3 THE FORELIMB
Clinical importance of the forelimb
Equine limbs are often subjected to trauma, especially the forelimbs.
Carpal joint disease is quite common. There are 7 or 8 bones in the carpus. The proximal carpal row has radial, intermediate, ulnar and accessory carpal bones. The distal row has carpal bones II, III, IV and sometimes carpal bone I. There are approximately 26–27 separate articulations between these bones. There are essentially three joints – the antebrachio-carpal, which both rotates and glides; the middle carpal joint which is a simple hinge joint and the carpo-metacarpal articulation which has very little movement.
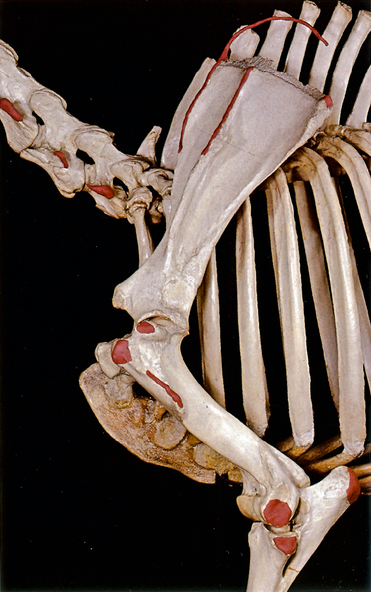
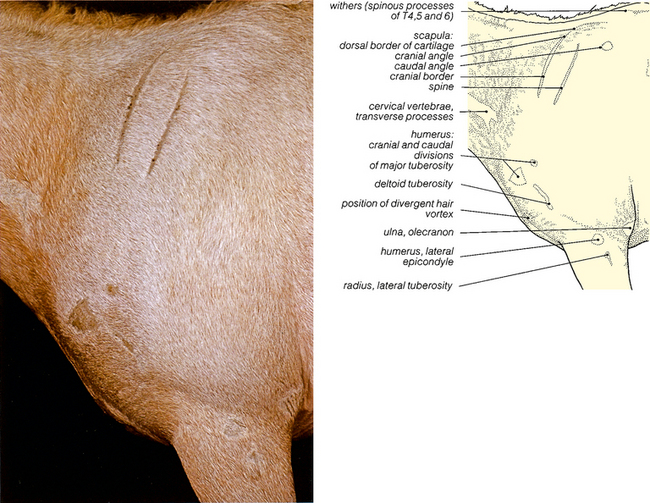
Fig. 3.2 The bones of the forelimb. Scapular and brachial regions: left lateral view. The palpable bony prominences shown in Fig. 3.1 have been coloured red. The palpable edge of the scapular cartilage is shown by a red wire. The tips of the spinous processes at the withers have not been coloured.
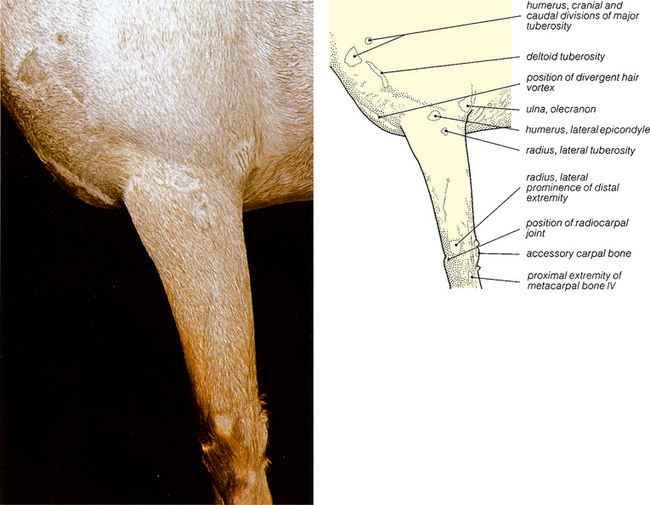
Fig. 3.3 Surface features of the brachial, antebrachial and carpal regions: left lateral view. The palpable bony prominences have been shaved. The surface features of the manus and the location of the carpal pad (chestnut) on the medial side of the limb in the distal antebrachium, are shown in Figs. 7.1, 7.3, 7.5 and 7.7. The lateral prominence on the distal extremity of the radius is often called the lateral styloid process, but it is partly metaphyseal.