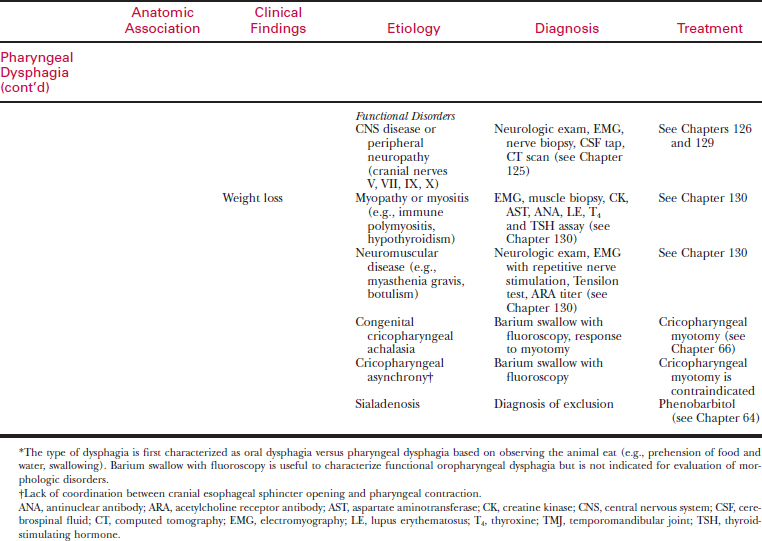
OROPHARYNGEAL DYSPHAGIA
Oropharyngeal dysphagia is defined as difficulty in moving a bolus of food or water from the oral cavity to the cervical esophagus. This disorder can be subclassified as oral dysphagia or pharyngeal dysphagia based on the clinical findings (Table 65-2).
Etiology
Oropharyngeal dysphagia usually is caused by morphologic disease that interferes with normal prehension and swallowing (see Table 65-2). Functional oropharyngeal dysphagia is associated with neuromuscular disorders that affect the tongue, muscles of mastication, or cranial nerves involved in voluntary and involuntary swallowing.
Clinical Signs
Diagnosis
The strategy for diagnosis of oropharyngeal dysphagia is as follows:
Signalment and History
The signalment may suggest certain breed predispositions for congenital neuromuscular disorders associated with oropharyngeal dysphagia (see Table 65-1). Obtain a complete history, including a description of eating and drinking. Evaluate for signs suggestive of aspiration pneumonia (cough, dyspnea, anorexia, depression) or a systemic neuromuscular disorder (weakness, muscle pain, gait abnormalities).
Physical Examination
Many of the morphologic diseases that cause dysphagia are detected initially by visual examination of the oropharynx. Tranquilization or general anesthesia may be required for a thorough oropharyngeal evaluation. A general physical and neurologic examination (see Chapter 125) are particularly important to identify focal and generalized neuromuscular abnormalities that may be associated with functional oropharyngeal dysphagia.
Radiography
Treatment
ESOPHAGEAL HYPOMOTILITY (MEGAESOPHAGUS)
Etiology
Table 65-3 CAUSES OF ESOPHAGEAL HYPOMOTILITY (MEGAESOPHAGUS)
Central and Peripheral Neuropathies
CNS (caudal brain stem) disorders (e.g., distemper, trauma, neoplasia)
Polyradiculoneuritis (coonhound paralysis)
Bilateral vagal nerve damage (e.g., surgery, trauma, neoplasia)
Hereditary spinal muscular atrophy
Neuromuscular Junctionopathies
Myasthenia gravis (congenital or acquired)
Polymyositis (e.g., SLE, idiopathic, infectious)
Familial canine dermatomyositis
Glycogen storage disease type II
Hypoadrenocorticism (typical and atypical forms)
CNS, central nervous system; SLE, systemic lupus erythematosus.
Clinical Signs
Diagnosis
Signalment and History
The signalment is important since idiopathic megaesophagus is a common disorder in young animals with regurgitation and certain breeds are predisposed (see Table 65-1).
Physical Examination
The physical examination is often unremarkable except for weight loss.
Radiography
Routine Laboratory Tests
Perform a minimum database of tests, including the following:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree