6 THE HINDLIMB
Clinical importance of the hindlimb
Osteoarthritis of the small hock joints does occur. ‘Bog spavin’ is a descriptive term for synovial effusion of the tarso-crural joint. It is the result of a low-grade synovitis. The swelling appears in the proximo-medial part of the hock. It is not a major cause of persistent hindlimb lameness in the horse. Osteochondrosis dissecans, a degenerative condition of cartilage, also affects the hock, particularly the distal intermediate ridge of the tibia and the lateral trochlear ridges of the tibio-tarsal joint. The hock joint can also suffer from bacterial infection and inflammation, similar to gonitis of the stifle joint. This often results in extensive necrosis and ultimately joint collapse. Another important condition of the hock is fluid distension of the tarso-crural joint which occurs dorso-medially between the fibularis (peroneus) tertius muscle and the medial malleolus; dorso-medially between the medial malleolus and the deep digital flexor tendon; and caudo-laterally between the lateral malleolus and the tuber calcis. Tarso-crural dislocation (luxation) is a rare event which is virtually impossible to repair and is an indication for immediate euthanasia.
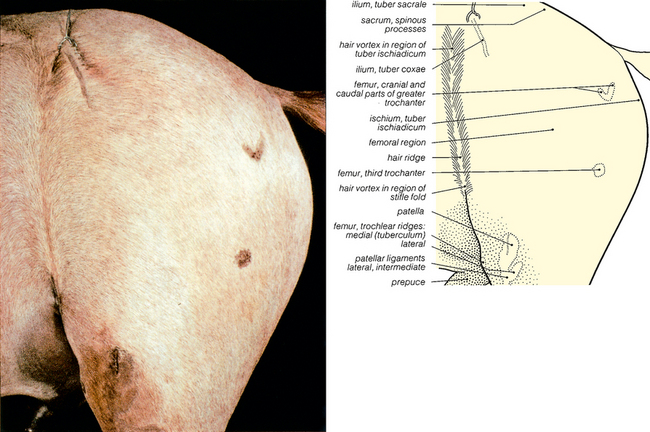
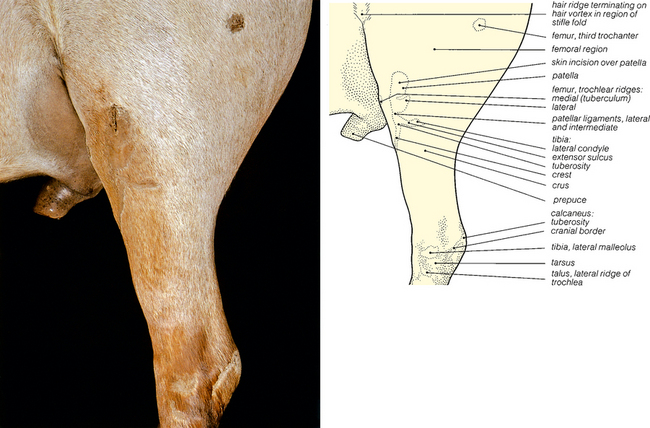
Fig. 6.1 Surface features of the pelvic and femoral regions of the gelding: left lateral view. The palpable features have been shaved. An incision marks the point where the patella was nailed to the femoral trochlea, in order to fix the stifle joint. The intermuscular septum between the biceps femoris and semitendinosus muscles (the so-called ‘poverty line’) is rarely visible after embalming (see Fig. 6.9).

Fig. 6.2 Bones of the pelvic and femoral regions: left lateral view. The palpable bony features shown in Fig. 6.1 have been coloured red, except the tuber sacrale and the sacral spines. In this skeleton the patella has not been positioned so distally in the trochlea: in the embalmed horse the hindlimb was fully extended before nailing the patella to the trochlea.
< div class='tao-gold-member'>