Donated blood should not exceed 20% of the blood volume of the donor, which equates to about 1.5% of the donor’s body weight. It is often encountered that the donor is unable to give the volume of blood that is required to achieve the desired PCV using the above formula. In these cases, if a donor of greater body weight cannot be obtained, the safe donor volume must be administered and a lower PCV achieved.
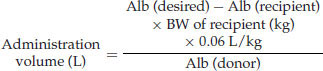
In the case of hypoproteinemia caused by hypoalbuminemia, hypoglobulinemia, or panhypoproteinemia, whole blood may also be administered where plasma is unavailable using the following formula (using albumin as the target protein):
When the collection and administration volumes are calculated, the donor is restrained in the standing position (preferably in a chute) and the catheter connected to the appropriate receptacle containing anticoagulant. The container is lowered to the ground and filled by gravity flow. In the case of commercial blood collection bags (Figure 73.1), they should be filled until turgid and then rocked to assure proper mixing of the blood and anticoagulant. Where these bags are not available, any sterile receptacle may be used. Sodium citrate is added to the receptacle at a volume to create a 1 : 9 ratio of sodium citrate:whole blood.
Figure 73.1 Acid citrate dextrose blood collection bags. These commercially available bags come as a set of three for separating blood components, but only one of the bags is used for whole blood collection.

After the desired volume is collected, the bag is attached to a filtered administration set (Figure 73.2) and administration to the donor initiated. The transfusion should begin at a slow rate of 5 mL/kg/hour for the first 15 to 20 minutes and the recipient monitored for signs of transfusion reaction. After this time, if no abnormalities are noted, the rate may be increased to 10 mL/kg/hour for the remainder of the transfusion.
Figure 73.2 Filtered blood transfusion administration set. These should be used to prevent microscopic clots and fibrin from being transfused.

In cases where acute hemorrhage is the cause of anemia, the bleeding must be stopped prior to or during the transfusion, because the volume expansion will worsen the losses. In the case of hemolytic disease, efforts should be made to identify the cause and minimize ongoing hemolysis, because the average lifespan of transfused red blood cells is limited to 3 to 5 days. Severe anemia may be recognized during the physical examination by inspection of the mucous membranes. Extreme anemia causes a pale appearance (Figure 73.3). Assessment of the anemic patient should include examination of peripheral blood. This may allow identification of Mycoplasma haemolamae infection of red blood cells (Figure 73.4).
Figure 73.3 The mucous membranes of an alpaca presented for weakness and lethargy. Note the extreme pallor. This animal had a packed cell volume of 9%, was tachycardic, tachypneic, and recumbent.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


