Geldings seem to be predisposed as well as horses with a special anatomical shape of the nephrosplenic space (Huskamp & Lopf 1980a; Huskamp 1987; Mariën 2002). The depth of the v-shaped nephrosplenic space might be important for entrapment (White 1990; Mariën 2002), and there is a wide variety among horses concerning the morphology of the nephrosplenic area (Huskamp & Lopf 1980a,b; Karlsbeek 1985; Huskamp 1987).
Diagnosis of left dorsal displacement of the large colon is generally based on rectal examination and confirmed by ultrasonography in questionable cases (Huskamp & Lopf 1980a; Santschi et al. 1993). In cases of severe meteorism of the ascending colon and/or the cecum, diagnosis can be confirmed more easily after cecocentesis and pressure relief (Huskamp & Lopf 1980a,b). Depending on the severity of the colic, medical therapy or surgical correction is indicated.
The reported recurrence rate of nephrosplenic entrapment is between 3.2% and 20.7% (Huskamp & Lopf 1980a; Baird et al. 1991; Hardy et al. 2000; Röcken et al. 2005). To prevent recurrence, different conventional surgical techniques, such as colopexy (Markel et al. 1988; Hance & Embertson 1992; Trostle et al. 1998), partial colon resection, and closure of the nephrosplenic space under general anesthesia by an open approach, have been described (Zekas et al. 1999). But because of the invasiveness and the perioperative morbidity, none of these surgical methods have often been recommended in the past (Mariën et al. 2001).
Since minimally invasive laparoscopic techniques have been published for ablation of the nephrosplenic space in a standing sedated horse (Mariën et al. 2001; Mariën 2002; Röcken & Mosel 2003; Röcken et al. 2005), this surgical procedure is well established in the relevant clinical case loads.
Surgical Procedure
Preoperative Preparation
Horses are placed on a low-residue diet (only pelleted feed) for 48 hours followed by a complete withholding of feed for another 24 hours before surgery to reduce the volume of ingesta in the large colon, with free choice of water. Tetanus prophylaxis and routine broad-spectrum perioperative antibiotics as well as non-steroidal anti-inflammatory drugs are administered.
Horses are restrained within standing stocks with their heads cross tied and are administered detomidine, butorphanol, and butylscopolamine to provide sedation and analgesia throughout the surgical procedure. A transrectal examination is performed to exclude that organs or intestine are located in the left paralumbar region.
Surgical Technique
The left paralumbar fossa is aseptically prepared and draped. This surgical procedure requires three portal sites that are infiltrated subcutaneously, intramuscularly, and subperitoneally with 20 mL of 2% mepivacaine each. The first portal is created in the paralumbar fossa with a 10-mm trocar-cannula system with a safety shield midway between the 18th rib and slightly dorsal of the ventral border of the tuber coxae. A 30° angled laparoscope is introduced and the abdomen is insufflated with CO2 to an intra-abdominal pressure of 5–10 mmHg to visualize the nephrosplenic region, to exclude any persistent displacement of the large intestine, and to create a space for further safe trocar placement (Figure 10.2).
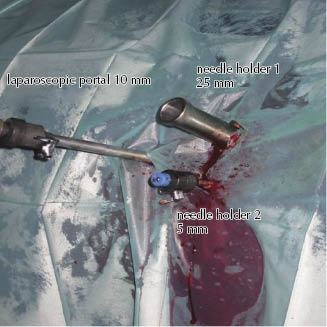
The second portal is placed in the 17th intercostal space at the same level as the ventral edge of the tuber coxae. The laparoscope is then removed from the first portal and introduced into the second portal, and the laparoscopic view is directed caudally in order to place the following two instrument portals under visual control. The third portal is created approximately 5 cm ventral to the first portal using a 5-mm trocar-cannula unit, and the first trocar is then enlarged and replaced by a valveless 25-mm-diameter trocar-cannula assembly, taking care not to puncture the spleen or the large intestine (Figures 10.3 and 10.4). The large-diameter cannula allows the surgeon to insert and to retrieve the 30-mm needle in the appropriate position in the jaws of the needle holder.
Figure 10.3 Laparoscopic portal 1 (10 mm) positioned left-sided in the 17th intercostal space, instrument portal 2 (25 mm) and 3 (5 mm) created in the left flank.
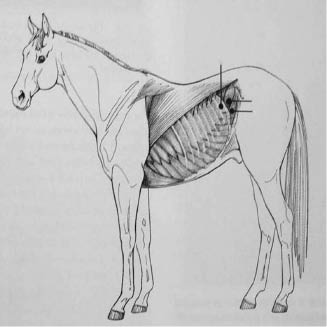
Figure 10.4 Laparoscopic portal sites, laparoscopic portal (10 mm) positioned left-sided in the 17th intercostal space; the two instrumental portals (25 mm) and (5 mm) are created in the left of the flank.
A one-half circular cutting needle attached to a 240-cm-long size 1 USP monofilament absorbable suture (Biosyn, Covidien, Mansfield, MA) is grasped with the laparoscopic needle holder and introduced intra-abdominally through the first portal (Figure 10.5A). A second needle holder is inserted through the ventrally located third portal.
Figure 10.5 Insertion of needle holder 1 through a big-sized instrument portal (A); the first bite is made through the perirenal fascia (B) in a dorsal to ventral direction by using a one-half circular cutting needle attached to a 240-cm-long size 1 USP monofilament absorbable suture (Biosyn) (C).
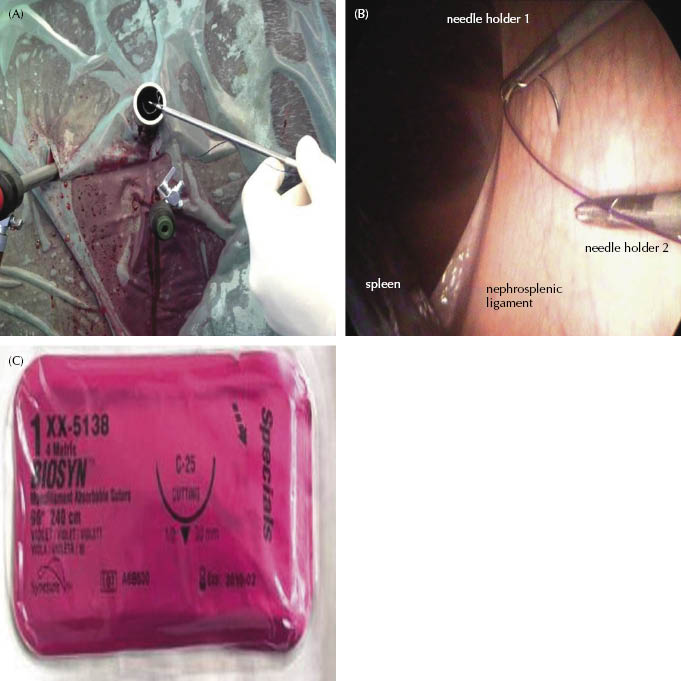
The nephrosplenic space is closed by apposing the perirenal fascia to the dorsomedial splenic capsule in a cranial to caudal direction. This procedure needs no additional local anesthesia. The first bite is made as cranial as possible through the perirenal fascia approximately 3 cm above the dorsal border of the spleen in a dorsal to ventral direction (Figure 10.5B). The needle is grasped with the second needle holder and replaced in the jaws of the first one. The needle is then passed through the dorsomedial splenic capsule at the same level in a ventral to dorsal direction and is retrieved extra-abdominally with the first needle holder (Figure 10.6). For the initial fixation of the continuous suture, the needle is passed through a small loop that is made at the end of the suture and then tightened (Figure 10.7). The needle is reinserted through the first portal, and the second bite is accomplished in the same fashion with an approximate interval of 1.5 cm to the first bite. Meanwhile, the suture is tightened and held in position by the assistant surgeon after each throw. Closure of the nephrosplenic space is completed by continuing this procedure (Figure 10.8). The smaller the angle between the dorsomedial splenic surface and the lateral perirenal fascia, the less tension is needed to appose these two tissues. Also, tension is normally decreased by advancing of the continuous suture. In the case of an extremely large-angled nephrosplenic space, the angle can be decreased and suture tension subsequently diminished by injecting the spleen at three to four places with 1 mg epinephrine diluted in 10 mL of sterile saline solution. At the end of the nephrosplenic space, a modified Roeder knot or alternatively a surgeon’s knot followed by a square knot is tied and tightened with a knot pusher or by using the needle holder (Figure 10.9).
Figure 10.6 The needle is then passed through the dorsomedial splenic capsule in a ventral to dorsal direction.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



