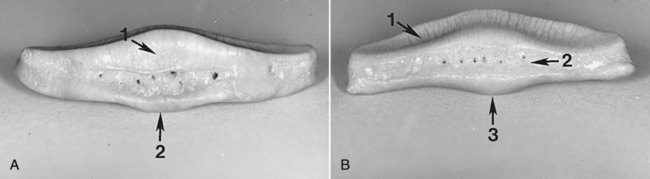
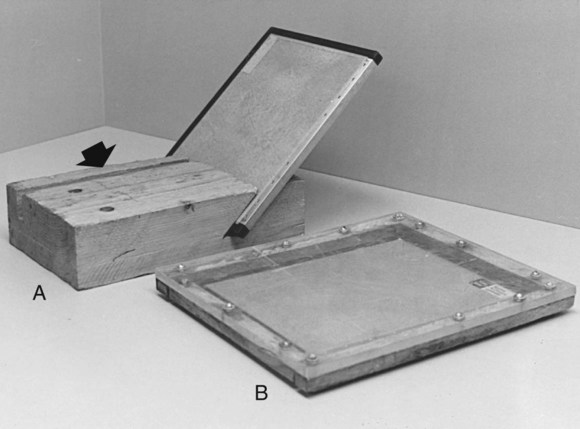
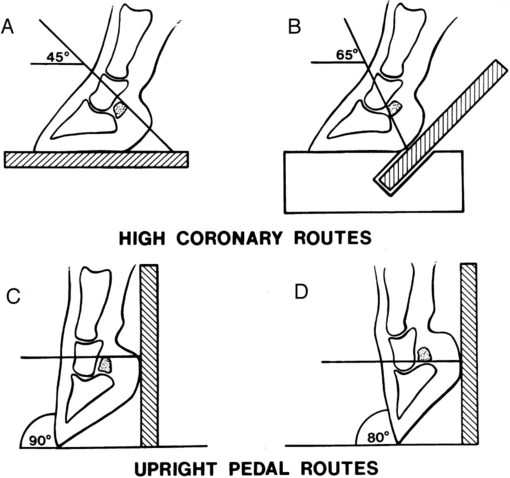
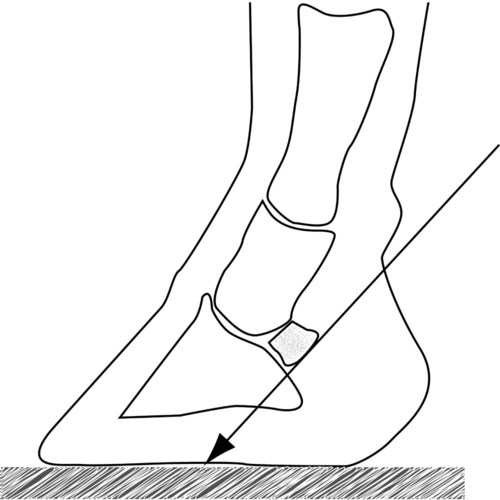
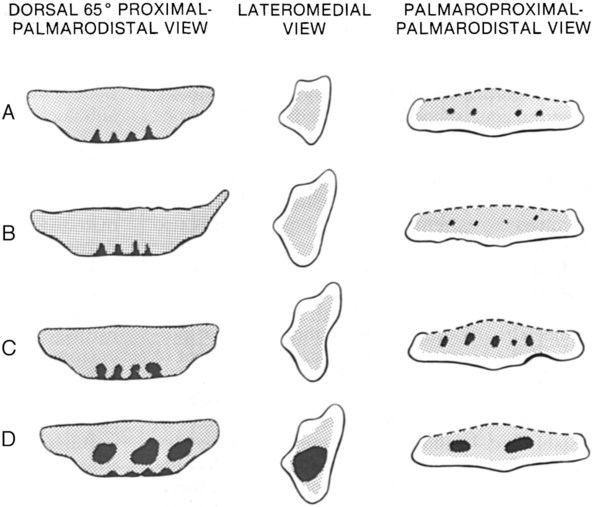
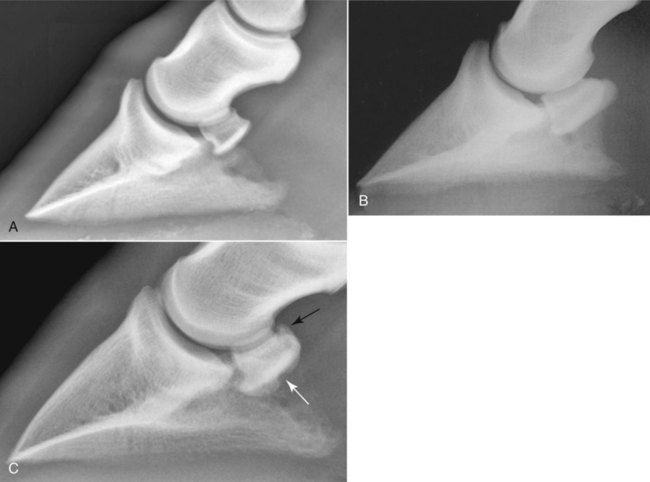
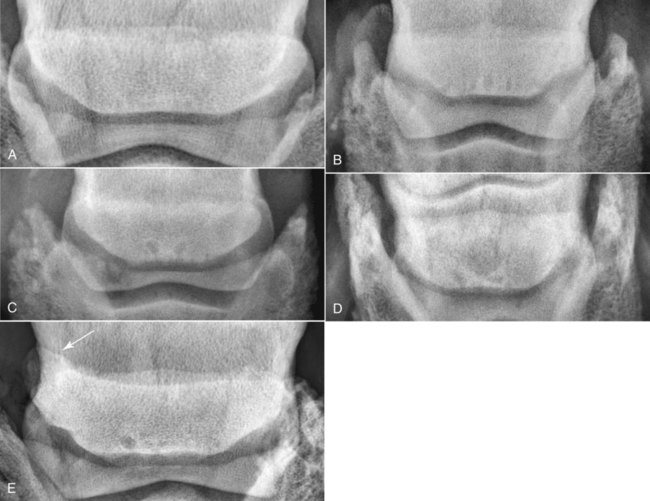
The normal radiographic anatomy of the navicular bone (distal sesamoid bone) is shown in Chapter 13. The navicular bone has two surfaces (flexor and articular), two borders (proximal and distal), and two extremities (medial and lateral). The navicular bone typically ossifies from a single center (Fig. 24-1).1 The navicular bone has two separate hyaline cartilage-covered articular surfaces. The larger proximal articular surface conforms to the condyles of the middle phalanx. A smaller distal articular surface, associated with the distal navicular border, is essentially a narrow facet that articulates with the distal phalanx. The distal articular surface of the navicular bone and the articular surface of the distal phalanx are usually parallel but can be convergent.2 The flexor surface has a prominent central ridge—termed the central eminence. The deep digital flexor tendon and adjacent bursa make contact with the fibrocartilage-covered flexor surface. The navicular bone is held in position by three strong ligaments. The paired suspensory navicular ligaments originate from the dorsolateral and dorsomedial aspects of the proximal phalanx and attach to the proximal navicular border and both extremities. The distal sesamoidean impar ligament originates from a projection on the distal navicular border just caudal to the articular surface and inserts on the distal phalanx deep to the deep digital flexor tendon. Blood vessels and sensory nerves traverse these ligaments and ramify into the navicular bone and synovial membrane by way of both borders.3 No evidence exists for an anatomic communication between the distal interphalangeal joint and the navicular bursa.4 Radiography is the first imaging modality employed for evaluation of the navicular bone.5 Indications include assessment of bony changes in navicular syndrome, the identification of significant bone abnormalities during prepurchase examination, the assessment of bone or bursal involvement in foot wounds or abscesses, the evaluation of suspected trauma, and the collection of information about the morphologic progression or remission of navicular bone abnormalities. Accurate radiographic evaluation of the navicular bone depends on a radiograph that is properly positioned and exposed and on a foot that is free of distracting artifacts. Proper preparation for navicular radiography is similar to that for the distal phalanx, as discussed in Chapter 23. Positioning aids, such as a reinforced cassette, grooved wooden blocks, and a cassette tunnel, assist in radiographic evaluation of the navicular bone (Fig. 24-2). Use of a grid for angular dorsoproximal-palmarodistal views is optional. A grid improves radiographic detail by reducing film fog from scatter radiation. Because the grid is fragile, its use is limited to techniques during which the foot does not bear weight directly on the grid, such as with a cassette tunnel. The location of the navicular bone and its complex shape require that at least three different views be made for complete evaluation. These include the angular dorsoproximal-palmarodistal views, the lateromedial view, and the palmaroproximal-palmarodistal (also called skyline) view (Box 24-1).2 The horizontal beam dorsopalmar view is an additional view that is helpful for evaluating the extremities of the navicular bone. In addition, dorsoproximolateral-palmarodistomedial and dorsoproximomedial-palmarodistolateral views project the extremities of the navicular bone without superimposition on the middle phalanx. Angular dorsoproximal-palmarodistal views of the navicular bone may be made by two different hoof-positioning techniques.6,7 These methods include (1) the high coronary stand-on route, in which the foot stands directly on a reinforced cassette, cassette tunnel, or grooved wooden block; the x-ray beam is centered just proximal to the coronary band and angled 45 or 65 degrees distally from horizontal and (2) the upright pedal route, in which the hoof rests on the toe in tiptoe fashion, with the dorsal hoof wall positioned either 80 or 90 degrees from horizontal; the x-ray beam is directed horizontally (Fig. 24-3). An undistorted projection of the proximal navicular border is achieved by using the 45-degree high coronary stand-on route or the 90-degree upright pedal route. The distal navicular border is obscured by these routes because it is projected below the level of the distal interphalangeal joint. Because only the proximal navicular border can be evaluated accurately in these two projections, they are used as supplemental views (Fig. 24-3, A and C). A 65-degree high coronary stand-on route or an 80-degree upright pedal route projects the distal navicular border proximal to the distal interphalangeal joint and superimposes the entire navicular bone behind the middle phalanx. The distal navicular border is well visualized, and although the proximal border is slightly distorted, it is readily identified. Either one of these two positioning methods is recommended for the angular dorsoproximal-palmarodistal projection because when they are done properly, the entire navicular bone is projected through the middle phalanx (Fig. 24-3, B and D). Stand-on techniques are technically easier but result in slightly more magnification of the navicular bone when compared with the upright pedal route.6 Magnification can be minimized on the high coronary stand-on route by using a grooved wooden block. A cassette and grid are placed in a precut groove behind the hoof as it rests on the block. Because of the position of the cassette, less magnification of the navicular bone occurs when compared with other stand-on techniques (see Fig. 24-3, B). The palmaroproximal-palmarodistal view, also called skyline view (Fig. 24-4), projects the flexor cortex, medulla, and central eminence. The concept is to isolate most of the bone between the palmar processes of the distal phalanx. The horse stands on a reinforced cassette or cassette tunnel. The foot is positioned as far caudal as possible while still bearing weight.8 Local analgesia may be required to obtain ideal foot positioning. Regardless of foot location, the primary beam is positioned tangential to the estimated plane of the flexor cortex and is centered between the bulbs of the heel. Too steep of a beam angle with the foot may result in superimposition of the ergot over the navicular bone. Reduced angulation alters the apparent width of the flexor cortex and results in an indistinct interface between cortical and trabecular bone and leads to an erroneous diagnosis of medullary sclerosis.8 Excessive superimposition of the palmar processes of the distal phalanx on the navicular bone can also occur. Oblique palmaroproximal-palmarodistal projections distort the navicular shape and superimpose it behind the palmar processes of the distal phalanx. In the angular dorsoproximal-palmarodistal views, the navicular bone is of uniform radiopacity. Its spindle shape varies somewhat from horse to horse. The extremities are fairly symmetric and are bluntly pointed. The proximal border is smoothly marginated. The shape of the proximal border has been classified variously as concave, undulating, straight, or convex.9,10 The distal border has a variable number (usually no more than seven) of cone-shaped radiolucencies representing synovial invaginations. Their size is variable, with the height being approximately 1.5 times the width of the cone at the base. Size is related to degree of work, although their shape should remain somewhat triangular. The lateral view offers a clear, unobstructed view of the navicular bone but presents a foreshortened image. Both extremities should be superimposed; a well-defined medullary cavity is visualized. The flexor surface is convex palmarly and is smoothly marginated. In some normal horses, a smoothly marginated dimple of variable depth is seen in the mid-portion of the central eminence. The proximal and distal borders are smooth, as are the articular surfaces. Some horses may have a mild elongation of the proximal or distal border, or both.2 The joint space between the navicular bone and the distal phalanx is usually parallel, but a convergent joint is sometimes present. In the palmaroproximal-palmarodistal view, a well-defined medullary cavity of uniform trabecular pattern with four or five small radiolucent invaginations may be seen. The cortex is of homogeneous opacity and is of uniform thickness centrally, with some thinning peripherally. The width of the flexor cortex varies from 2.0 to 3.6 mm because of breed differences and geometric magnification.2,8 The flexor surface is smoothly marginated with a central eminence, which is usually rounded and prominent, but in some horses may appear flattened normally. A small crescent-shaped radiolucency may be seen within the cortex of the central eminence, representing a normal midsagittal synovial fossa. This fossa is occasionally seen as a dimple on the flexor surface on the lateral view. In some horses, a lucent crescent is seen within the central eminence, even in bones without a dimple. This is caused by a trabecular bone island interposed between two parallel cortical bone plates of the central eminence.11,12 The ends of both extremities are rounded, being variably superimposed over the palmar processes of the distal phalanx. The articular surface is occasionally seen in this view. The term navicular disease is used in this discussion to denote a chronic progressive syndrome involving the navicular bone, its fibrocartilaginous flexor surface, its surrounding soft tissues, including the deep digital flexor tendon, distal sesamoidean impar ligament, collateral ligaments, and navicular bursa, and the distal interphalangeal joint.5 The precise source of pain in navicular lameness remains unclear. Variable response to local analgesia of the medial and lateral palmar digital nerves, the distal interphalangeal joint space, and the navicular bursa is noted. This variable response suggests that sensory nerves innervating the synovial membranes of the collateral sesamoidean ligament, the distal sesamoidean impar ligament, and the navicular bone itself play a separate or combined role in mediating pain in navicular disease.4,13 In addition, pain arising from the dorsal margin of the sole has been shown to be attenuated by analgesia of the distal interphalangeal joint or palmar digital nerve block.14 This further complicates the interpretation of nerve block results in horses suspected of having navicular origin pain. Navicular disease is primarily a slowly developing, intermittent, bilateral forelimb lameness.15 It is also occasionally recognized in the hindlimb. In general, navicular disease is most common between 3 and 18 years of age, with a peak incidence of 9 years of age at presentation. Males have involvement more often than do females, geldings have a greater risk than stallions, and the breed prevalence varies according to the population characteristics of the reporting institutions.16,17 Genetic factors have been implied in the susceptibility to navicular disease: for example, horses with a more concave or undulating proximal border have higher risk of developing the disease, presumably because of altered distribution of biomechanical forces.5 No pathognomonic clinical test is available for navicular disease. The diagnosis is based on a characteristic gait, localization of pain to the palmar part of the foot, identification of radiographic signs of navicular degeneration, and elimination of other causes of lameness.15,18 When navicular lameness is suspected, both feet should be radiographed because radiographic changes are often bilateral even if clinical signs are not. The pathophysiology of navicular disease is multifactorial; although there is no consensus on the exact pathogenesis of navicular disease, current research tends to support a biomechanical etiology, rather than vascular abnormalities.19 Classically, navicular disease has been characterized as navicular fibrocartilaginous degeneration with secondary tendon fibrillation, and later development of palmar cortex bone erosions.15,18 Recently, the timing of onset of these abnormalities has been questioned, and there is some evidence that vascular and matrix changes within the deep digital flexor tendon may precede changes in the fibrocartilage of the navicular bone.19,20 Other bony changes involving the distal border synovial invaginations (enlargement) have also been noted.21 Abnormalities such as dilated vessels, vascular thrombosis, granulation tissue, and empty synovium-lined invaginations have been observed histologically to a variable degree.3,18–24 The presence of histologic abnormalities in the distal sesamoidean impar ligament and sesamoidean collateral ligaments has also been described.25 Whether these findings represent a continuum of events or are separate, isolated abnormalities remains unclear. Enthesopathy involving the ligaments of the proximal and distal borders can occur with or without distal border foramina changes. Similar confusion exists regarding the significance of radiographic changes in the navicular bone in horses with lameness attributed to navicular disease. Poor correlation of pathologic and radiographic findings with clinical signs and prognosis has been demonstrated.16,23,23 Horses without radiographic abnormalities may have clinical navicular lameness, and horses with pathologic and radiographic changes may be sound.23,27 This paradox is explained in part by the fact that horses have different pain thresholds, are subjected to wide ranges of physical exercise, and are evaluated in variable stages of disease.8 Additionally, some pathologic changes may represent insignificant wear lesions or may be located in tissues of soft tissue opacity and thus are not radiographically discernible.18,28 Some authors agree that radiographic signs of navicular disease in an otherwise clinically normal horse are significant and may warrant a cautious prognosis for future soundness.8,29 However, no universal agreement exists regarding the clinical significance of all radiographic signs seen in navicular disease. Radiographic abnormalities associated with navicular degeneration are varied. Bony abnormalities may occur separately but usually occur in combination, unilaterally or bilaterally. Their clinical relevance regarding presence, absence, or degree of lameness in a given animal is varied.26 Additionally, no clear association exists between changes in the radiographic appearance of navicular bones and clinical outcome after treatment.30 Thus, radiographic changes of navicular degeneration must be interpreted in context with the presenting clinical signs. This is similar for other musculoskeletal conditions. The major radiographic signs of navicular degeneration are shown in Box 24-2. A diagram depicting various radiographic signs of navicular degeneration is shown in Figure 24-5. Radiographic manifestations of navicular degeneration and normal variants are shown in Figures 24-6 through 24-9.
The Equine Navicular Bone
Anatomy
Indications for Radiography
Preparation for Radiographic Evaluation
Radiographic Views
Dorsoproximal-Palmarodistal Views
Palmaroproximal-Palmarodistal View
Normal Radiographic Appearance
Navicular Disease
Radiographic Signs of Navicular Degeneration

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The Equine Navicular Bone