Figure 4.3 Animals may have very different experiences of treatment to human patients. (Courtesy of SPCA Hong Kong.)

Sometimes we can refer to gold standard treatments described in textbooks. However, textbook advice is like scientific findings in that it needs to be adapted to individual clients. There is no such thing as best practice in the sense of a treatment that should always be done. What is right for each patient is a bespoke practice that fits with the particular animal’s individual personality, circumstances and takes into account the relevant owner-based, financial and other constraints. (Remembering this may help practitioners to feel less frustrated or guilty for providing such treatments – they are best for this case, and this more complex problem-solving is part of the skill of veterinary practice.)
In some cases we might respect our clients’ wishes, as human doctors do. However, veterinary professionals should not unthinkingly leave decisions to clients, nor simply transpose decisions from human medicine. Human patients are very different to animal patients, and veterinary professionals’ duties are very different to human medical professionals’. Applying human treatment choices is a form of anthropomorphism and should be done critically by considering human–non-human differences. Humans may have very different biology, pathology, pharmacology, psychology and experience of treatment. Humans may want to see their grandchild’s wedding, feel guilty for taking up resources, fear the afterlife, understand treatment, consider their life as sacred and have human dignity, all of which may not apply to animals (Figure 4.3). Similar considerations guard against egomorphically choosing the option you would want if you were the patient. It is often better to ignore what is good for humans and instead to choose veterinary treatments based on more basic evaluations and clinical reasoning.
Ideally, clinical choices should be based on future welfare evaluations, by choosing the option with the best balance of costs and benefits. This cost–benefit analysis method can consider one stakeholder or several. Some decisions concern only individuals (discussed in Section 4.2), others concern multiple animals (Sections 4.3 and 4.4) and others concern animals and humans (Sections 4.5, 4.6, 4.7 and 4.8). Each of these involves increasingly wider considerations and decision-making.
THE ANIMALS
4.2 Individual Patients
Treatments may affect animals’ welfare in many different ways. They may directly prevent feelings (e.g. analgesia or anxiolytics) or cause them (e.g. nausea or dysphoria). They may avoid the causes of feelings (e.g. curative medications), mask their symptoms (e.g. some uses of sedatives) or increase the risk factors for such causes (e.g. through nephrotoxicity or surgical lesions). They may also extend life or shorten it (e.g. through deliberate euthanasia or through risky procedures).
There is no categorical list of what treatments are in patients’ interests. Bespoke practice will therefore vary for different patients. Medications can be contraindicated by allergies or concomitant diseases. Hospitalisation or frequent visits can be contraindicated by severe vet-fear. Long courses of medication or risky procedures may be contraindicated by anticipated owner non-compliance, inability to fund future treatment for complications or likely unwillingness to consent to later euthanasia. Breed, lifestyle and human–animal relationships mean different animals have varying background risks of disease or expected lifespans. The right treatment for each case depends on the individual animal and its particular circumstances.
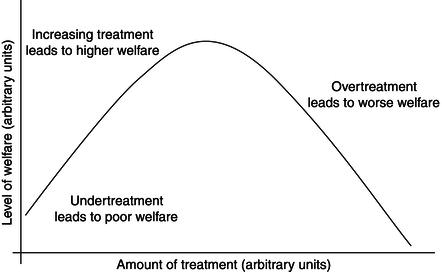
In general terms, there are two types of mistreatment (Figure 4.4). Undertreatment is where animals do not get treatments that could be provided and that would be in their interests. Overtreatment is where animals get any treatment that is not in their interests, compared to more conservative options such as (a) no treatment or (b) euthanasia. It is impossible to give a definitive list of overtreatments or undertreatments, but higher risk treatments that may be more likely to constitute overtreatment are suggested in Table 4.1.
Often, mistreatment involves both undertreatment and overtreatment. If a patient receives an ineffective antibiotic, then it both lacks a worthwhile treatment and receives a potentially harmful drug. Similarly, surgery without adequate analgesia may be both undertreatment insofar as the animal does not receive required painkillers and overtreatment insofar as the animal may be better off without the highly painful surgery.
Table 4.1 Categories of overtreatment and examples that may be overtreatment for some individuals (after Yeates 2010b).
| Comparison | Acute | Chronic |
| More conservative treatment | Performance-enhancing or cosmetic surgery Removal of benign tumour | Chemotherapy for “surgical tumour” Excessive prophylaxis Unnecessary disease monitoring |
| Euthanasia | Large-scale tissue resection (other than limb) Hoisting a long-term cast horse or downer cow | Perpetuation of life of suffering patient Poorly tolerated chemotherapy Long-term hospitalisation of wild animal |
Choosing the bespoke treatment should be based on evaluations of the patient’s future welfare for each treatment option, including no treatment and euthanasia. The option that is evaluated as best is the one that should be prioritised. This evaluation may be based on qualitative evaluations, such as criteria like extreme suffering (which is not easily defined), hierarchies or binary criteria. Such methods may be especially useful for planning and communication with owners, as they are easy to understand and can set objective thresholds. For example, binary methods work well when it is clear what each change will mean – for example, that a change in any sole parameter is sufficient to prescribe euthanasia. If this is not clear, and some parameters worsen and others improve, then we still need to make a judgement about which are more important.
Figure 4.5 Anaesthesia itself does not involve feelings, and hence can be given neutral value in quantitative methods (although the feelings during induction and recovery do involve feelings that should be considered). (Courtesy of RSPCA Bristol.)

Qualitative methods are not good at taking risks into account. For example, we may think a small risk of extreme suffering or failing to satisfy a vital need does not outweigh a high probability of achieving a better outcome (otherwise this would rule out any non-life-saving treatments or euthanasia). Risk is more easily handled by quantitative methods which consider the severity, duration, frequency and likelihood of pleasant and unpleasant feelings that will occur in the different possible outcomes for each option. For example, pleasant life may have positive value, suffering a negative value and the absence of feelings such as anaesthesia a neutral value (Figure 4.5). Quantitative decision-making can be based on thresholds applied to the quantitative assessments discussed in Section 3.7. For example, Table 4.2 suggests some decision-making thresholds based on Table 3.6.
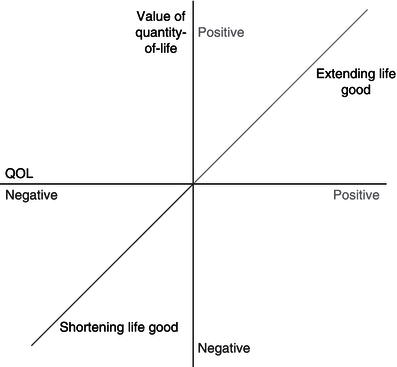
Because quantitative methods involve a consideration of the duration of future feelings, they need to consider the animal’s expected longevity and welfare for each option, so quality-of-life and quantity-of-life can be balanced. One approach is to consider extended life as being worth achieving or avoiding based on the expected quality-of-life (FAWC 2009; Yeates 2011b, 2012b). Animals may be kept alive if their future life is expected to involve good feelings that outweigh the negative feelings, i.e. they have a life-worth-living. Animals should be euthanased if death is in the animal’s interests (Yeates 2010c). Death is in an animal’s interests when their future life is expected to involve more suffering than enjoyment, i.e. they have a life-worth-avoiding (Wathes 2010; Yeates 2011b). This means that quantity-of-life is not a separate value to quality-of-life, but that the value of quantity-of-life depends entirely on the animal’s expected quality-of-life (Figure 4.6).
Table 4.2 Guide to interpreting overall positive and negative summated scores (adapted from Morton 2007).
| Score | Interpretation | Prescription |
| +5 to +11 | Has a life-worth-living | Major adjustments should be avoided |
| 0 to +5 | Major adjustments not warranted, but would benefit from some changes | |
| –7 to 0 | Has a life-worth-avoiding | QOL should be improved immediately (e.g. within 1 week) |
| –8 to –15 | Major changes needed, alongside regular review of treatment and prognosis | |
| –16 to –24 | Euthanasia mandated unless high chance of improvement within 3 days |
Veterinary professionals should work out whether a patient’s life would be worth living or worth avoiding when one’s options include euthanasia, a life-saving treatment (e.g. resuscitation) or an intervention that could constitute overtreatment. But how do we work out whether a life is worth living or avoiding if it involves a mixture of periods of good and bad welfare? And what about comparing between treatments that both lead to a life-worth-living but vary in the lifespan and quality-of-life? In these cases, a more complex method to balance quality-of-life and quantity-of-life is required.
The idea of quality-adjusted-life-years (QALYs) is used in human medicine to decide how to allocate funds for different treatments for different people, but we can also use them to decide between treatments for an individual patient. The basic idea is that each treatment option is rated in terms of the longevity that it is expected to provide multiplied by the overall quality-of-life that the treatment would provide. In human QALY calculations, quality-of-life is usually rated as “1” when the patient is completely healthy and poorer quality lives are scored between 0 and 1 (Harris 1987). Veterinary practitioners might use shorter periods than years – such as quality-adjusted-life-months (QALMs). These are calculated using the formula in Box 4.1. So, for example, 6 months with perfect welfare would score 6 × 1 = 6 QALMs, whereas 1 year with quality-of-life of score 0.3 would score 12 × 0.3 = 4 QALMs. The first treatment would therefore be chosen.
This concept can fit with the ideas of a life-worth-living and a life-worth-avoiding, by considering using negative quality-of-life scores. Medical assessments usually consider human life to always have positive value (Kaplan et al. 2007), but we can score animal’s lives-worth-avoiding as less than 0. Death is rated as 0, not because being dead prevents any feelings, but simply because it involves 0 life years (and 0 times any quality-of-life score equals 0).
Of course, animals’ lives are not always of unvarying quality-of-life. Most treatments provide a number of periods in which animals may experience a different quality-of-life. Animals’ lives are also not entirely predictable. Most treatments provide a number of risks of possible longevity and quality-of-life. Ultimately, this concept can be made even more sophisticated by working out the quality-of-life for each of the different periods of life that each treatment would provide and the probability that each period will occur. These can be multiplied to create an overall qualitative assessment, which we might call quality-adjusted-life-periods (QALPs), using the steps described in Box 4.2. These effectively lead to the formula in Box 4.1.
Figure 4.7 In quantitative methods like QALYs, the age of an animal will alter their life expectancy. (Courtesy of RSPCA Bristol.)

Using QALYs have disadvantages. It has certain inherent biases, such as preferring life-saving treatments for younger animals, with which not everyone may agree (Figure 4.7). The calculations may be difficult and counter-intuitive and may seem coldly uncaring, especially for life and death decisions. The conclusions may conflict with more intuitive clinical decisions and may be ignored. This means that, until the method has been developed and validated, QALYs would be used best as a device to assist reflective decision-making but not to definitively determine treatment choices.
4.3 Decisions Affecting Multiple Patients
In many cases, we have to consider multiple animals, such as a whole flock or herd, or when transplanting blood or kidneys from one animal to another, or when considering practising or experimenting on our patients.
Some cases are simple because one option is in every animal’s interests. Some treatments may improve every animal’s welfare, for example, better fly control and dagging to avoid the need for tail-docking may benefit every lamb. Other treatments may be worthwhile for every animal, even if they only benefit some animals and even harm others; for example, vaccinating a flock may cause some vaccination reactions but is still indicated for each individual. Similarly, one may reduce post-ovariohysterectomy haemorrhage rates by double-ligating ovarian vessels, but the slower surgery time may increase anaesthetic risks, such as post-anaesthetic dysphoria or post-operative mortality. If the risks of haemorrhage outweigh the anaesthetic risks, then double-ligation is in the interests of each individual patient, even though some unlucky patients are harmed.
Other cases are more complicated because they involve ignoring or harming some animals in order to benefit others. For example, one might have to decide whether to kill a few members of a herd for post-mortem, isolate an individual to prevent infection or de-horn steers or tooth-clip piglets to prevent them harming others.
For these cases, veterinary professionals may use quantitative methods to aggregate the welfare of all animals involved. For example, tail-docking causes sheep pain and distress but may prevent a proportion of the sheep suffering from fly-strike. In the case given in Box 4.3, the calculation suggests the decision should be not to tail-dock the lambs. This decision is highly case-specific – for example, it would suggest that tail-docking should be done if the expected incidence of fly-strike in non-tail-docked lambs increased from 4% to 5%. So the method could lead to different decisions in other situations, e.g. for store lambs, November lambing, easy-care lambs, for mulesing instead of tail-docking, if fly-struck lambs were euthanased earlier, etc.
An alternative approach is to use a hierarchical method that prioritises certain outcomes over others. One hierarchical method is to use a bottom-up rule to choose whatever option improves the welfare of the worst off. Another hierarchical method is a rights-based rule to reject any option that causes any animal to have welfare below a certain level, for example a life-worth-avoiding. For example, in the tail-docking decision in Box 4.3, we might think that avoiding any animal experiencing the catastrophic event of fly-strike is more important than preventing minor pain and distress (even in a larger number of animals). This would suggest we should subject all animals to tail-docking (even if only 1% of the flock would be expected to get fly-strike).
In practice, one may choose to use a combination of hierarchical and quantitative approaches. One may think that one should avoid certain severe harms to any individual (e.g. substantial suffering), but that more minor harms can be balanced across individuals using quantitative methods.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree