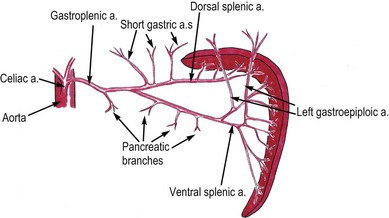
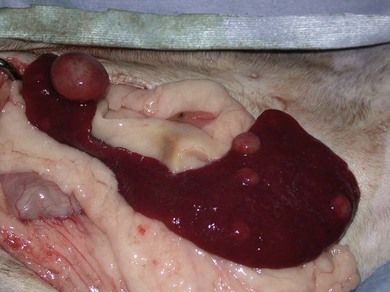
Chapter 34 Disease of the feline spleen is not common. Splenic lesions in feline necropsy specimens range from 0.3–5.9%1,2 and so veterinary surgeons can go many years without ever knowingly encountering feline splenic disease. Splenomegaly, or splenic enlargement, may be diffuse (symmetric) or focal (asymmetric) and feline splenic disease is more likely to be neoplastic than canine splenic disease2 with up to 73% of splenic changes being neoplastic.3 Despite this, however, the feline spleen is less frequently removed than its canine counterpart. This chapter outlines broad principles involved with splenic disease, with attention paid to the spectrum of conditions encountered in the cat. The spleen is often not immediately visible on opening the abdomen, where it is located in the left cranial quadrant. The head of the spleen is closely associated with the fundus of the stomach and the body and tail can be entirely on the left or move more towards the midline. The blood supply comes from the celiac artery; branches are sent off to the left lobe of the pancreas, and then the splenic artery divides into dorsal and ventral branches a centimeter or so from the spleen. The ventral branch arborizes with the left gastroepiploic artery after supplying the main body of the spleen. The dorsal branch gives rise to the short gastric arteries after supplying the dorsal extremity of the spleen. Venous drainage is via the splenic vein, which drains into the portal vein via the gastrosplenic vein (Fig. 34-1). There are unique ultrastructural properties of the non-sinusoidal feline spleen which make it unable to remove non-deformable erythrocytes containing Heinz bodies from the circulation,4 resulting in the high incidence of Heinz bodies in clinically normal cats.5 Cats presenting with splenic disease are typically older, with a median age of 12 years, and with no sex predilection.6 Presenting signs of splenic disease in cats are typically non-specific, and the history usually includes weight loss, anorexia, lethargy and vomiting.3 A palpable abdominal mass or splenomegaly is found in approximately 50% of cases,3,6,7 although the spleen is usually enlarged in over 80% of cats with lymphoma. It is typical to find splenomegaly when the spleen is infiltrated with mast cells, and the spleen is often irregular in contour.3 These patients also often present with anorexia and vomiting due to gastric and duodenal ulcers from paraneoplastic histamine release.8 Most cases of hemoperitoneum in cats are traumatic in nature and evidence of abdominal effusion or a palpable abdominal mass is often absent.7 Following blunt trauma, the spleen and liver are the most likely sources of severe ongoing hemorrhage.9 The clinical signs tend to be non-specific and include lethargy, anorexia, vomiting, abdominal distension, generalized weakness, pale mucous membranes, hemoglobinuria, and sometimes syncope and overt signs of shock. Cats rarely present with spontaneous hemoperitoneum, with only four cats out of 19 undergoing splenectomy having free abdominal blood in one study.6 In spontaneous hemoperitoneum cases bleeding occurs most commonly from the liver, with the spleen only accounting for 17% of cases. A ruptured spleen from hemangiosarcoma is the most common neoplastic cause although neoplasia only accounted for 46% of cases. Splenic lymphoma is a rare cause of spontaneous hemoperitoneum.7,10 Cats with spontaneous hemoabdomen are often anemic, with many having a packed cell volume of 20% or lower. An increased reticulocyte count and thrombocytopenia are also frequently found.6,7 Decreases in total protein, often through hypoalbuminemia, are common. Cats with hemoabdomen also often have high serum lactate levels, indicative of their low circulating blood volume and poor blood pressure. Elevations in serum urea and creatinine may also be present, typically with a pre-renal cause. With primary visceral mast cell disease involving the spleen, it is common to see a circulating eosinophilia and up to 40% of cats have a buffy coat layer that is positive for mast cells.11 Erythrocytosis due to catecholamine release as seen in dogs is not expected in cats, as they lack the muscular component to the spleen and sinusoid splenic blood.12 Ultrasound is the most useful imaging modality for examination of the spleen though inflated thoracic radiographs or computer tomography13 are used to screen for metastatic disease. The normal feline spleen is diffusely homogenous, has a finer echotexture than the liver (like the dog), and is more echogenic than the liver or renal cortex. Splenic masses can appear both hypoechoic and hyperechoic on ultrasound.7 The spleen in cats with lymphoma is reportedly diffusely hypoechoic, mottled in texture and may contain small hypoechoic foci, although the foci can be up to 1–2 cm in diameter.3,14 Abdominal effusion and at least one enlarged abdominal lymph node are also found. Myeloproliferative disease involving the spleen is also diffusely hypoechoic. Mast cell disease often results in a subjectively larger spleen, with a diffusely hypoechoic or nodular/mottled texture although it might present as single or multiple nodules.15 Liver involvement is also present in approximately 30% of cases. No characteristics allowing differentiation of cats with lymphosarcoma from cats with mast cell tumor have been described, although the former are more likely to have abdominal effusion or lymphadenopathy.3 Common incidental findings in feline spleens include myelolipomas which are well-defined, hyperechoic foci.16 Rarely, the splenic vein will thrombose, normally in association with feline liver disease or portal vein thrombosis; in this situation color flow Doppler will reveal no flow within the spleen.17 Computed tomography is increasingly being explored for staging of neoplasia involving intra-abdominal organs such as the spleen, or for identifying the origin of an abdominal mass.18 It is likely this practice will increase with growing availability of these scanners. Magnetic resonance imaging (MRI) is not widely used at this time for imaging the feline cranial abdomen although the appearance of normal liver, spleen, kidneys, and pancreas has been published as a reference guide.19 Ultrasound-guided fine needle aspirates can be used to distinguish causes of splenomegaly, and they provided a diagnostic sample in 81 of 101 cats,3 although in another study fine needle aspirates could not identify an underlying cause of splenomegaly in two of five cats20 and in another study cytology only corresponded to the histologic diagnosis in 61% of splenic aspirates, although this included cats and dogs.21 The cat is sedated and positioned in right lateral or dorsal recumbency and a 23G or 25G 1–1.5 inch needle is used. Samples should be collected with a non-aspiration technique (needle pushed into spleen and retracted and redirected several times), as this has been shown in the feline spleen to provide higher cellularity and less blood yet the same cell morphology compared to samples obtained by aspiration techniques (applying suction through a syringe).22 There is no evidence to suggest that bleeding is common or important after splenic aspiration in cats, even in the face of thrombocytopenia.23 There is also no evidence in the cat or dog to suggest splenic aspiration has resulted in tumor-seeding to the needle tract in the body wall. Surgery is not always indicated in splenic disease. The proper diagnostic tests (along with signalment, history, and clinical signs) should be pursued to obtain the most accurate diagnosis. These tests may include hematology, imaging, and cytology as addressed above, as well as biochemical analysis, bone marrow aspirate to rule out myeloproliferative diseases or leukemia (acute myeloid leukemia or chronic myeloid leukemia),24–27 polymerase chain reaction to rule out specific infectious agents,28–30 culture for fungal30 or bacterial splenitis or possibly bacteremia inducing immune-responsive splenomegaly/hyperplasia. Also, while these diseases are less common, genetic tests are available to rule out specific hemolytic (e.g., pyruvate kinase deficiency)31,32 or storage diseases, which can also result in splenomegaly. Special stains on cytological samples may also be of benefit.26,27,33 Surgical conditions of the feline spleen include laceration, torsion, some neoplasia (benign and malignant), and occasionally other causes such as foreign bodies and abscesses, as listed in Box 34-1. Abscesses within the spleen are uncommon in the cat and usually found in association with hepatic abscesses.39 Many neoplastic conditions, when limited to the spleen, warrant surgical intervention (e.g., splenic mast cell tumor, hemangiosarcoma, leiomyosarcoma, fibrosarcoma), but many do not (Box 34-1). Conditions of the spleen may be generalized or localized, but the decision about whether a patient requires surgery is more dependent on the overall clinical situation rather than the exact distribution of lesions within the spleen.
Spleen
Surgical anatomy
General considerations
History and clinical signs
Hemoperitoneum
Blood analysis
Imaging
Cytology
Surgical diseases