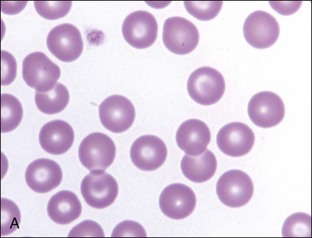
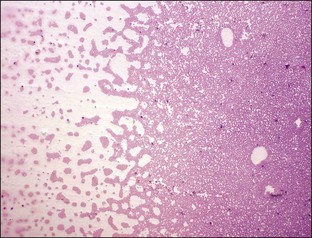
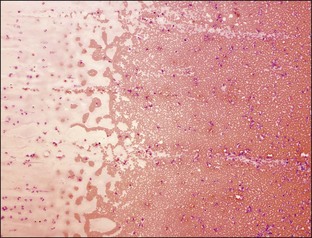
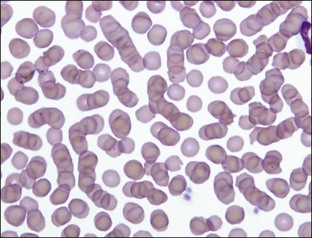
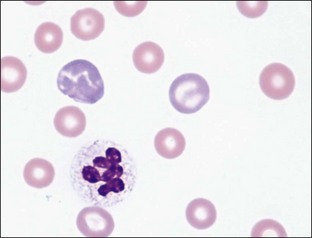
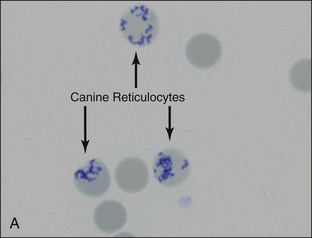
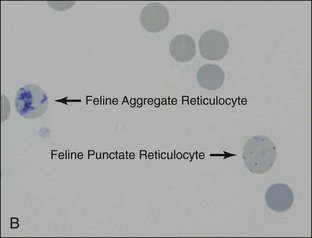
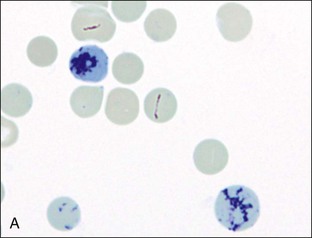
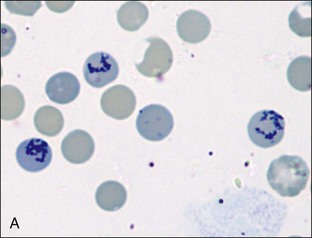
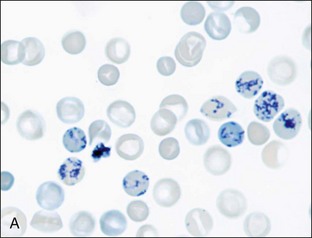
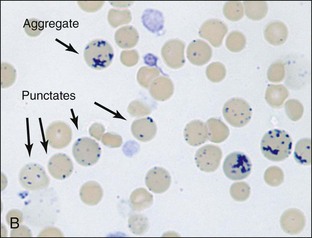
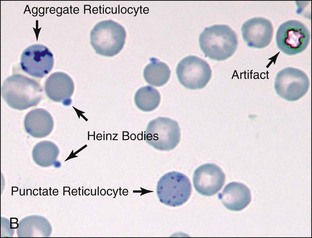
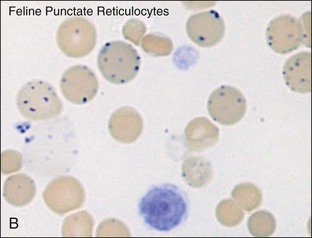
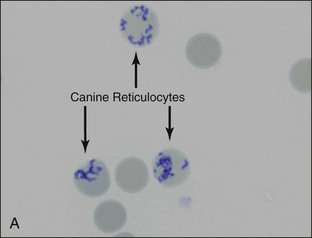
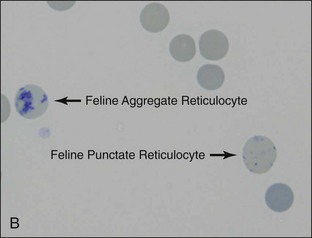
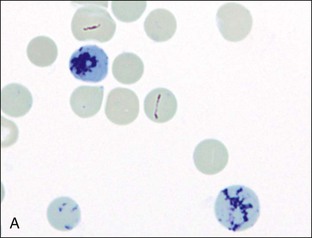
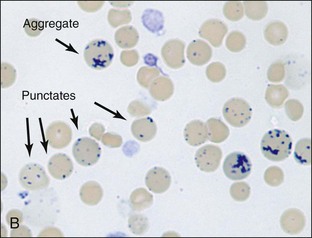
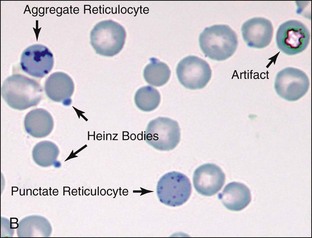
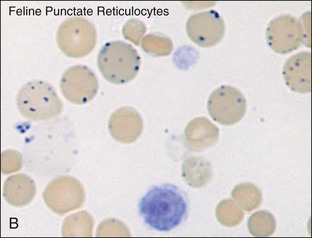
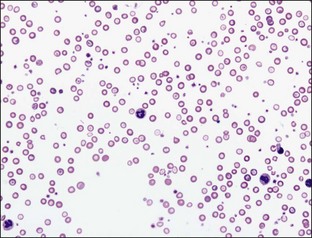
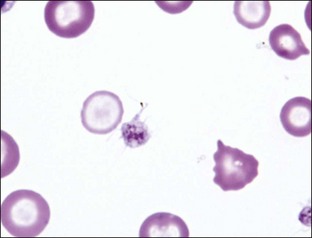
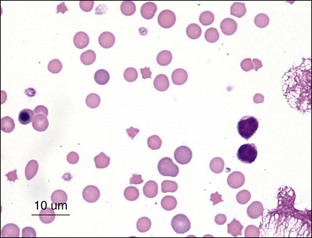
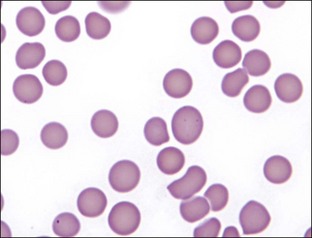
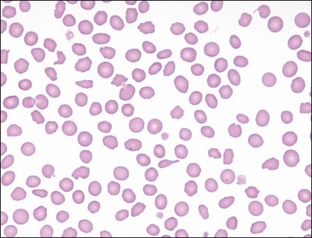
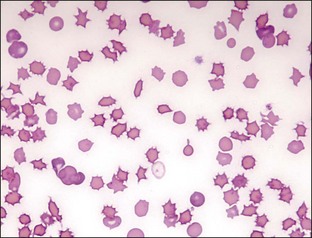
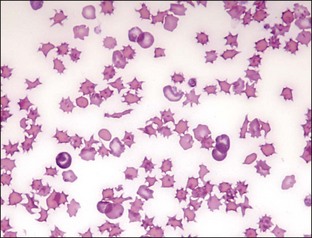
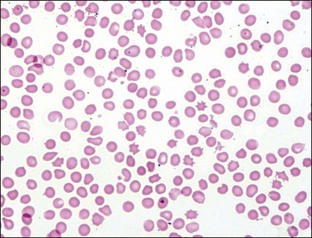
Section 2 Normal Morphology (Discocytes and Normocytes) Morphologic Changes Associated with Disease Leptocytes: Target Cells (Codocytes) and Folded Red Blood Cells Schistocytes (Fragmented Erythrocytes) Keratocytes (Blister Cells and Helmet Cells) Echinocytes (Crenated Cells, Burr Cells, Berry Cells) Erythrocytic Ghosts (Lysed Red Blood Cells, Fading Erythrocytes) Nucleated Red Blood Cells (Metarubricytes and Rubricytes) Siderotic Inclusions (Pappenheimer Bodies) Mycoplasma hemocanis (previously Hemobartonella canis) Mycoplasma hemofelis (previously Hemobartonella felis) Careful attention should be made to not confuse rouleaux with RBC agglutination. Rouleaux are orderly linear stacks of RBCs, whereas RBC agglutination is formed by grapelike RBC aggregates. To aid in differentiating between rouleaux and agglutination, a saline dilution test is useful. Rouleaux may be easily dissociated by dilution of RBCs in saline, whereas true agglutination persists despite saline dilution (for method, see Appendix). If rouleaux is confirmed, determine plasma or serum total protein, albumin, globulin, fibrinogen values and lipemic index, and investigate potential causes of any abnormalities found. The clinical usefulness of punctate reticulocyte counts in cats remains unclear. Many laboratories and all hematology instruments that report reticulocyte counts in cats, count and report only aggregate reticulocytes. Manual reticulocyte counts are done by counting the number of reticulocytes present in 1000 RBCs. The percentage is determined by dividing the number of reticulocytes counted by 10. The absolute reticulocyte count is determined by multiplying the reticulocyte % by the RBC count. The degree of reticulocytosis is best indicated by the absolute aggregate reticulocyte count (see the Appendix for more information).
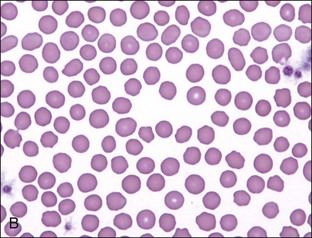
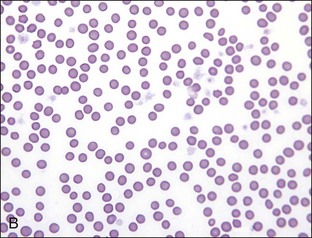
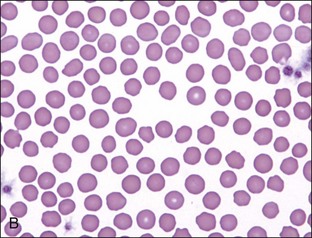
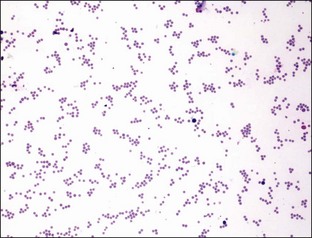
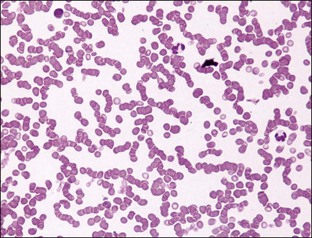
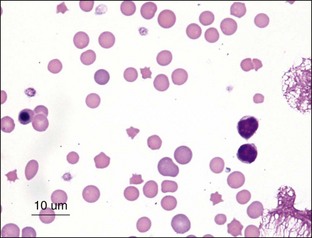
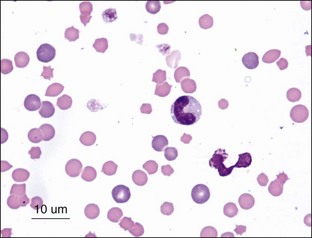
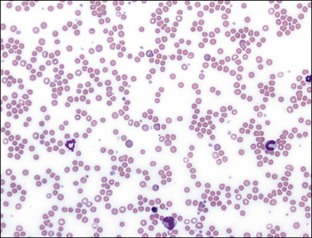
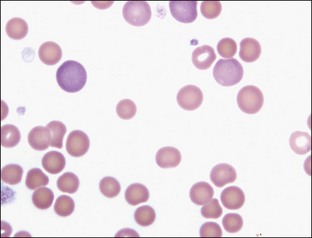
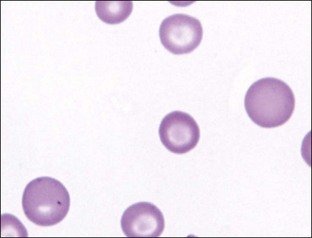
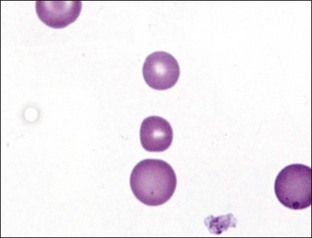
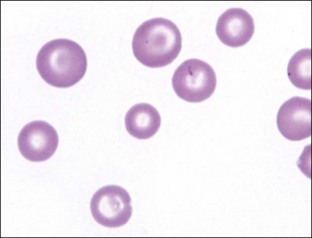
Red Blood Cells
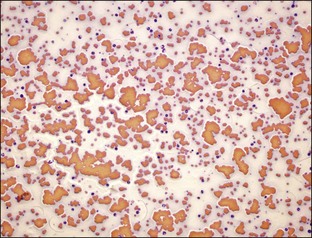
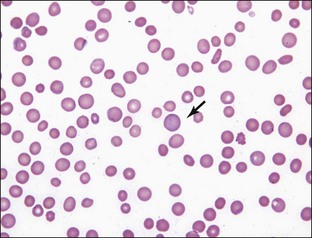
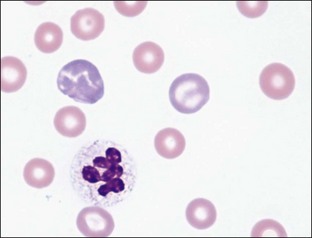
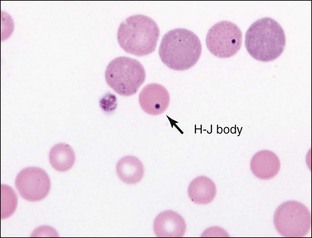
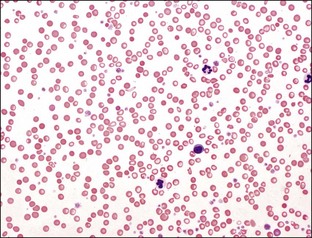
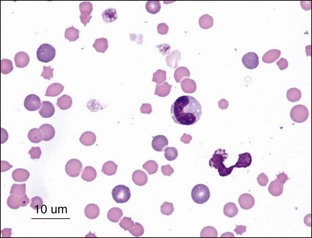
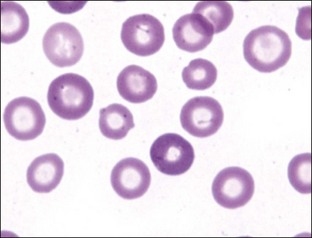
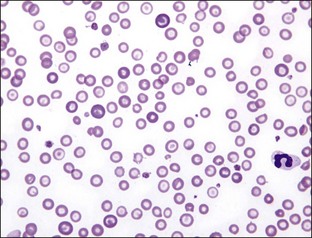
Morphologic Changes Associated with Disease
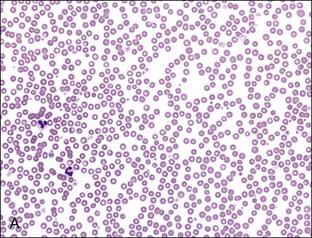
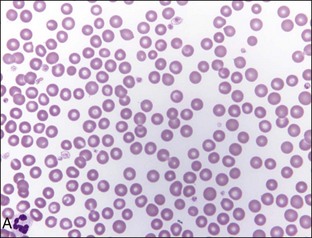
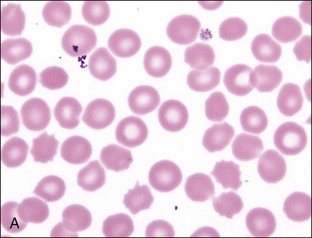
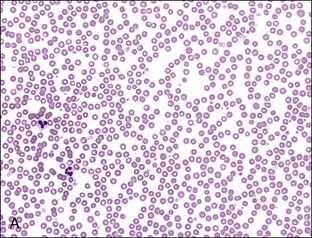
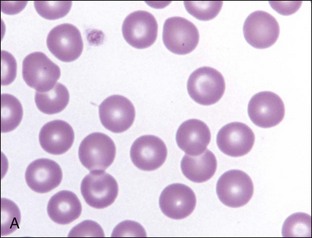
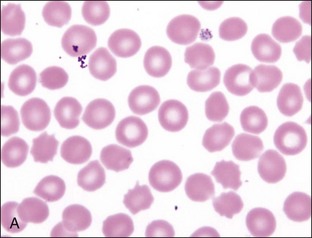
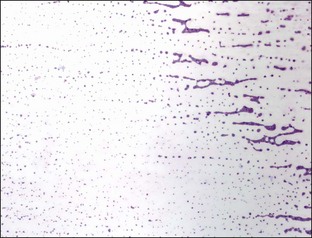
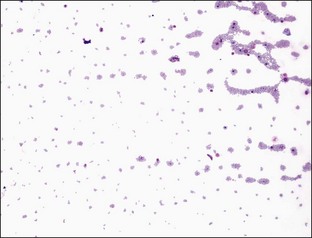
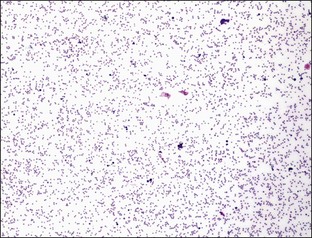
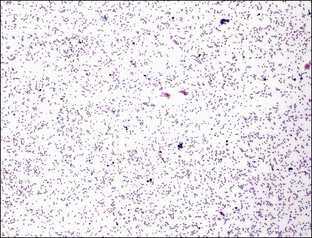
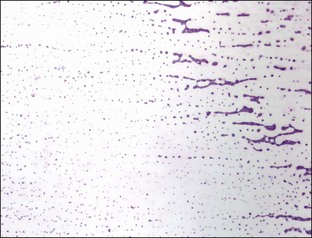
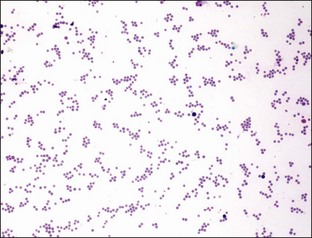
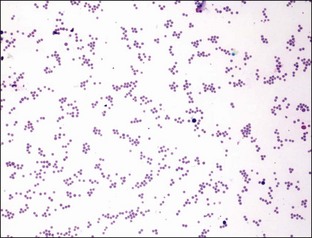
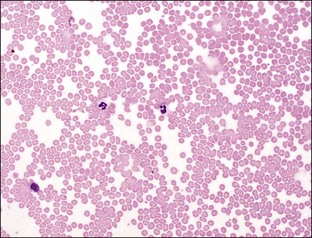
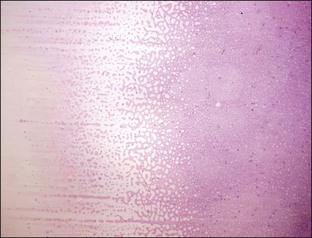
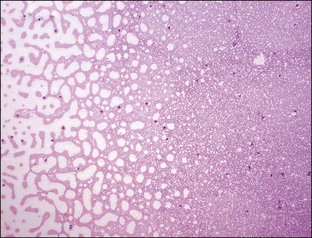
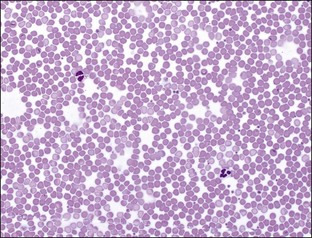
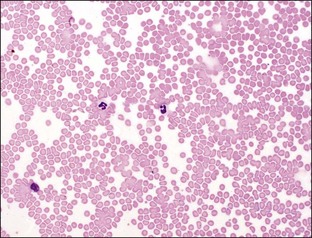
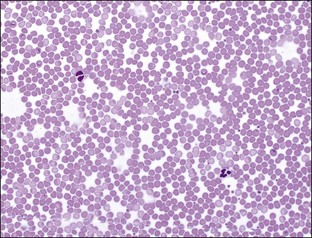
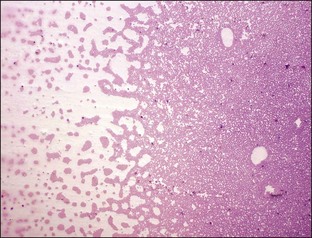
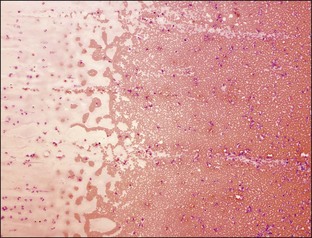
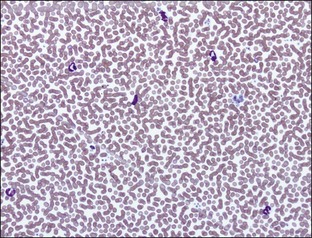
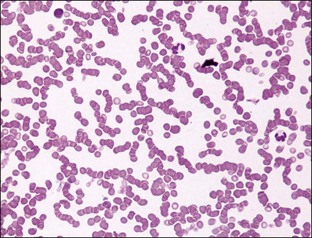
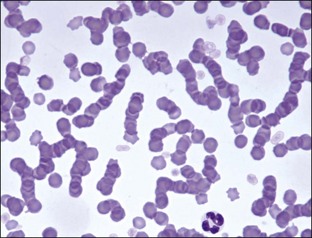
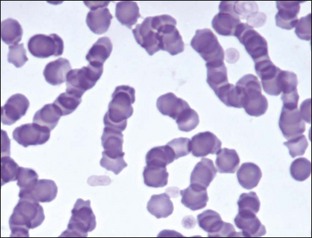
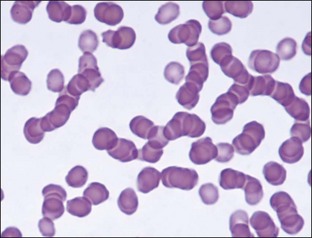
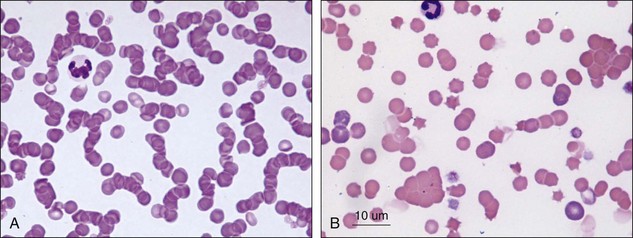
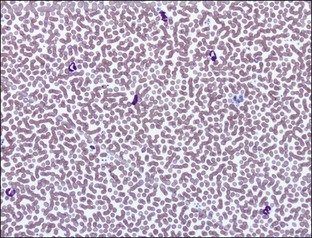
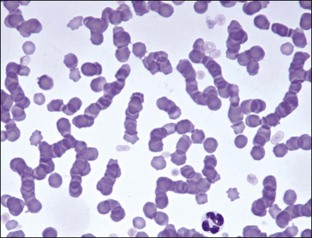
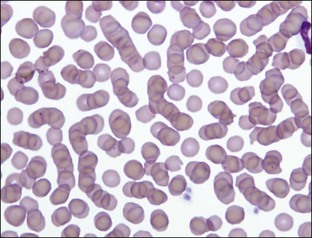
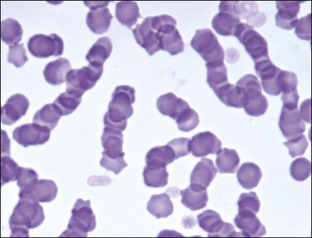
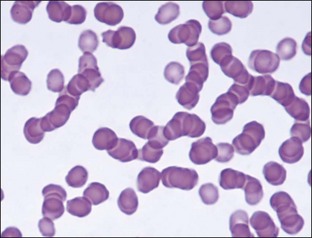
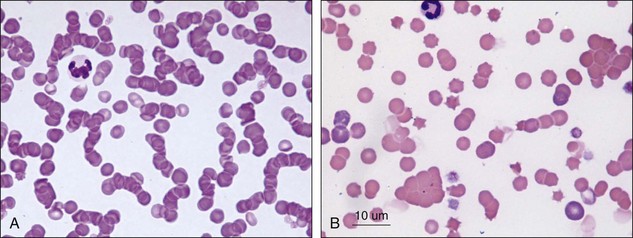
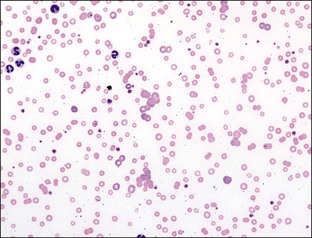
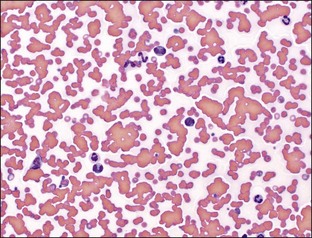
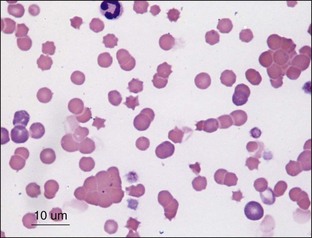
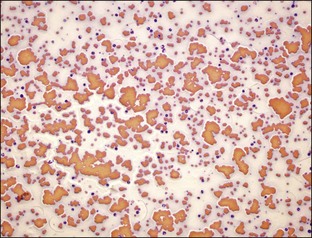
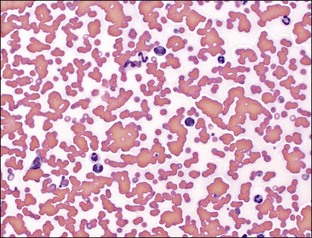
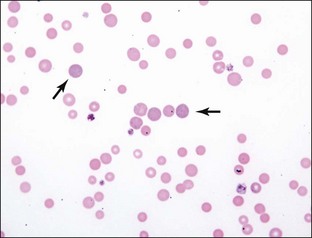
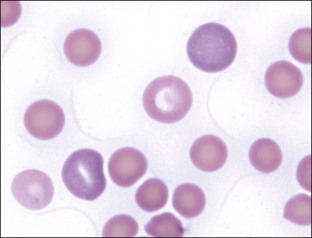
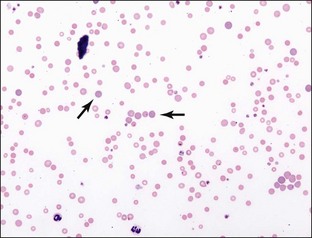
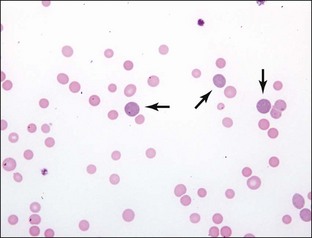
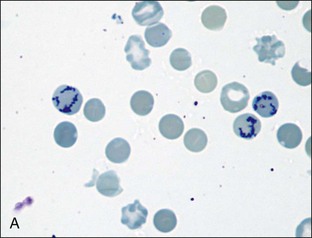
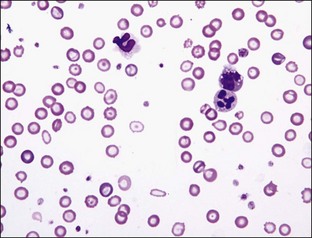
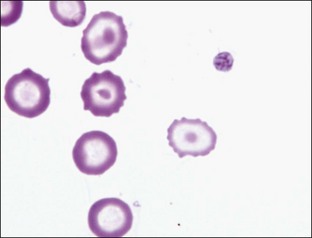
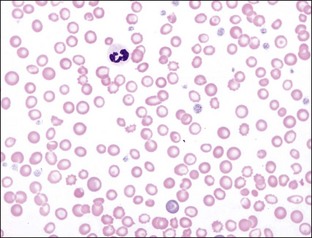
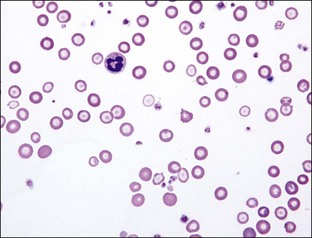
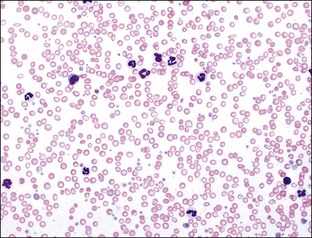
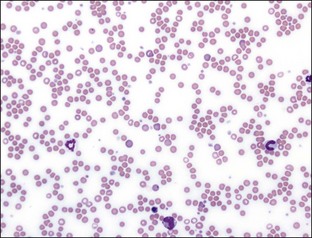
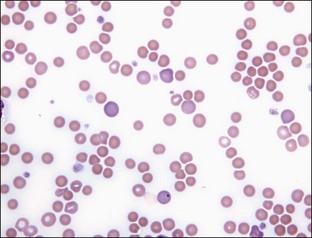
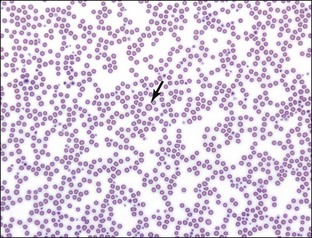
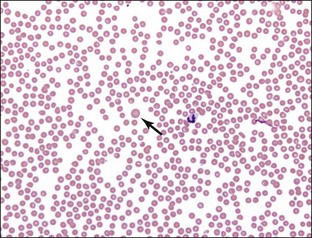
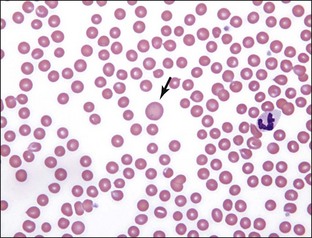
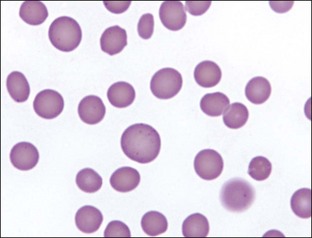
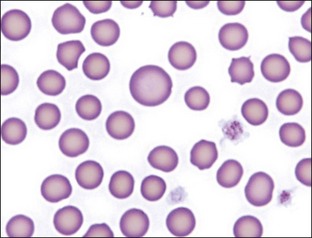
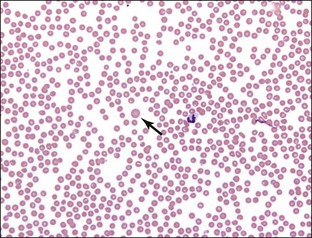
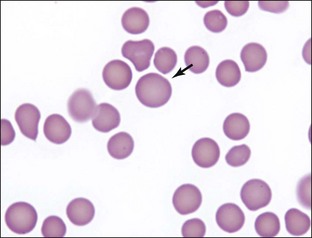
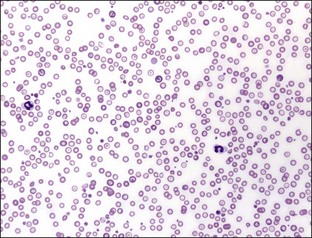
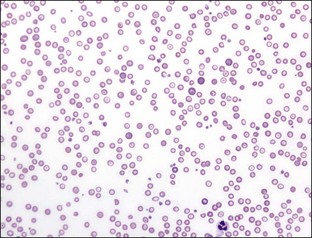
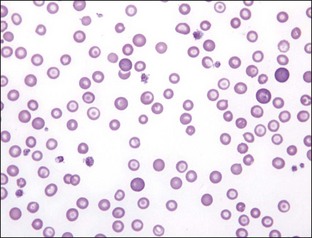
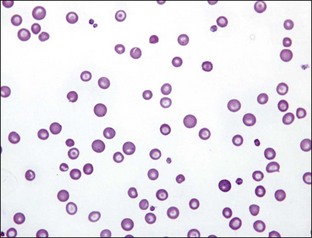
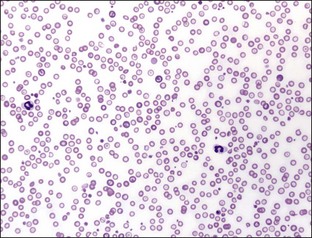
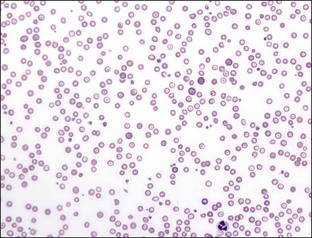
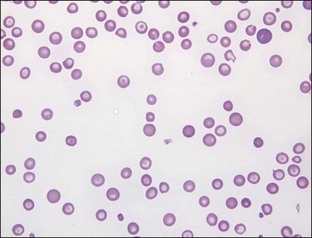
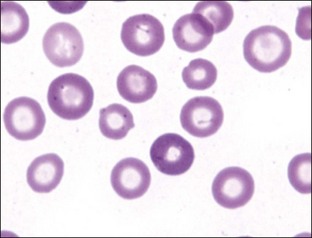
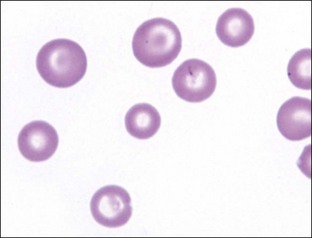
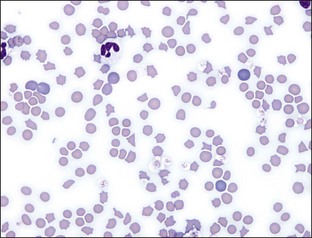
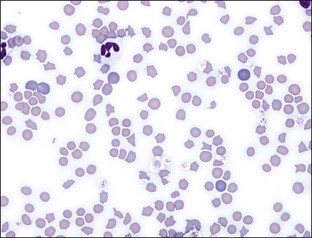
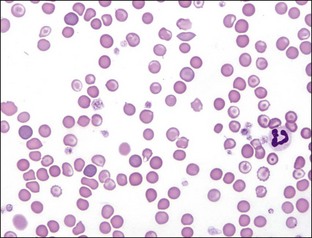
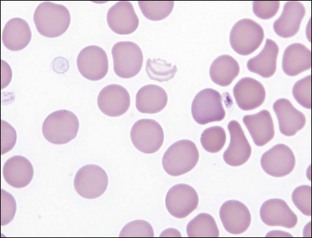
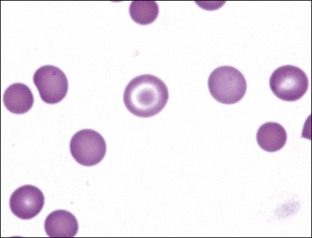
Rouleaux
Diagnostic Significance:
Next Steps:
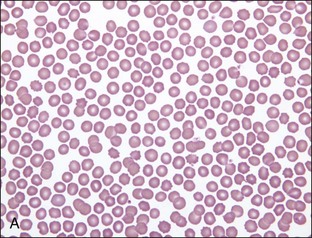
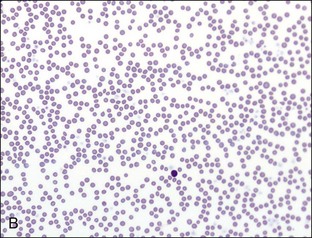
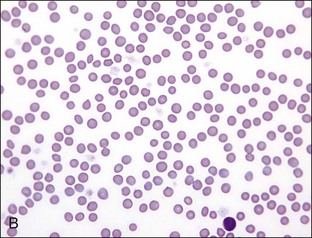
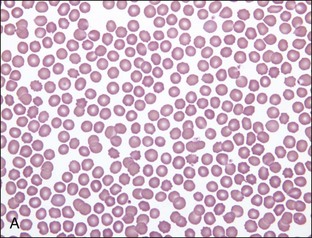
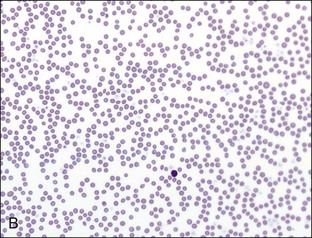
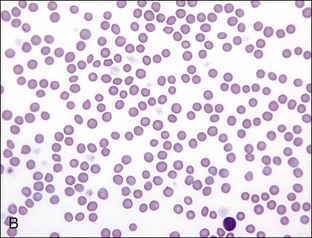
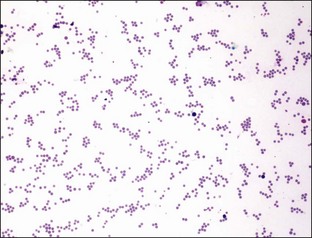
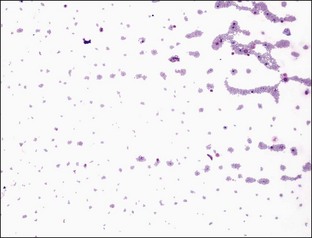
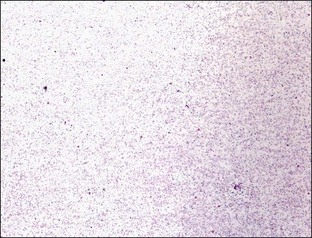
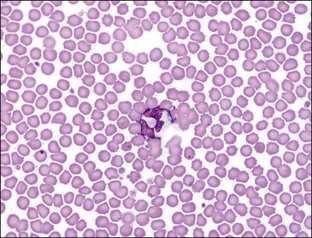
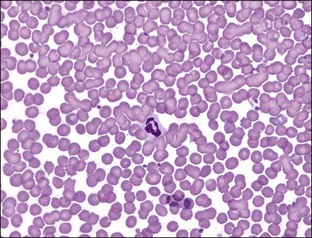
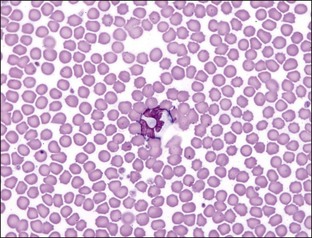
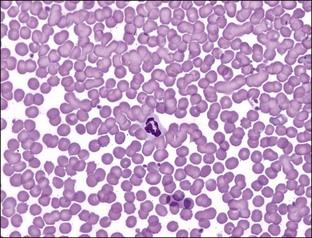
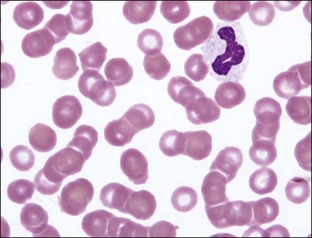
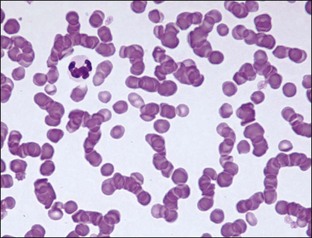
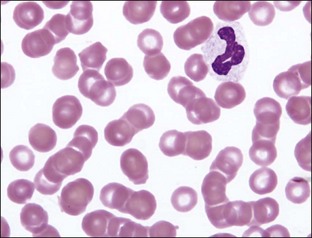
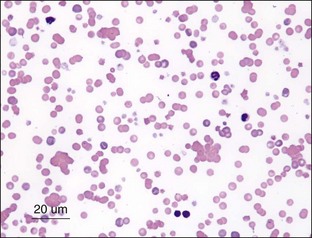
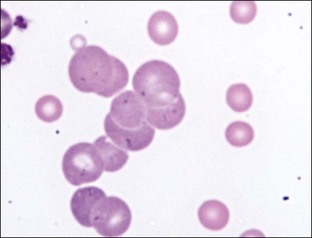
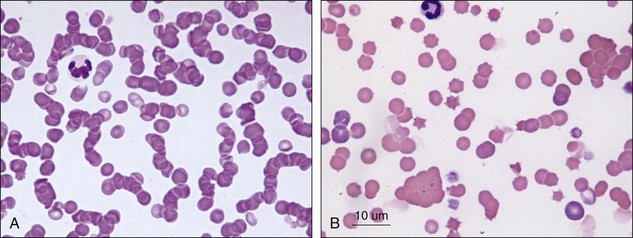
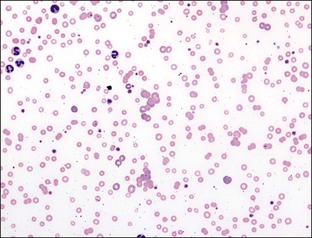
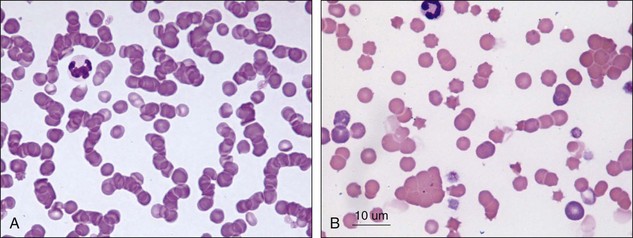
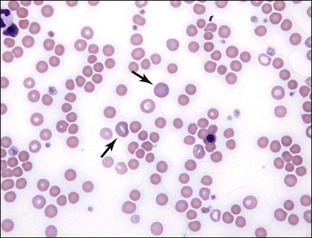
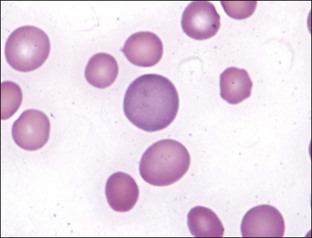
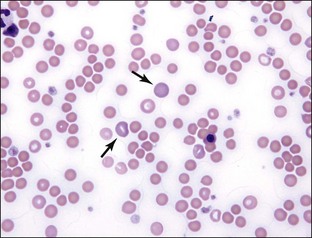
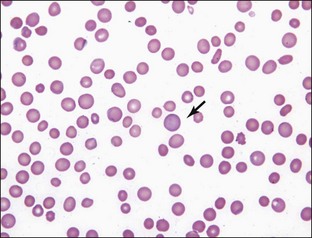
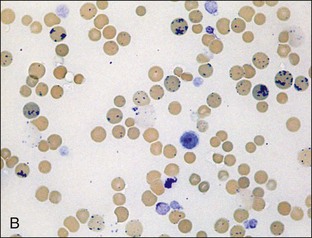
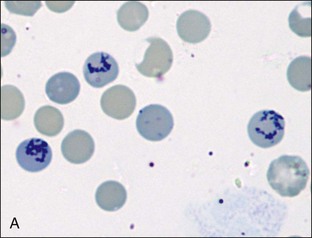
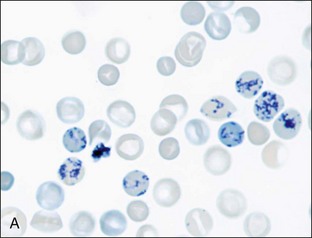
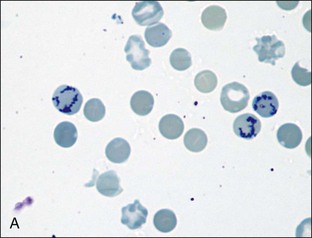
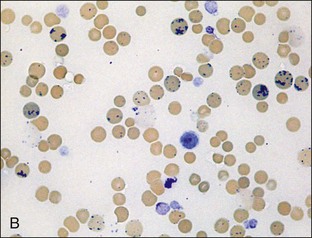
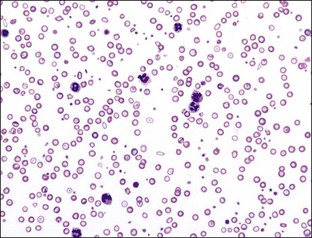
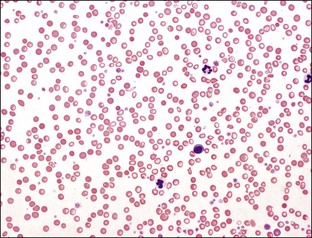
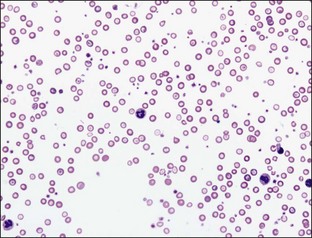
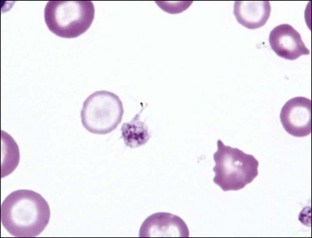
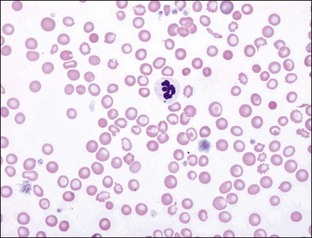
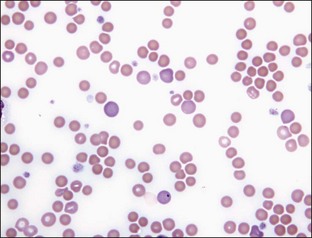
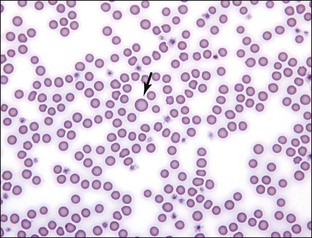
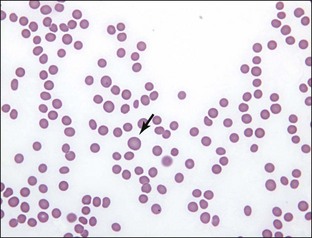
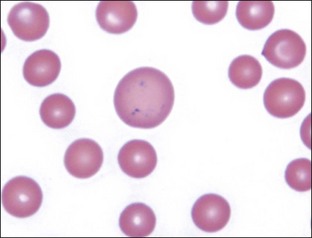
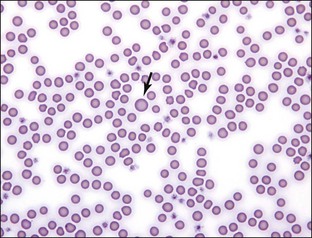
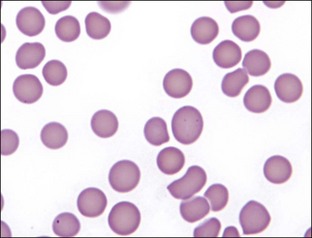
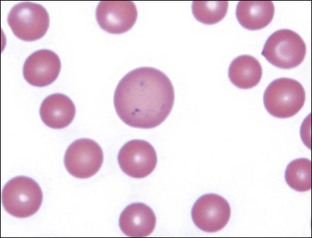
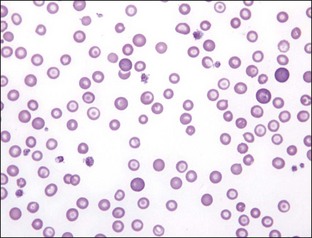
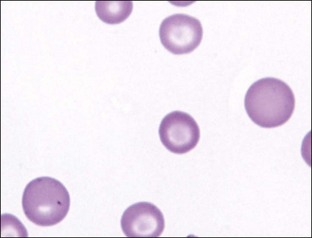
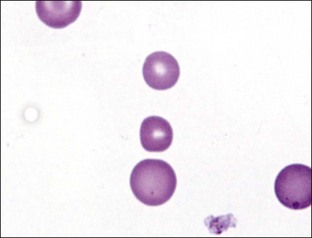
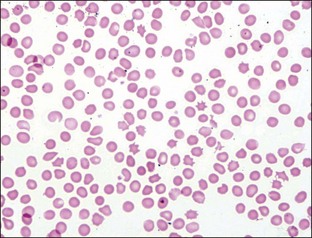
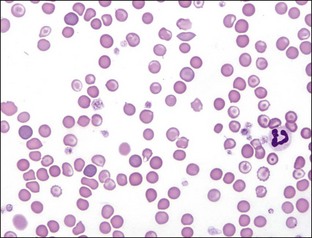
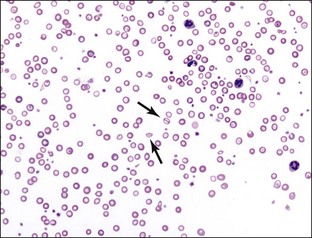
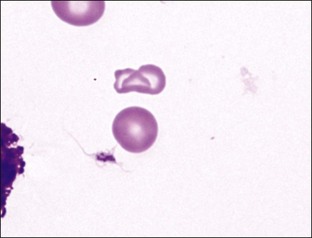
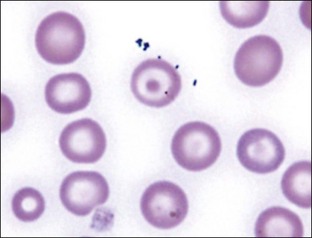
Reticulocytes
Distinctive Features:
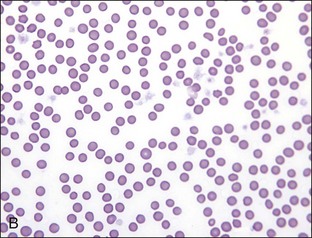
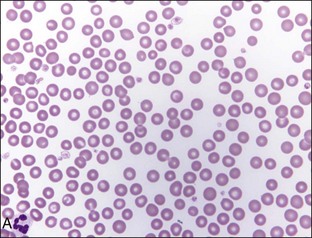
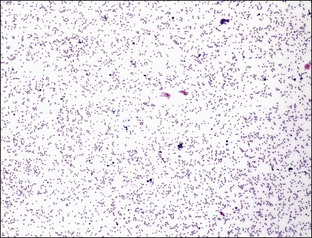
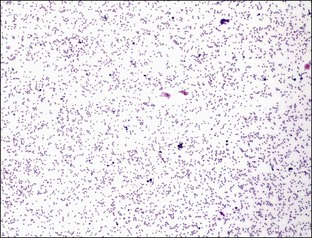
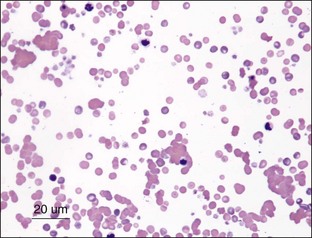
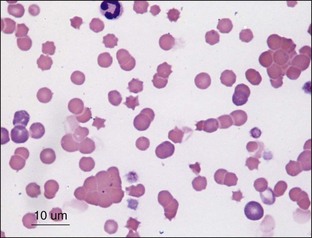
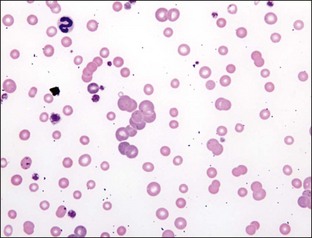
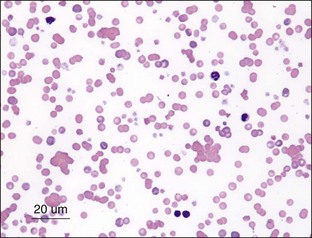
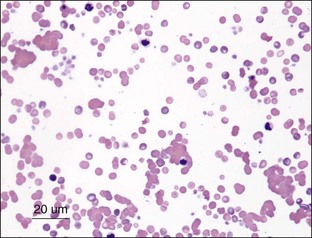
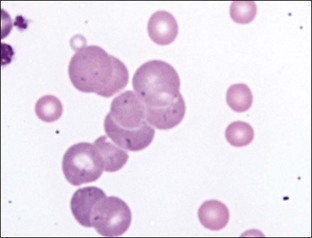
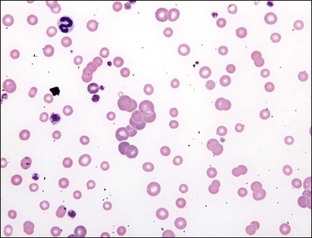
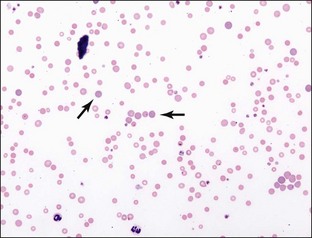
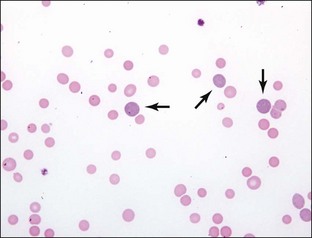
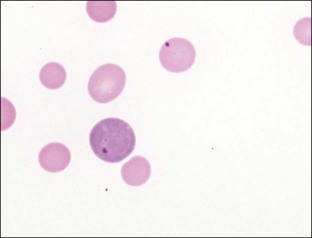
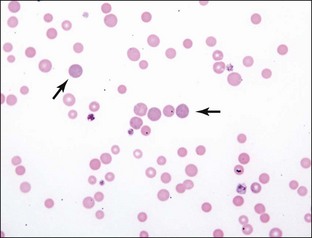
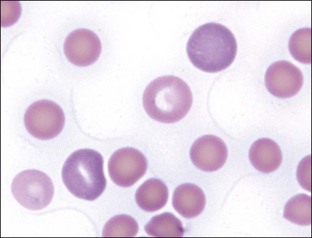
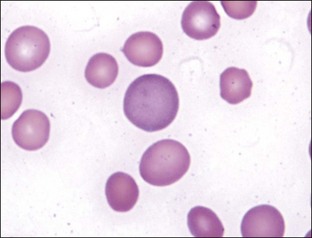
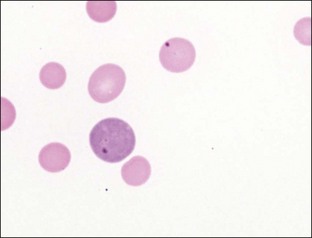
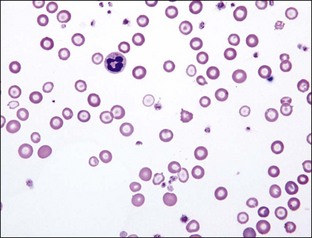
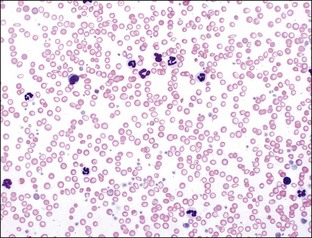
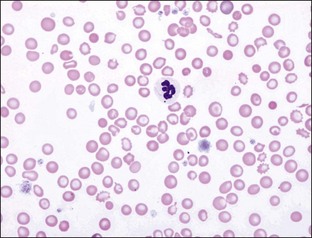
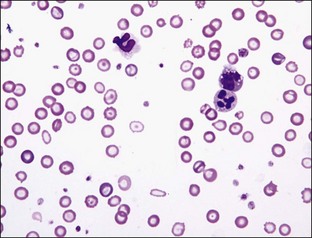
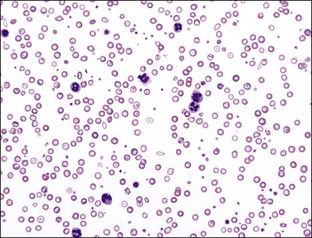
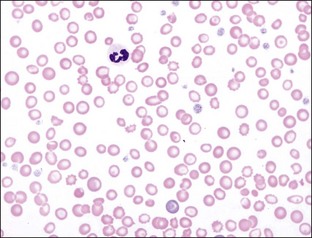
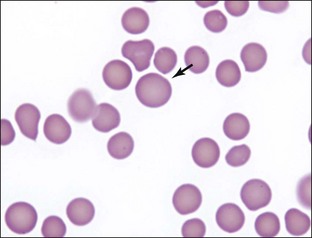
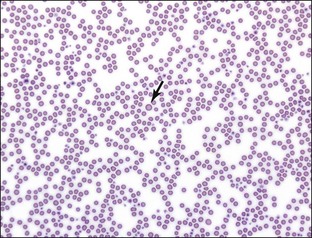
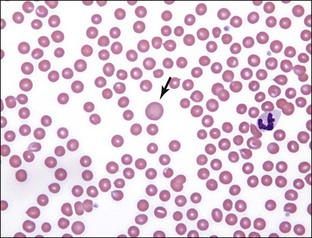
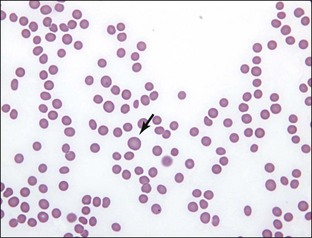
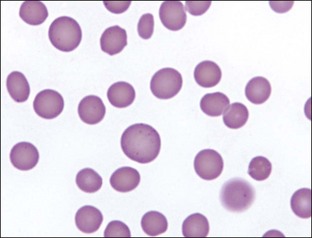
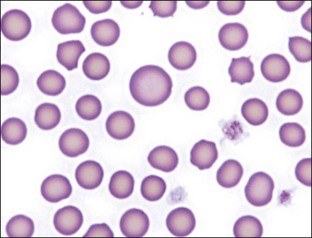
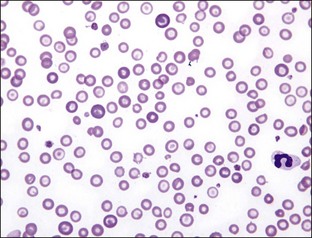
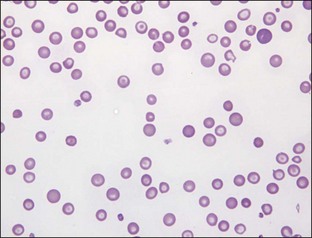
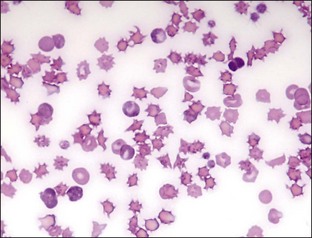
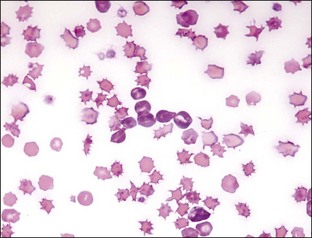
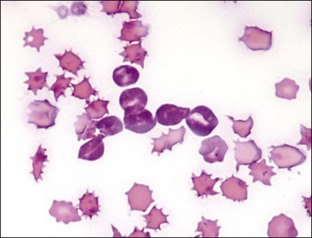
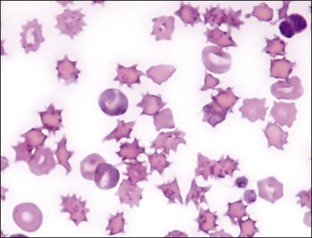
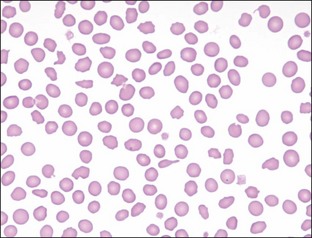
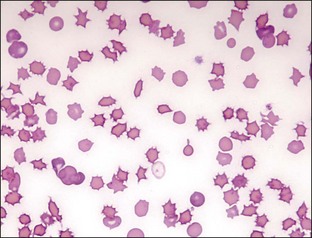
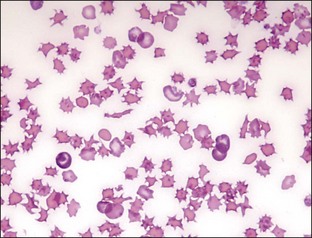
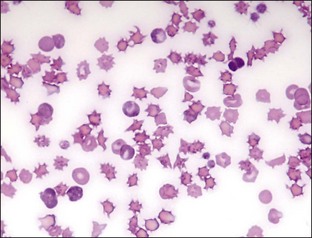
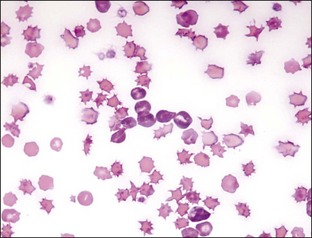
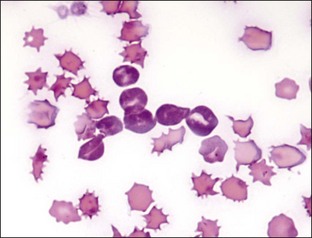
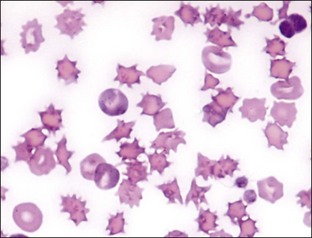
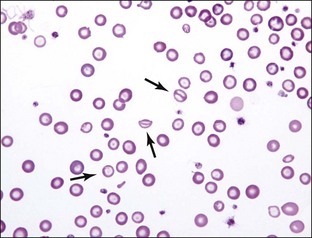
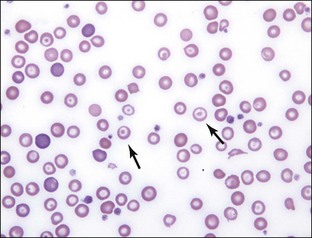
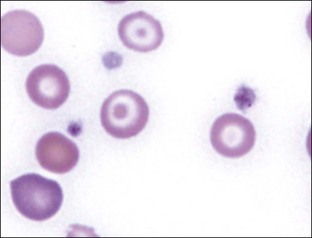
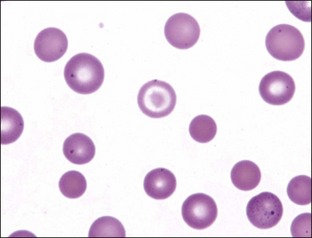
Poikilocytes
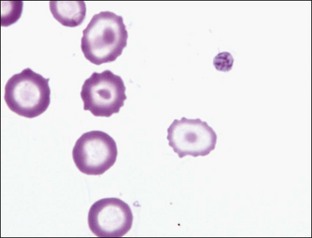
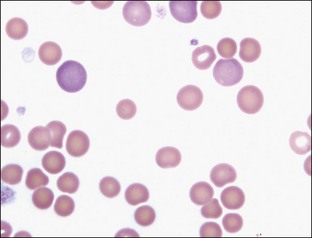
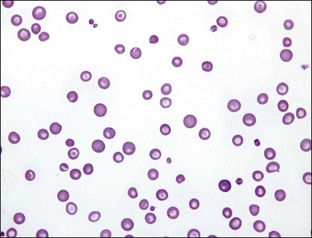
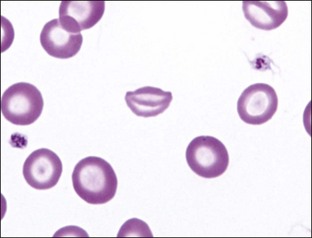
Leptocytes: Target Cells (Codocytes) and Folded Red Blood Cells