Chapter 126 Diseases of the Brain and Cranial Nerves
The brain may be anatomically and functionally divided into three major compartments, the brain stem, cerebellum, and cerebrum. Cranial nerves have their cell bodies within the brain, but most of their nerve fibers course outside the brain. Diseases of the brain and cranial nerves may be neoplastic, infectious, idiopathic, vascular, traumatic, metabolic, toxic, congenital, or degenerative in origin. These disorders may result in dysfunction of a focal, regionally specific brain area or may produce more diffuse or multifocal deficits. Because many different diseases can affect similar areas causing very similar clinical signs, the first portion of this chapter discusses clinical signs of lesions in each brain region. The remainder of the chapter discusses important brain diseases within each etiologic category. Diagnosis of neurologic disease is discussed in Chapter 125, and management of seizures is discussed in Chapter 127.
CLINICAL SIGNS AND NEUROLOCALIZATION
Brain Stem Lesions
Cerebellar Lesions
Forebrain Lesions
Herniation from Space-Occupying Brain Lesions
NEOPLASIA
Etiology
Primary Brain Tumors in the Canine
Primary tumors of the canine brain arise spontaneously and may grow slowly or rapidly.
Clinical Signs
Diagnosis
Laboratory Testing
Electrodiagnostic Testing
Radiography
Computed Tomography and Magnetic Resonance Imaging
Cerebrospinal Fluid Analysis
For CSF tap technique and normal values, see Chapter 125.
Treatment
Corticosteroids
Hyperosmotic Solutions and Diuretics
Anticonvulsant Therapy
Phenobarbital at a dosage of 2.2 to 2.5 mg/kg PO every 12 hours is indicated if seizures are part of the clinical picture (see Chapter 127). Potassium bromide is often required as an additional anticonvulsant if seizures are recurrent.
Specific Chemotherapy
Surgery
Radiation Therapy
Stereotactic Radiosurgery
INFLAMMATORY BRAIN DISEASES
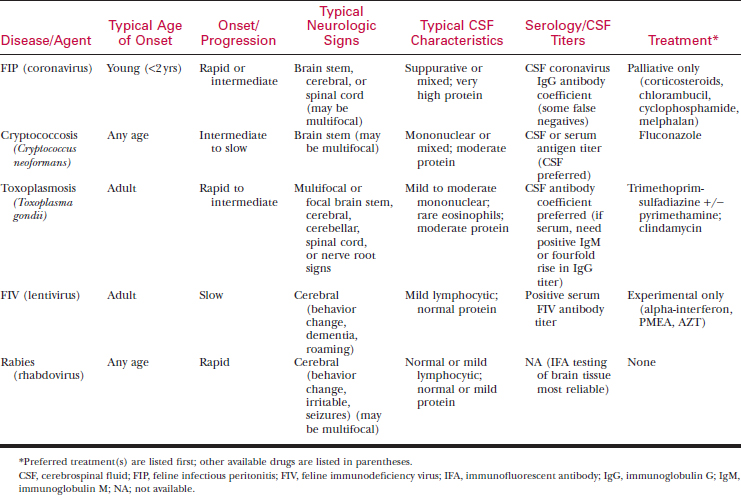
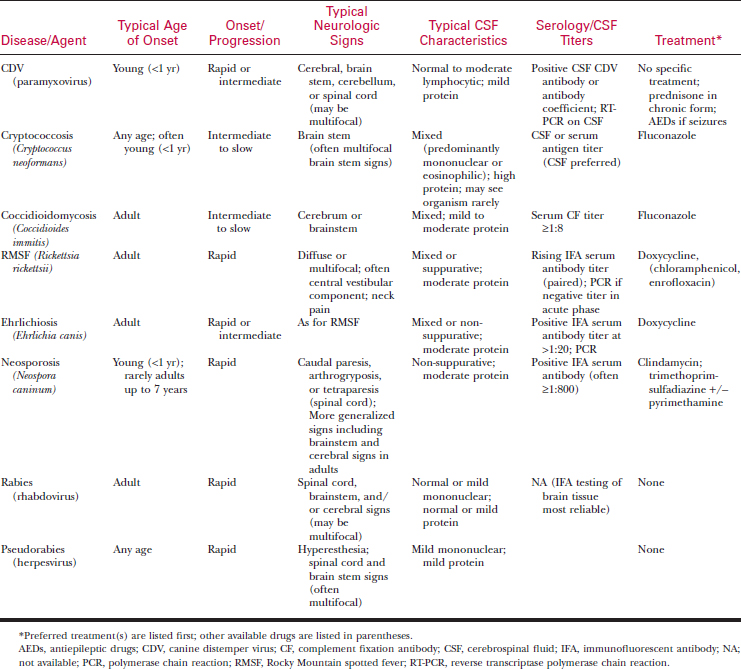
Infectious Meningoencephalitis
Etiology
Diagnosis
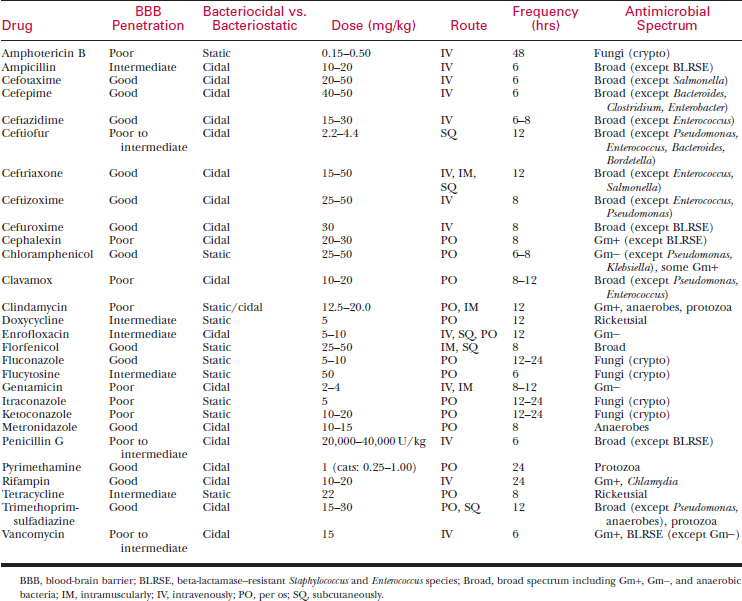
Treatment
IDIOPATHIC INFLAMMATORY BRAIN DISORDERS
Granulomatous Meningoencephalomyelitis
Clinical Signs
Diagnosis
Treatment
Necrotizing Encephalitis
Clinical Signs
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree