The aim of physical rehabilitation is to reestablish normal function using modalities such as heat and electrical stimulation, mobilization, and therapeutic exercise.1 Superficial heating agents penetrate soft tissues to a depth of approximately 1 cm. Deep heating agents can elevate tissue temperatures at depths of 2 cm or more. Deep heating agents commonly used include therapeutic ultrasound (US) and diathermy. Although diathermy is an effective deep heating modality, it requires the patient to remain stationary for 15 to 20 minutes and is not practical in dogs. Therapeutic US is considered an effective treatment modality for rehabilitating musculoskeletal conditions such as restricted range of motion (ROM) resulting from joint contracture, pain and muscle spasm, and wound healing.2 There are advantages and disadvantages of US therapy (Box 19-1). Many protocols for the administration of US are based on tradition or extrapolated from basic science research and remain to be tested in controlled clinical trials.3–6 This chapter is based on a review of current literature pertaining to the basic research findings (in human and dogs) and the clinical application of US therapy in dogs. Energy within a sound beam decreases as it travels through tissue, because of scatter and absorption. Scattering is the deflection of sound out of the beam when it strikes a reflecting surface. Absorption is the transfer of energy from the sound beam to the tissues. Absorption is high in tissues with high protein content7,8 and relatively low in adipose tissue.7,9 For more detailed information regarding the components of US machines, piezoelectric effects, sound generation, and sound propagation through tissues, the reader is referred to other sources.10,11 The US beam is attenuated in air and reflected at air-tissue interfaces. Consequently a coupling medium must be placed between the sound head and the skin.12 Methods for direct coupling, immersion, and use of coupling cushions have been described for dogs.13 Commercially prepared water-soluble US gels are the best and most practical coupling method. The gel may be preheated. Coupling agents that are not recommended include1 substances that may irritate or penetrate through the skin2; electroconductive gels, such as for electrocardiography or electromyography, which contain salts that can damage the transducer face3; lanolin-based compounds, which would cause heating of the transducer head with poor transmission to tissue8; and mineral oil,4 which is messy to remove.13 Over-the-counter creams and lotions should not be used because they generally do not provide effective transmission of US. Other methods of coupling have been used. However, research results on these indirect coupling methods are inconclusive, and further investigation is warranted.14 The underwater method was popular before smaller transducer heads became available.8 Immersion should be considered only when the surface to be treated is so uneven that direct contact is too difficult. The part of the body to be treated, usually a distal limb, can be immersed in a container of tap water at room temperature. The water and the animal’s skin must be clean.15 Water in a whirlpool is not recommended if it has been agitated because air bubbles form in the water. Deionized, degassed water is not necessary, but the water may be boiled and cooled or allowed to stand to remove air bubbles. Even so, small air bubbles tend to accumulate on the transducer face and the skin during treatment. The therapist can wipe these off quickly, but should try to minimize his or her own exposure. With regard to container type, metal containers reflect some of the US beam, which could increase the intensity in areas near the metal; rubber or plastic do not cause as much reflection. During treatment, the transducer should be held underwater 0.5 to 3.0 cm from the skin surface. The intensity may be increased by 0.5 W/cm2 to compensate for absorption by water.7 Immersion has not compared favorably with direct coupling in several studies that examined the tissue temperatures achieved with these two methods. One study compared immersion to topical US gel on temperature rise at a depth of 3 cm in the gastrocnemius muscle of humans.12 The treatment consisted of continuous US at 1.5 W/cm2 for 10 minutes, with the sound head moved at a speed of 4 cm per second. With direct coupling, tissue temperature increased 4.8° C compared with 2.1° C with immersion. In another study the lateral epicondyle of pigs was treated with the transducer in direct contact with the skin and with the limb immersed in a water bath with the applicator held 2 cm from the skin surface. The temperature in the tendons of the extensor muscles originating at the lateral epicondyle rose into the therapeutic range (an increase of 2° or more) with direct coupling, but not with immersion.16 Another alternative to direct coupling is the use of a coupling cushion.13 Placing a water-filled balloon between the transducer head and the skin, with coupling gel at the interfaces, has been described.10 A recent in vitro study compared the transmission properties of commercial gel pads, bladder techniques, and water bath immersion, through pig skin from which the hair had been clipped.14 Insufficient acoustic energy transmission occurred with degassed tap water in latex gloves, gel in a latex glove, degassed tap water baths, and gel-filled condoms. The authors recommended that if the direct method cannot be used because of the contour of the surface to be treated, clinicians should consider the use of commercially available gel pads. If other direct techniques are used, transmission is considerably less than with the direct coupling technique or commercial gel pads.14 The hair coat of dogs treated with US presents a problem not encountered with human patients. Because US energy is absorbed by tissues with high protein content, and deflection of the US beam occurs at tissue interfaces, it would be expected that US penetration through the hair coat into underlying tissues would be poor. For horses, one author has specifically recommended clipping the hair and using adequate coupling gel or having the horse stand in water to reduce any air interphase.17 A study was conducted in dogs to determine temperatures in underlying tissues when delivering US through intact hair coats.18 Despite application of a thick layer of gel on the skin, US delivered through short or long hair coats produced only minimal temperature increases in the underlying tissues, compared with therapy after the hair had been clipped, although there was considerable warming within the hair coat and on the skin (Figure 19-1). Sound waves above a frequency of 20,000 hertz (20 kHz) exceed the upper range of human hearing and are termed US. The higher the frequency, the less divergent the sound beam. Ultrasound beams are considered to be collimated, and frequencies in the megahertz (MHz) range expose a limited target area. Frequency, not intensity, determines depth of penetration. The frequency most often used is 1 MHz because it represents a compromise between deep penetration and adequate heating. A frequency of 1 MHz frequency heats at depths between 2 and 5 cm.19 As the frequency increases, penetration decreases. A frequency of 3.3 MHz (commonly referred to as 3 MHz) heats at depths between 0.5 and 3 cm.8,19,20 Therefore for superficial lesions, a frequency of 3 MHz is preferred; for deeper lesions, a setting of 1 MHz is needed.8 If there is underlying bone, most of the US transmitted to that depth will be absorbed by the bone and may cause periosteal pain.19–21 The intensity should not be turned up very high to heat the underlying soft tissue if the bone is not adequately covered by soft tissues.19 Low frequency or “long wave” US machines have also been investigated.22 These units emit US at a lower frequency, around 45 kHz. In an in vitro study using fibroblasts, osteoblasts, and monocytes, both 45 kHz and 1 MHz exposure enhanced cell proliferation, protein synthesis, and cytokine production.22 The higher the intensity, the greater and faster the temperature increases. The depth of tissue penetration is not affected to a large degree. Generally intensities required to increase tissue temperature 2° C or more vary from 1 to 2 W/cm2 continuous wave US for 5 to 10 minutes. To heat an area with substantial soft tissue, intensities as high as 2 W/cm2 may be used. If there is less soft tissue, or if bone is close to the skin surface, lower intensity and higher frequency are appropriate. After selection of an initial intensity, the patient’s tolerance to the heat produced by the US is the final determinant of intensity.7 This may be difficult to determine in pets. Many dogs lie quietly during US treatment. However, dogs sometimes begin to whine or otherwise seem uncomfortable within 5 to 10 minutes after commencing US. It should be assumed that any distress demonstrated by a patient may indicate pain, and the intensity of the US should be reduced or the session interrupted or discontinued. Most therapists tend to use intensities that produce no detectable sensation in human patients. However, some clinicians advise that the intensity be increased until the person feels vigorous heating, after which time the intensity should be decreased if the patient experiences pain.19 This is impractical in dogs. The US dosage that a patient is receiving usually cannot be monitored. In the past, in an effort to avoid tissue damage, the dosages have been low and the patient experiences no sensation. However, there is the possibility that the patient is not receiving a sufficient dose of US energy. More recent recommendations seem to address this issue. Typical duty cycles for pulsed mode US range from 0.05 (5%) to 0.5 (50%). For pulsed mode, the terms temporal peak intensity and pulse average intensity are used. Obviously pulsing decreases the pulse average intensity and decreases tissue heating. Pulsing may be used when the desired effect is based on a nonthermal mechanism or when minimal heating is desired, such as treating near bone.8 Low-intensity continuous mode could also be chosen for these purposes. The treatment area should be two to four times the size of the effective radiating area of the transducer head.19 Increasing the total area beyond the recommended area decreases the dosage and the heating effect. Experimental evidence indicates that a duration of 5 to 10 minutes is necessary to produce adequate tissue heating in an area equivalent to two to three times the diameter of the sound head.21,23 For instance when using direct coupling with topical US gel, continuous mode at 1.5 W/cm2 for 10 minutes, and moving the sound head at 4 cm per second, it took nearly 8 minutes for the temperature to reach therapeutic levels when temperature was measured at a depth of 3 cm in the gastrocnemius muscle of humans.12 For an intensity of 1.5 W/cm2 Draper recommends a duration of approximately 5 minutes at 3 MHz and at least 10 minutes at 1 MHz, assuming that an area twice the size of the effective radiating area of the transducer is treated.19 The findings in dogs (see Figure 19-1, A) support these recommendations. The recommended speed at which the sound head is moved over the skin is approximately 4 cm per second, or slower, to achieve uniform distribution of energy to the target tissues.10 Moving the transducer too quickly diminishes the heating and the therapist may have a tendency to cover too large an area. Various longitudinal and circular patterns may be used. The transducer should never be stationary when direct coupling is used. Because the US beam is nonuniform, some target areas within the beam could receive a large amount of energy. This predisposes target areas to hot spots and tissue damage, including endothelial damage and platelet aggregation. Keeping the transducer moving is not as critical with underwater applications because hot spots occur in the near field of the beam. Hot spots are situated in the water if a sufficient distance is maintained from the tissue. However, the distance may compromise the heating effect. Problems with achieving adequate tissue heating with the immersion technique have been previously described. Treatment schedules may include daily treatment initially, followed by less frequent sessions as the condition improves.7 Bromiley8 states that treatment can be given daily for up to 10 days, but should not exceed two 10-day courses without a 3-week rest. Similar recommendations have been made for horses.17 However, the scientific rationale for these recommendations is not clear. Tissue burns are a major concern of treatment.13 These may occur if the intensity is too high, treatment times are too long, or the transducer is held stationary, thereby concentrating energy in a small area. These same factors may put the patient at risk for cavitation, a phenomenon in which bubbles of dissolved gas form and grow during each rarefaction phase.10 Also if the transducer is inadvertently held in the air while emitting US, the face of the transducer may overheat. The transducer may become damaged, and the animal could be burned if the overheated surface of the transducer contacts the skin. Some units have a built-in system to prevent the crystal from overheating. Regarding safety of the therapist, some US energy is unavoidably propagated through the housing of the sound head to the hand of the therapist, but the effects of this “parasitic” exposure are unknown. Avoid direct US exposure to the following: • Carotid sinus or cervical ganglia. Ultrasound could alter the normal pacing of the heart or stimulate baroreceptors.7 • Eyes. Because blood supply to the lens is poor, heat is poorly dissipated and could result in cataracts. Retinal damage could also result.10 • Heart. Electrocardiographic changes have occurred in dogs. • Injured areas immediately after exercise.15,17 • Malignancy. Ultrasound applied to murine tumors resulted in larger tumors compared with controls.24 • Spinal cord if a laminectomy has been performed.7 However, US therapy has been advocated in the area around the spinous processes in horses25 and would also be acceptable in dogs if the bone is intact. • Testes. Temporary sterility could be associated with heating. • Wounds that are contaminated. Ultrasound could drive bacteria into the tissues26; infectious processes may be accelerated by heat.7 • Recent incision sites. It has been recommended not to treat incision sites with continuous US for the first 14 days to avoid dehiscence.17 • Exert precaution in the following situations: • Bone fracture. This is controversial. Concern exists that high doses retard callus formation, delay calcification,15 or cause pathologic fractures, subperiosteal damage, or demineralization.26 Others believe that US over fracture sites is acceptable unless sensation is impaired.9 Experimentally, low-intensity pulsed US may accelerate fracture healing.10 • Bony prominences. Treat around bony prominences rather than directly over them, to avoid concentrating energy at the periosteum, or use an immersion technique. Treat bony areas with low dosage levels to avoid the danger of pathologic fractures.8 • Cold packs or ice before US. Cold alters pain and temperature perception, limiting the patient’s ability to respond if the US intensity is too high. • Decreased blood circulation. Normal blood flow dissipates the heat that is generated. • Decreased pain and temperature sensation. Pain response serves as a sensitive monitor of excessively high intensities or faulty equipment17 that could cause burns or other tissue damage. • Animals that are overly sedated, restrained, or under local anesthesia. • Physeal areas in immature animals.8,10,15 High intensities could affect physes and bone growth. • Injuries in the acute stage that should not receive heat therapy.17 • Acute inflammatory joint disease. Intracapsular heating may accelerate destruction of articular cartilage in acute inflammatory joint disease.7 Note that metal implants are not necessarily a contraindication for US therapy. The effects of US on cementing compounds such as methylmethacrylate are unknown.10
Therapeutic Ultrasound

Physical Principles
Coupling Techniques
The Effect of the Hair Coat
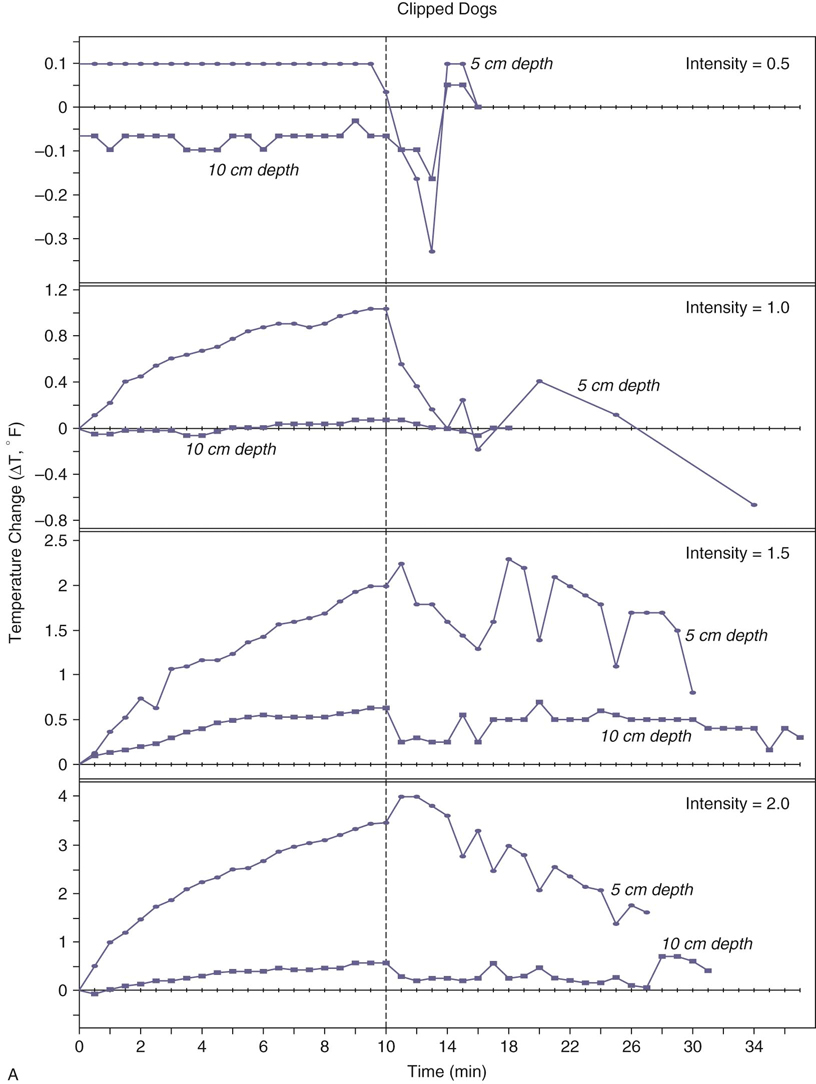
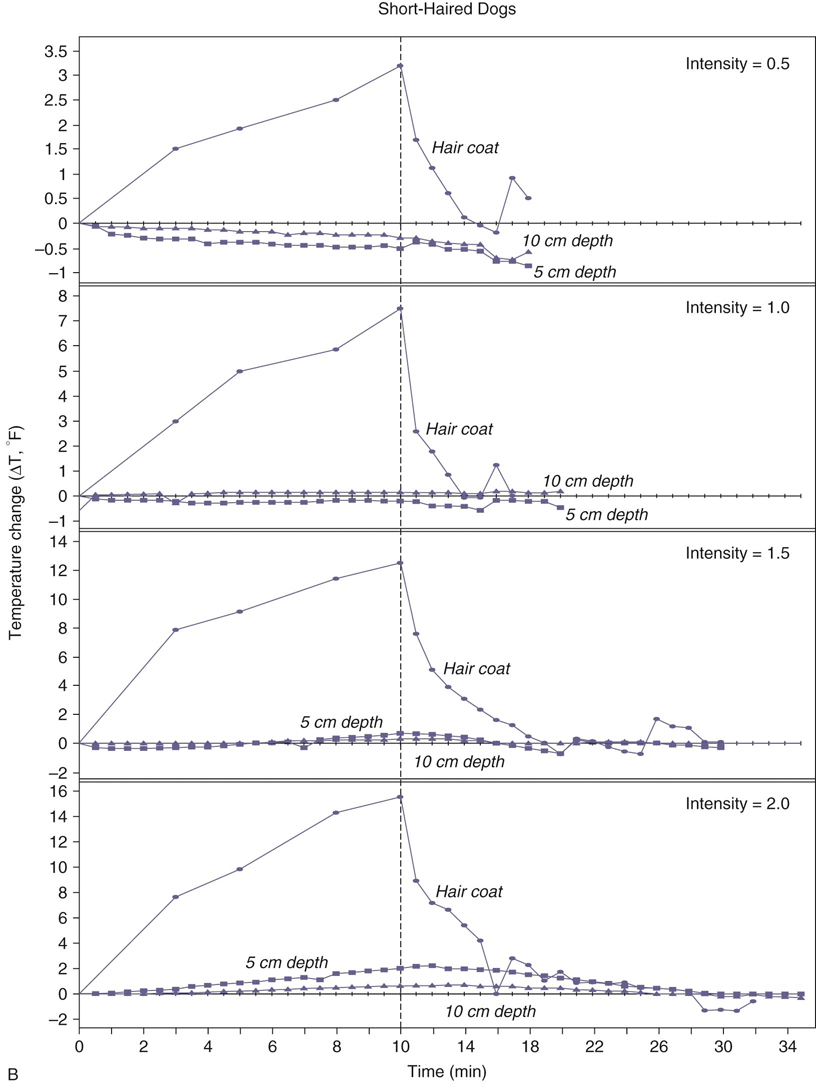
Figure 19-1 A, Intramuscular temperature changes measured at 5- and 10-cm depths during 1-MHz ultrasound at four intensities (W/cm2) applied to clipped skin over the caudal thigh in dogs. The vertical dashed line represents the end of 10 minutes of ultrasound exposure. The units on the y-axis differ for each intensity. B, Temperature changes measured intramuscularly at 5- and 10-cm depths and within the hair coat, during 1-MHz ultrasound at four intensities (W/cm2) applied over the caudal thigh in dogs with short hair coats (greyhounds). The vertical dashed line represents the end of 10 minutes of ultrasound exposure. The units on the y-axis differ for each intensity. (From Steiss JE, Adams CC: Effect of coat on rate of temperature increase in muscle during ultrasound treatment of dogs. Am J Vet Res 60:76-80, 1999.)
Treatment Variables
Precautions and Contraindications
Therapeutic Ultrasound
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree


