Chapter 11 Anesthesia and Pain Management in Dental and Oral Procedures
There is a vast amount of information about anesthesia that is beyond the scope of this book in terms of the nuances, idiosyncrasies, and precautions, that should be investigated more thoroughly by the reader. This chapter is intended to serve as a user-friendly guide to some convenient anesthesia protocols, routes of administration, and management suggestions before, during, and after operative dentistry on the small animal patient.
GENERAL ANESTHESIA
General Comments
• General anesthesia is a necessary part of most dental procedures to provide immobility required for safe and total access to the oral cavity.
• Dental patients are usually categorized, according to the American Society of Anesthesiologists (ASA) classification, as class I or II (normal patient or patient with mild systemic disease; see below). An exception to this may be the geriatric patient or the patient that is immunologically or metabolically compromised.
• Safe anesthesia protocols are available, even for young puppies and kittens, so they can be placed under general anesthesia for various dental procedures such as interceptive orthodontic extractions.
• General anesthesia is often a major concern of the client, particularly when multiple sessions are required.
• A significant portion of the cost of any dental procedure is generated by anesthesia, supportive measures during anesthesia, and preoperative laboratory evaluations.
• Monitoring the physiologic changes that occur during anesthesia, such as hypothermia, hypotension, and cardiorespiratory depression with appropriate intervention, will help to ensure a safer anesthesia session.
• With proper attention to their physiologic needs, healthy geriatric patients or patients with mild systemic diseases can be anesthetized safely. These patients can be treated for their dental disease and will benefit from improved oral health.
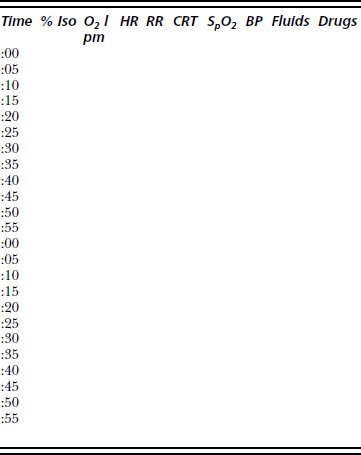
• Anesthesia records should include administration time, route, and duration of anesthetic drugs; dosages used; fluids administered; catheter type, size, and location; endotracheal tube size; monitoring parameters; and vaporizer settings and oxygen and nitrous oxide flow rates. The anesthesia record should continue until the patient can maintain sternal recumbency unassisted.
• Charting heart rate, respiratory rate, and any other parameters monitored is a necessity. Any anesthesia complication or excessive delay in recovery should be noted so that future anesthesia protocols can be adjusted (Table 11-1).
• To reduce the incidence of aspiration during anesthesia, food should be withheld for 12 hours prior to induction of anesthesia, except to prevent hypoglycemia in young patients and diabetics. Water should be available to the patient until the morning of the procedure.
Chart: American Society of Anesthesiologists (ASA) Classifications1
• Age is not a factor in assigning risk. While many healthy older patients may have early organ dysfunction, it poses no greater risk than to a young patient with equivalent organ dysfunction. Patient evaluation prior to anesthesia includes (1) signalment (species, breed, age, and sex), (2) a complete physical examination, (3) the chief complaint, and (4) the medical history.
Preprocedure Workup
• The decision to perform preanesthetic laboratory workups, and the degree of comprehensiveness of such workups, will vary based on several factors including the laboratory capability of the practice, the age of the patient, the physical examination findings, the anxiety level of the client over the procedure, and even the timing of the procedure. Remember that normal laboratory values do not ensure a safe, successful anesthetic episode but rather are screening for problems in one of three categories: (1) immediate life-threatening problems, (2) problems necessitating changes in the anesthesia protocol, and (3) problems that are more longstanding that will require follow-up subsequent, and unrelated, to the anesthesia. Most problems identified will fall in category 3 and less often in category 2. Rarely will a life-threatening problem be identified solely by laboratory values.
• A basic preanesthesia profile should include packed blood cell volume (PCV), total blood protein or solids value, and urine specific gravity. Other tests may be added based on the patient evaluation. It is often recommended that young healthy patients have a PCV; total protein, blood glucose, and blood urea nitrogen levels; and a urine specific gravity performed. Older patients or those with significant findings in their initial physical examination should have a complete blood count and chemistry profile performed as a minimal database. Additionally, tests for thyroid function, feline leukemia, and feline immunodeficiency virus (for cats), complete urinalysis, electrocardiogram, ultrasonographic examinations, and thoracic radiography should be scheduled, depending on the patient’s condition and the client’s permission.
• Other considerations for determining the anesthesia protocol include weight, temperament, procedure to be performed, length of anticipated procedure, concurrent diseases (e.g., epilepsy, heart disease, kidney disease, liver disease, endocrine disease, gastrointestinal disease, or bleeding disorders), medications administered previously or concurrently, previous anesthesia experiences, and dietary history.2
Preanesthetic Medications
Comments
• Preanesthetic medications are used to reduce the anxiety level of the patient, provide preemptive analgesia, reduce the amount of induction and maintenance drugs and, on occasion, to reduce the volume of secretions.
• These drugs usually are given intramuscularly 10 to 30 minutes prior to the induction of general anesthesia.
• In select instances they can be administered intravenously immediately before the induction agent. This route should not be used for routine administration of premedication due to the possibility of rapid changes in cardiorespiratory function. Dosages should be reduced by at least 50% when these drugs are administered intravenously.
• Intravenous administration in compromised patients may cause a more profound effect than desired; it is preferable to administer these drugs intramuscularly.
Anticholinergic Agents
Comments
• To maintain heart rate and hence cardiac output in patients receiving vagotonic drugs, such as α2-agonists and opioid agonists, patients who may be subject to strong vagal reflexes, or those patients whose cardiac output is heart rate dependent, such as very young patients, patients with significant cardiac disease (i.e., hypertrophic cardiomyopathy), procedures in the oropharynx, or inadvertent application of ocular or carotid pressure.
Atropine
Advantages
• Can be given intraoperatively to increase heart rate if a significant sinus bradycardia or second-degree atrioventricular (AV) block develops.
Tranquilizers and Sedatives
Comments
• Reduce nervousness, reduce the amount of induction agent required to allow intubation, smooth the transition to and from general anesthesia, and reduce the amount of anesthetic drug required to maintain anesthesia.
Phenothiazine Derivatives
Comments
• The α-adrenoreceptor blockers, +/− antihistaminergic, +/− antidopaminergic, depending on chemical structure changes.
Acepromazine
• In the dog, as the dosage is increased there is a concomitant increase in magnitude of adverse or undesirable effects. If increased sedation is desired, it is recommended that opioids be administered with the acepromazine to prevent excessive vasodilation, hypotension, and hypothermia associated with increased dosages of acepromazine.
• Dogs with quiet, calm temperaments and older dogs will require only the low end of the dosage range in order to achieve adequate sedation.
Benzodiazepines
Comments
• Disinhibition occurs in approximately 25% of veterinary patients, with resultant transient excitation following intravenous administration. Most common in young adult, normal, healthy patients.
Advantages
• When combined with a dissociative agent (i.e., ketamine or tiletamine), can be used as a combination induction agent or to provide short-term anesthesia.
• When used with an opioid medication, provides good sedation and tranquilization in older or quieter patients.
Alpha2 Adrenoreceptor Agonists
Comments
• Drugs in this group are sedative-hypnotics and will result in a quiet to minimally responsive patient. As the dosage is increased, a state resembling hypnosis can be achieved such that the patient is essentially unresponsive to external stimuli. However, anesthesia is not achieved, even at high dosages.
• Significant cardiorespiratory depression can occur with the drugs in this class. Manipulation of chemical structure has reduced this effect in many of the newer drugs. Bradycardia and peripheral vasoconstriction are the most common undesirable effects.
• Alpha2 receptor activation prevents release of norepinephrine from the presynaptic nerve terminal, with a resultant lack of stimulation of postsynaptic neurons.
• To date, all α2 agonists also have α1 activity, although the relative α2-to-α1 activity varies significantly among the drugs in this class.
• Because of the profound cardiac depression, it is recommended these drugs be administered intramuscularly whenever possible.
Advantages
• Used in conjunction with ketamine to provide chemical restraint resembling anesthesia and may be suitable for minor procedures.
Disadvantages
• Profoundly vagotonic, resulting in bradycardia that can be prevented with the use of an anticholinergic agent. Bradycardia is due to a direct cholinergic effect as well as activation of the baroceptor response.
• Profound vasoconstriction occurs due to α1 activation, resulting in an increase in the systemic vascular resistance.
• The ratio of α2-to-α1 activity is 160:1, indicating a significant α1 effect in addition to the desired α2 effect.
• Use of α2-antagonists other than yohimbine may not reverse cardiovascular or gastrointestinal effects.
Advantages
• Bradycardia is a physiologic response due to the baroceptor response to vasoconstriction (α1) as opposed to a cholinergic effect.
• When used in combination with opioids or dissociatives, there is a significant dosage reduction in medetomidine.
• Significant minimum alveolar concentration (MAC)-sparing effect and induction dosage requirements when used as a premedicant.
Opioids
Comments
• Opioids used as a preanesthetic medication provide analgesia as well as sedation (synergistic when used in combination with a sedative-tranquilizer).
• Administering opioids as preanesthetic medication can reduce dramatically the amount of anesthetic agent required to maintain anesthesia.
• Morphine, oxymorphone, and hydromorphone (opioid agonists) produce greater pain relief, but also greater sedation.
• Meperidine (Demerol) is significantly less potent than morphine, oxymorphone, or hydromorphone and has a short duration of action (2 to 3 hr). It is the only opioid that causes vagolytic and negative inotropic effects at clinically used dosages.5 As such, it should be used cautiously in debilitated patients, as well as in those with hypothyroidism or hyperthyroidism, severe renal insufficiency, and adrenocortical insufficiency. It also causes significant histamine release and therefore should not be administered intravenously.
• Fentanyl is a very short-acting opioid agonist that causes significant bradycardia and respiratory depression when administered intravenously or intramuscularly.
• Buprenorphine is a partial opioid agonist (mu). It provides adequate analgesia for most moderately painful procedures. The duration of action is dose dependent and can range from 2 to 10 hours, depending on amount used. Onset of effect ranges from 30 minutes following intravenous administration to 1 hour following intramuscular administration. Buprenorphine causes minimal sedation or other adverse effects associated with opioids, even when used at high dosages. Due to the lack of sedation and longer onset time, its use as a premedicant is limited.
Dosages
• Morphine: dog, 0.5 to 1.0 mg/kg IM, IV, or SC q 4 to 6 hr3,4; cat, 0.1 to 0.5 mg/kg IM or SC q 4 to 6 hr.
• Note: when administered intravenously, morphine must be given slowly to prevent histamine release.
• Oxymorphone: dog, 0.05 to 0.2 mg/kg IM, IV, or SC q 4 to 6 hr; cat, 0.05 to 0.1 mg/kg IM, IV, or SC q 4 to 6 hr.
• Meperidine: cat or dog, 2 to 5 mg/kg IM or SC4 q 2 to 3 hr. Do not administer intravenously due to significant histamine release.
• Fentanyl: 5 to 10 μg/kg IM or IV q 15 to 60 min or 0.3 to 0.7 μg/kg/min as a continuous-rate infusion.
Neuroleptanalgesia
Comments
• Combines a tranquilizer or sedative (i.e., neuroleptic) with an opioid (i.e., analgesia) as a preanesthetic medication.
Induction Drugs
Comments
• Adverse effects of these drugs are dosage dependent; therefore, techniques which minimize the induction dosage requirement are desirable.
Barbiturates
Thiopental sodium
• Available commercially in 1 g bottles to dilute to a final desired concentration. For example, to make a 5% solution, 20 ml of diluent is added to 1 g of sterile powder.
Dissociative Agents
Ketamine
• Often given intravenously with diazepam as an induction agent (5 mg/kg ketamine and 0.25 mg/kg diazepam) in dogs and cats.
Propofol
Advantages
• Can be given as repeated injections or continuous infusion due to minimal accumulation of the drug in the dog.
Disadvantages
• Causes profound and significant respiratory depression when given rapidly. Preoxygenation is strongly recommended.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree