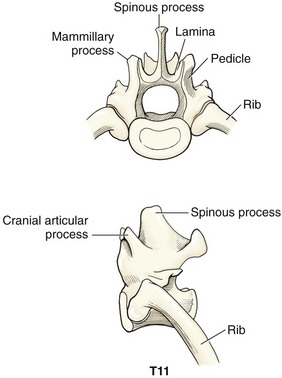
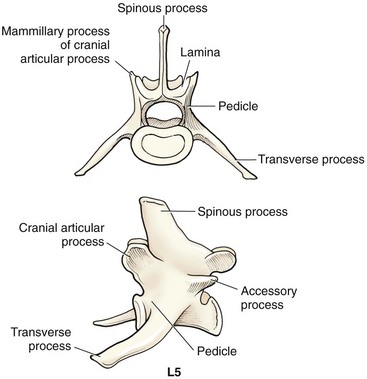
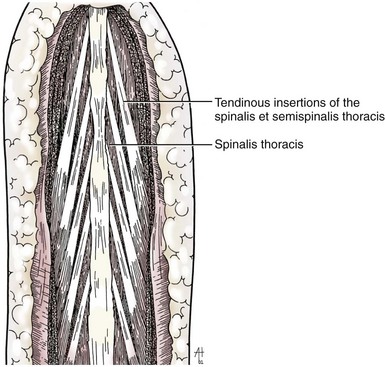
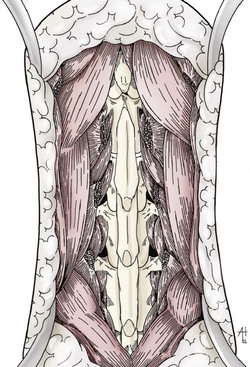
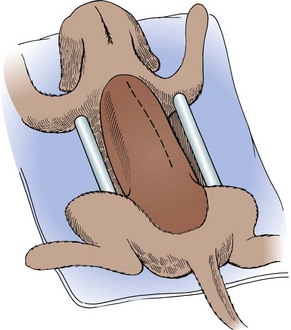
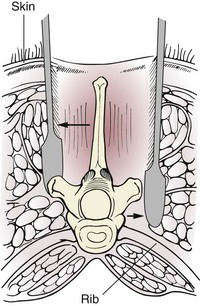
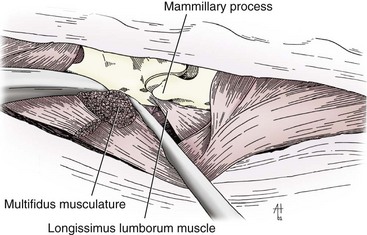
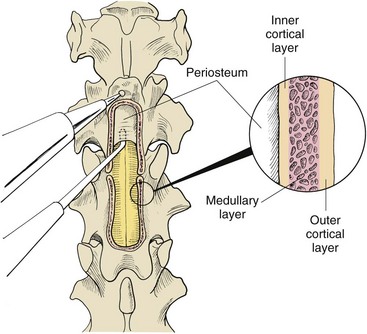
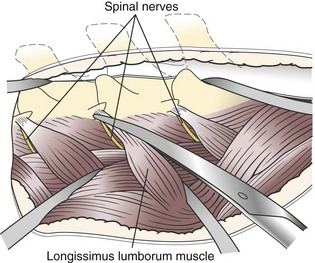
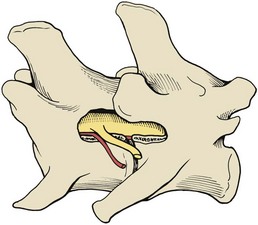
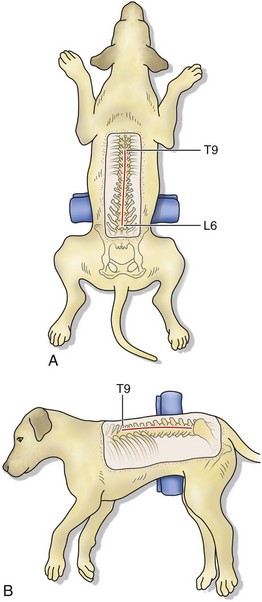
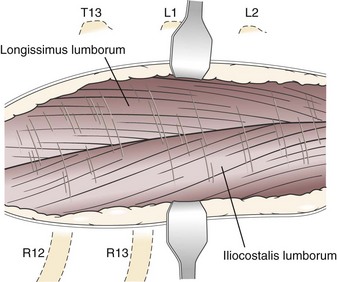
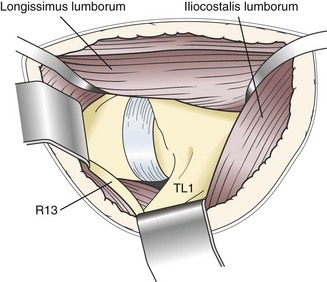
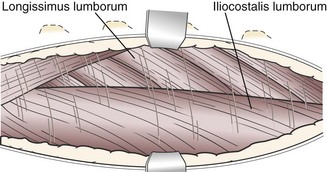
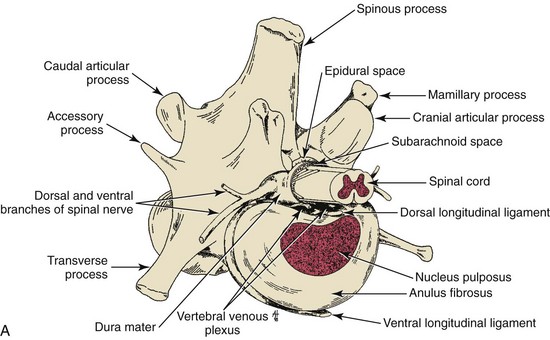
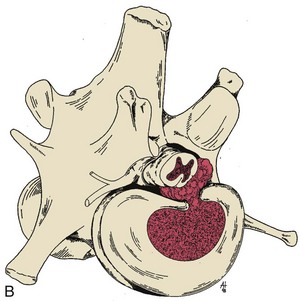
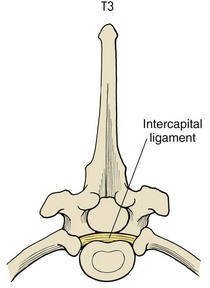
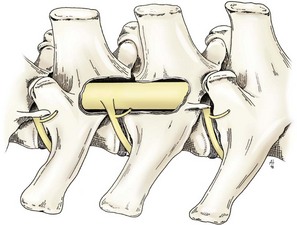
Chapter 41 Preoperative management of the patient with thoracolumbar myelopathy is similar to that described for the patient with cervical myelopathy (see Chapter 40). If instability is known or suspected (e.g., spinal trauma), the patient should be immobilized on a rigid surface, and excessive motion to the thoracolumbar spine should be prevented. A thorough neurologic examination is essential, as is a complete history of the patient’s neurologic status before hospital admission. In paraplegic patients, it is imperative to accurately assess the ability of the dog or cat to perceive noxious stimuli applied to the toes of the pelvic limbs. Absence of deep pain perception (see p. 1437) is a negative prognostic indicator, especially in trauma cases. The length of time that deep pain perception has been absent is inversely related to prognosis, emphasizing the importance of an accurate history. Assessment of neurologic dysfunction as UMN or lower motor neuron (LMN) in nature is important for localization purposes but does not affect prognosis. Similarly, the presence of Schiff-Sherrington posture (see p. 1428) is helpful in lesion localization but is not a prognostic indicator. Anesthetic management of the patient with thoracolumbar myelopathy is similar to that described for the patient with cervical myelopathy (see Chapter 40, pp. 1468 to 1469). Also, see Tables 32-5 and 32-6 on pp. 1045-1048 for anesthetic considerations in orthopedic patients. There are 13 thoracic vertebrae and 7 lumbar vertebrae. All of these vertebrae have similar components (vertebral body, lamina, pedicle, articular processes, transverse processes, dorsal spinous process), but these components differ substantially in size and shape along the vertebral column (Figs. 41-1 and 41-2). Of particular importance to the surgeon are the differences between the first 10 and the last 3 thoracic vertebrae and their articulations with each other. The articular processes from T1 through T10 are oriented dorsoventrally like the cervical articular processes (from C2-C3 caudally). Unlike the cervical articular processes, however, these thoracic articular processes do not present an obvious distinct anatomic boundary between what is articular process and what is lamina. From the T10-T11 articulation caudally, the joint spaces of the articular processes are located in a sagittal plane, with the cranial articular process joint surface facing medially and the caudal articular process joint surface facing laterally. The tubercles of the ribs articulate with the transverse processes of the thoracic vertebrae of the same number. The dorsal spinous processes of the thoracic vertebrae decrease in height from cranial to caudal and change from a caudal to a cranial orientation typically after the 11th (anticlinal) thoracic vertebra, whose dorsal spinous process is oriented dorsally. From mid-thoracic to approximately the 5th or 6th lumbar vertebra, there is a distinct accessory process lateral to and at the ventral base of the cranial articular process. From the T11-T12 space caudally, the intervertebral foramen is ventral to the accessory process; from T10-T11 cranially, the intervertebral foramen is located between the accessory process and articular processes. The lumbar vertebrae have large distinctive transverse processes that are oriented cranially and slightly ventrolaterally. The “elbow” of these processes (the cranial aspect of the base of the process near the junction with the pedicle) represents an important surgical landmark for implant placement. The dorsal spinous processes of the lumbar vertebrae are directed slightly cranially; they are largest in the mid-lumbar region. The dorsal spinous process of the 7th lumbar vertebra is palpably shorter than that of the 6th lumbar vertebra. Dorsal Approach to the Cranial and Mid-Thoracic Spine The most common indications for the dorsal approach to this region of the thoracic spine include removal of tumors and stabilization/decompression of congenital vertebral anomalies (e.g., hemivertebrae). In the latter scenario, it is essential to understand that stabilization of the abnormal region is mandatory. Position the patient in sternal recumbency with the thoracic limbs pulled cranially (Fig. 41-3) and close to the body. Alternatively, cross the thoracic limbs. The goal is to abduct the dorsal scapulae so that they do not interfere with the approach. Make a dorsal midline incision from caudal cervical to caudal thoracic region (depending on the specific region of interest and the specific procedure to be performed). Incise the subcutaneous tissue to expose the median raphe. Incise the raphe on either side of the transverse processes, controlling hemorrhage with monopolar or bipolar cautery. Retract the trapezius and underlying rhomboideus muscles laterally to expose the serratus dorsalis musculature. Incise the fascia of this musculature along either side of the median raphe close to the dorsal spinous processes, and reflect these muscles laterally to expose the spinalis et semispinalis thoracis musculature and associated tendinous insertions on the dorsal spinous processes (Fig. 41-4). Sharply incise the attachments of these muscles to the dorsolateral aspects of the dorsal spinous processes bilaterally, and then elevate these and deeper epaxial muscles off of the lateral aspects of the dorsal spinous processes using Freer elevators (small dogs and cats) or Army/Navy osteotomes. Insert Gelpi retractors at the caudal and cranial aspects of the incision at this time, and remove epaxial musculature from the articular processes to the level of the rib tubercle (if indicated) using a combination of sharp and blunt dissection and bipolar cautery. Several options are available for performing decompression at this point. In the author’s opinion, the dorsal spinous processes should be preserved and a full dorsal laminectomy avoided if at all possible. In this region of the spine, the articular facets probably contribute more to spinal stability than in other regions of the spine, and these facets are difficult to distinguish from laminae at their medial aspects. Perform a hemilaminectomy using a high-speed air drill, taking care to avoid the intervertebral foramen while drilling. Drill through outer cortical and inner cancellous bone as described for dorsal laminectomy of the cervical region (see Chapter 40, p. 1488), then carefully drill the inner cortical layer until it is thin and flaky (like filo dough). In small breed dogs and cats, the bone in this region of the spine may not have an obvious cancellous layer. Once the inner cortical layer is thin enough, remove it with a probe (e.g., Gross ear hook and spoon) or fine-tipped Lempert rongeurs. If necessary, undercut the lamina beneath the dorsal spinous process to midline or slightly past midline for increased exposure (Fig. 41-5). If a complete dorsal laminectomy is performed, stabilize the spine. Close the incision routinely. This approach is the most frequently used in veterinary spinal surgery. It provides access to dorsal, lateral, and ventrolateral aspects of the vertebrae and spinal cord. Dorsal laminectomy, hemilaminectomy, and combinations of these two procedures can be performed via this approach. Indications for this approach include removal of compressive masses (e.g., disk material, hemorrhage, neoplasia, fracture fragments) and application of implants. Position the patient in sternal recumbency with the thoracic and pelvic limbs in a flexed position (Fig. 41-6). Create a dorsal midline incision approximately three vertebral lengths cranial and caudal to the region of interest. Incise through subcutaneous fat and fascia to reveal the thoracolumbar fascia. Incise the thoracolumbar fascia (unilaterally for a hemilaminectomy, bilaterally for a dorsal laminectomy) just lateral to a dorsal spinous process at the caudal aspect of the incision, and continue the fascial incision cranially using Mayo scissors. Angle the scissor blades away from you to avoid a flap of fascia that will hang into the approach. Use Freer elevators or Army/Navy osteotomes to subperiosteally elevate the multifidus musculature off the lateral aspects of the dorsal spinous processes (Fig. 41-7). Remove any remaining muscular attachments with Metzenbaum scissors. Working caudally to cranially, place a Freer elevator or a small osteotome beneath the multifidus muscle caudal to the articular processes (facets), and pull the muscle dorsally and cranially over the facets, elevating the muscle attachments off of the facets with another elevator or osteotome. At the cranial aspect of the facets, locate the white fibrous attachment of the multifidus musculature to the mammillary process (on the cranial articular facet), and remove this attachment with Mayo scissors and/or bipolar cautery (Fig. 41-8). Repeat this process for the remainder of the facets to be uncovered. Place Gelpi retractors in the cranial and caudal aspects of the incision. Place both ends of the Gelpi retractors beneath the multifidus musculature. If the dissection already described has been performed bilaterally, exposure is sufficient for performing a dorsal laminectomy. To perform a dorsal laminectomy, remove the dorsal spinous processes over the intended laminectomy site using bone cutters or double-action rongeurs. Use a high-speed air drill to remove the outer cortical, inner cancellous and inner cortical bone layers as previously described (Fig. 41-9). To perform a hemilaminectomy, locate the tendons of insertion of the longissimus lumborum musculature, and transect these tendons from their insertions on the accessory process with sharp Metzenbaum scissors or bipolar cautery (Fig. 41-10). Spinal nerves and blood vessels are located beneath these tendons and should be avoided. Remove portions of the articular processes using a Lempert or Ruskin rongeur to make this region more level with the pedicle. Use a high-speed air drill to remove the pedicle, the articular processes, and part of the lamina (undercut the dorsal spinous process). The bone transition of outer cortical–inner cancellous–inner cortical is similar to that described for dorsal laminectomy. Because of the curvilinear shape of the area to be removed, the dorsal and ventral aspects of the hemilaminectomy are thicker than the middle section. Concentrating on the middle section will likely result in the creation of a narrow hemilaminectomy defect. The author prefers to create a wide, rectangular defect (Fig. 41-11) to provide adequate decompression and to allow for ready removal of compressive tissue. The author also prefers to leave the accessory process intact until the hemilaminectomy is completed (decreased chance of hemorrhage); this process is easily “snipped” off using the tips of Lempert rongeurs, if indicated. The venous sinuses are likely to be visualized with this approach. If venous sinus hemorrhage occurs, control the hemorrhage with Surgicel or Gelfoam as described for cervical spinal surgery (see Chapter 40, p. 1468). FIG 41-11 Diagrammatic representation showing the location and extent of a typical left-sided hemilaminectomy. A miniaturized version of the hemilaminectomy, called a pediculectomy (Fig. 41-12), can also be performed via this approach. Close the incision routinely. There are limited applications for these approaches to the spine, which include access to intervertebral disks for fenestration, exposure for pediculectomy, and exposure for lateral corpectomy. These approaches can be performed with the patient in sternal, oblique sternal, or lateral recumbency, depending on surgeon preference. Create a skin incision lateral to the dorsal midline at approximately the levels of the rib heads and transverse processes (depending on the specific region to be exposed) for the lateral approach and at 1.0 to 2.0 cm lateral to the midline for the dorsolateral approach (Fig. 41-13). Incise through subcutaneous fat and fascia to reach the thoracolumbar fascia. Incise the thoracolumbar fascia to expose an underlying second layer of fat and the thoracolumbar musculature. For the lateral approach, identify and bluntly dissect between the fascicles of the iliocostalis lumborum muscles to expose the rib head or the transverse process (Fig 41-14). Clear the musculature off the pedicle and disk space using a Freer elevator, and retract the iliocostalis lumborum fascicles with Gelpi retractors (Fig. 41-15). For the dorsolateral approach, bluntly separate between the longissimus lumborum and multifidus lumborum at the septum between these muscle masses (Fig. 41-16) in a craniomedial direction until the tendons of the longissimus muscles are revealed, inserting on the accessory processes. Elevate the musculature off of the intended region of exposure as described for the lateral approach, using Freer elevators. Close the incision routinely. The neurosurgical instrumentation required for surgery of the thoracolumbar spine is essentially the same as that used for brain (p. 1446) and cervical spine surgery (p. 1490). For some thoracolumbar fracture/luxation scenarios, both basic plating equipment (see pp. 1086-1093) and specialized plates (e.g., Lubra plates, Auburn plates) may be required, depending on surgeon preference. Postoperative care of the thoracolumbar surgical patient is similar to what is described for surgery of the cervical spine (see p. 1477). Patients with thoracolumbar spinal cord disease are more likely to be non-ambulatory than dogs with cervical lesions and more likely to have UMN urinary incontinence. Therefore, physical therapy and attentive bladder management is commonly required for these patients. It is prudent to keep patients hospitalized until they are able to urinate on their own, as many owners have difficulty with bladder expression. The majority of dogs and cats with thoracolumbar spinal cord injuries who have voluntary pelvic limb motor function are able to urinate voluntarily. In patients with no deep pain perception to the pelvic limbs, functional recovery is often prolonged or unlikely. In these scenarios, teaching pet owners about bladder management and principles of physical therapy is often necessary. A number of carts are available for patients who are expected to be nonambulatory paraparetic or paraplegic for extended periods of time. Complications associated with thoracolumbar spine surgery are similar to those described for cervical spine surgery (see p. 1477). When working in the cranial to mid-thoracic spine, especially if near the rib heads, pneumothorax is a possible complication. Inadvertent damage to thoracic or lumbar nerve roots during surgery may lead to a transient visible bulge of a section of abdominal musculature on the operated side. Although uncommonly reported, very wide dorsal laminectomies may predispose to the development of a constrictive laminectomy “membrane” (scar tissue). Specific Diseases As discussed with cervical disk disease (see p. 1508), thoracolumbar disk disease refers to degeneration of the nucleus pulposus (Hansen type I or Type I degeneration) or the annulus fibrosus (Hansen type II or Type II degeneration) and the clinical consequences of this degeneration. Type I degeneration is also called chondroid degeneration, and type II degeneration is called fibroid degeneration. The pathophysiology of disk disease is discussed in Chapter 40 under cervical disk disease (p. 1478). Type I disk extrusions in dogs and cats (much less common) are usually ventral or ventrolateral (Fig. 41-17). Disk disease in the thoracolumbar region is more frequently encountered than cervical disk disease. Disk problems cranial to the T10-T11 disk space are uncommon, probably because of the stabilizing influence of the intercapital ligament (Fig. 41-18). This ligament passes over the dorsal annulus from rib head to rib head in all but the first pair and the last two pairs of ribs. Type I disk extrusions usually occur between vertebral levels T11 and L3. The T12-T13 and T13-L1 disks are the most common sites for type I disk extrusions to occur in small breed dogs. In larger dogs, the L1-L2 and L2-L3 disk spaces are the most common sites for type I extrusions. The L4-L5 intervertebral disk space appears to be the most common site for thoracolumbar disk extrusion in cats. The typical signalment for patients with thoracolumbar disk disease is essentially the same as that described in Chapter 40 (see p. 1479). Although most dogs that present with type I disk extrusions are small breeds, large breed dogs are also occasionally afflicted by type I disk extrusions. In one report of thoracolumbar disk disease in large (more than 15 kg) nonchondrodystrophic dogs (Cudia et al, 1997), 92% of the cases were found to have type I disk extrusions. Large dog breeds that seem to be most commonly encountered with type I disk extrusions include mixed breed, German Shepherds, Labrador Retrievers, Doberman Pinschers, and Rottweilers.
Surgery of the Thoracolumbar Spine
General Principles and Techniques
General Considerations
Preoperative Management
Anesthetic Considerations
Surgical Anatomy
Standard Surgical Approaches to the Thoracolumbar Spine
Dorsal Approach to the Thoracolumbar Spine
Dorsal laminectomy
Lateral and Dorsolateral Approaches to the Thoracolumbar Spine
Suture Materials and Special Instruments
Postoperative Care and Assessment
Complications
Thoracolumbar Disk Disease
General Considerations and Clinically Relevant Pathophysiology
Diagnosis
Signalment.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree