Chapter 4 Amphibians
Case 4.1
Clinical examination
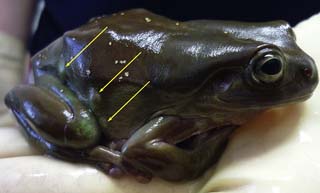
On presentation, the frog had a good nutritional status (bodyweight 38 g). The animal was calm but alert and responsive. The general health and the animal’s behaviour seemed to be unimpaired. The skin surface was smooth, moist and shiny. The mucous membrane in the mouth appeared pale pink-coloured and shiny. On the upper and lower surface of the right thigh were two 0.2 cm to 1.5 cm sized, whitish, round to oval, soft and elastic visible swellings. Similar distensions occurred on the frog’s right foot and on its right body wall (Fig. 4.1).
Faecal examination and ultrasonographic examination (Fig. 4.2) were performed, followed by incision of the distensions.
Diagnostic lancing and laboratory examination
Incision of distensions
One vesicle at the frog’s right foot and one on its abdominal wall were incised using a 23-G-needle. Several white objects were removed (Fig. 4.3) and microscopically evaluated.
A swab was taken out of one vesicle and subjected to a microbiological examination.
![]() 2. What is your interpretation of the removed structures (see Fig. 4.3)?
2. What is your interpretation of the removed structures (see Fig. 4.3)?
Results
 Ultrasonographic examination: in the subcutaneous, liquid-filled vesicles, several 0.2–0.4 cm sized hyperechogenic structures are visible
Ultrasonographic examination: in the subcutaneous, liquid-filled vesicles, several 0.2–0.4 cm sized hyperechogenic structures are visible
 Faecal examination using flotation and sedimentation techniques showed negative result for the presence of endoparasites
Faecal examination using flotation and sedimentation techniques showed negative result for the presence of endoparasites
 Microbiological examination revealed a medium amount of Enterobacter spp., Bacillus spp. and Staphylococcus spp.
Microbiological examination revealed a medium amount of Enterobacter spp., Bacillus spp. and Staphylococcus spp.
 In microscopic magnification (100×), the removed white structures showed peristaltic movement
In microscopic magnification (100×), the removed white structures showed peristaltic movement
Please evaluate the clinical history, Figs 4.1– 4.3, the results of the physical examination, diagnostic lancing and laboratory tests.
![]() 3. List your differential diagnoses.
3. List your differential diagnoses.
![]() 4. List your further diagnostic strategy.
4. List your further diagnostic strategy.
Differential diagnoses for subcutaneous swellings in frogs
 Subcutaneous larvae of cestodes or tapeworms, so called plerocercoids
Subcutaneous larvae of cestodes or tapeworms, so called plerocercoids
 Subcutaneous stages of nematodes, e.g. filariae
Subcutaneous stages of nematodes, e.g. filariae
 Subcutaneous larvae of acanthocephala or thorny-headed worms, so-called cystacantha
Subcutaneous larvae of acanthocephala or thorny-headed worms, so-called cystacantha
 Subutaneous larvae of trematoda or flukes, so-called metacercaria, e.g. Clinostomum
Subutaneous larvae of trematoda or flukes, so-called metacercaria, e.g. Clinostomum
 Chronic, progressive myositis caused by microsporidia, e.g. Pleistophora myotrophica
Chronic, progressive myositis caused by microsporidia, e.g. Pleistophora myotrophica
 Myositis caused by Ichthyophonus-like protozoa
Myositis caused by Ichthyophonus-like protozoa
 Cysts and dermal nodules caused by Amphibiocystidium (= Dermocystidium, Dermosporidium and Dermocystoides)
Cysts and dermal nodules caused by Amphibiocystidium (= Dermocystidium, Dermosporidium and Dermocystoides)
 Dermal or subcutaneous granulomas, often caused by mycobacteria (e.g. Mycobacterium xenopi, M. marinum, M. fortuitum) or fungi like Saprolegnia (e.g. S. parasitica), Basidobolus (e.g. B. ranarum), Mucor (e.g. M. amphibiorum) or Cladiosporum
Dermal or subcutaneous granulomas, often caused by mycobacteria (e.g. Mycobacterium xenopi, M. marinum, M. fortuitum) or fungi like Saprolegnia (e.g. S. parasitica), Basidobolus (e.g. B. ranarum), Mucor (e.g. M. amphibiorum) or Cladiosporum
 Neoplasias, spontaneous or caused by viral agents like herpesviruses, e.g. Lucké tumour virus (LTHV or RaHV-1)
Neoplasias, spontaneous or caused by viral agents like herpesviruses, e.g. Lucké tumour virus (LTHV or RaHV-1)
 Oedemas or dermal ulcers caused by ranaviruses from the family Iridoviridae
Oedemas or dermal ulcers caused by ranaviruses from the family Iridoviridae
Further diagnostics
 Because of the morphology and the peristaltic movements, the structures were suspected to be of parasitic origin. To determine the family and/or genus of a parasitic structure, the removed structures were fixed in alcohol and submitted to specialized institutions (Fischer et al. 2010) for parasitology. A morphological, histological and molecular biological examination was performed
Because of the morphology and the peristaltic movements, the structures were suspected to be of parasitic origin. To determine the family and/or genus of a parasitic structure, the removed structures were fixed in alcohol and submitted to specialized institutions (Fischer et al. 2010) for parasitology. A morphological, histological and molecular biological examination was performed
 Morphological and histological examinations revealed the structures as plerocercoids of pseudophyllid cestodes, termed spargana
Morphological and histological examinations revealed the structures as plerocercoids of pseudophyllid cestodes, termed spargana
 Molecular biological examination identified the parasite species as Spirometra erinaceieuropaei
Molecular biological examination identified the parasite species as Spirometra erinaceieuropaei
Therapy (Table 4.1)
| Praziquantel | 15 mg/kg SC twice, every second week |
| Isoflurane | 0.015 ml/g liquid isoflurane topically on the skin – to maintain anaesthesia during the surgery |
| Incision of the vesicles using a 23 G needle | In total about 50 0.1–0.8 cm sized, irregularly shaped, white, partly transparent and tough objects were removed from the vesicles. Some objects were up to 3 cm long |
| Quarantine | During the medication on wet towels |
| Disinfection of the aquaterrarium | Neopredisan® 135-1 (Menno GmbH, Norderstedt, Germany) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree