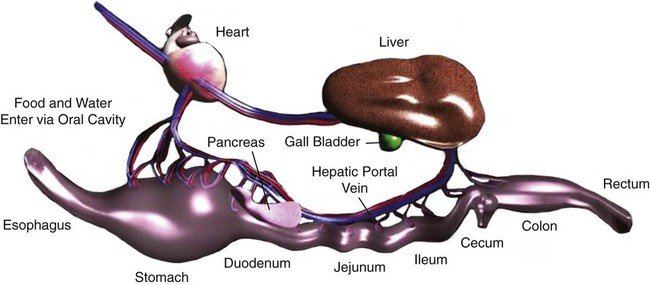
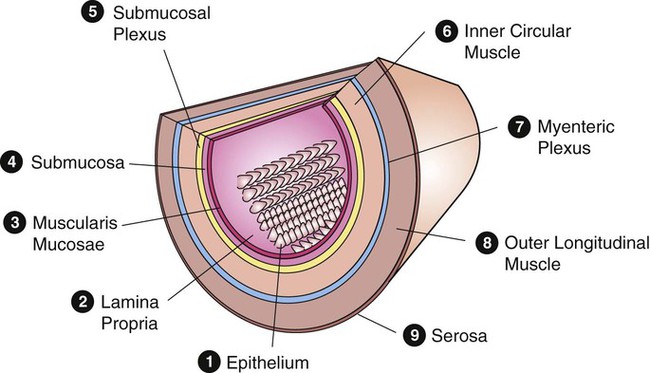
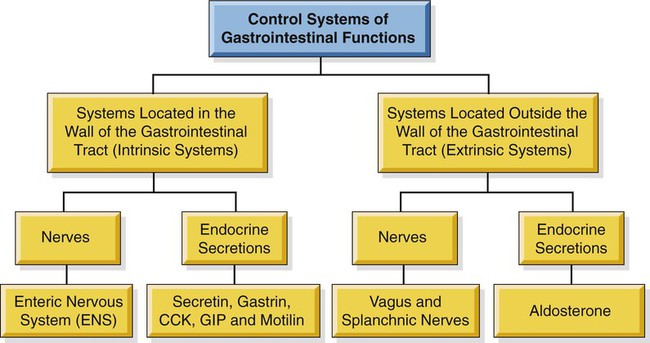
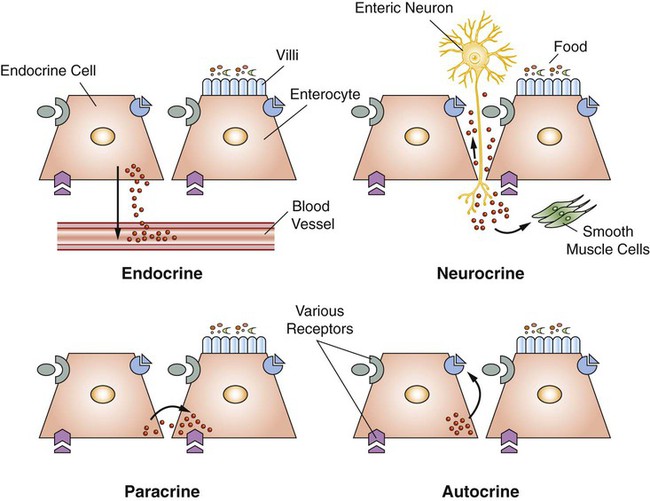
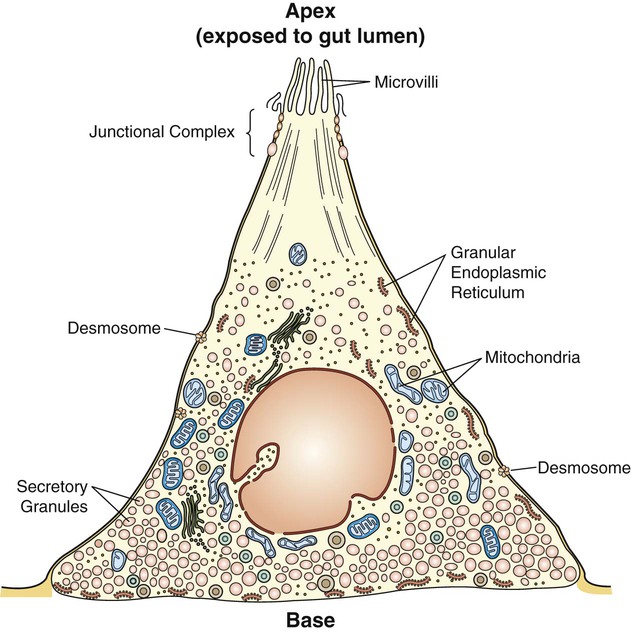
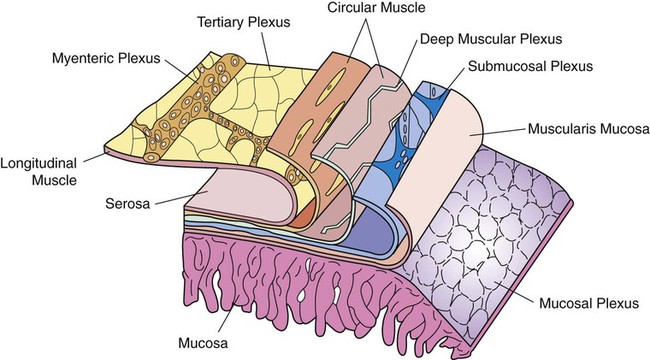
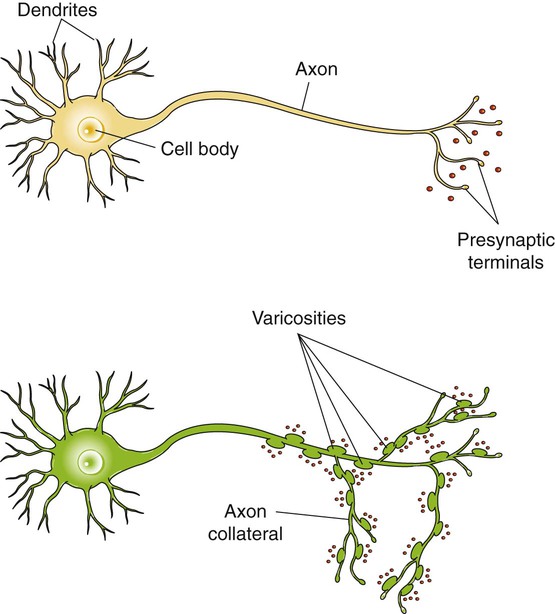
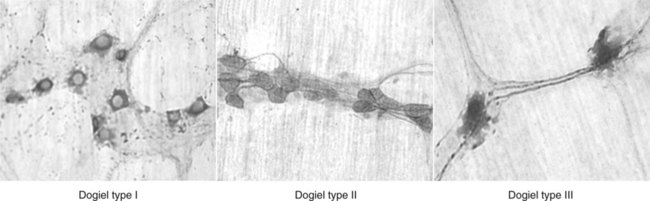
1. The gastrointestinal tract, or gut, supplies the body with nutrients, electrolytes, and water by performing five functions: motility, secretion, digestion, absorption, and storage. 2. Intrinsic and extrinsic control systems regulate various functions of the gut. 3. The intrinsic neuronal control system of the gastrointestinal tract is the enteric nervous system. 4. The intrinsic hormonal control system of the gut consists of five hormones including secretin, gastrin, cholecystokinin, gastric inhibitory polypeptide, and motilin. 5. The immune system of the gut is extensive and interacts with the regulatory systems of the gastrointestinal tract to control the various functions of the gut. 6. The extrinsic neuronal control system of the gut is comprised of two nerves: the vagus and the splanchnic. 7. The extrinsic hormonal control system of the gut is limited to one hormone: aldosterone. The digestive system consists of two parts, the gastrointestinal (GI) tract and the major digestive accessory glands, which include the liver and pancreas (Figure 27-1). This chapter focuses on the control systems that regulate the various functions of the GI tract. The control systems that regulate the functions of the liver and pancreas will be discussed in Chapter 29. The GI tract, also known as the gut, is a tube-like structure that extends from the mouth to the anus. Histologically, this tube consists of four main layers: (1) the mucosa, which comprises epithelial cells (enterocytes, endocrine cells, and others), the lamina propria, and the muscularis mucosae; (2) the submucosa; (3) two muscle layers, an inner thick circular layer and an outer thin longitudinal layer; and (4) a serosal layer (Figure 27-2). Functionally, the GI tract supplies the body, including the gut itself, with nutrients, electrolytes, and water. To supply the body with these substances, the gut performs five functions: motility, secretion, digestion, absorption, and storage. On the basis of the needs of the various organ systems in the body, the GI tract orchestrates and controls these five functions through two control systems, intrinsic and extrinsic. The intrinsic control system elements are located between the different layers of the gut, whereas the extrinsic control system resides outside the wall of the GI tract. Each of these systems consists of two components, namely, nerves and endocrine secretions (Figure 27-3). The secretions of the intrinsic and extrinsic control systems of the gut are regulatory and not digestive in nature (Box 27-1). That is, they regulate the activity of cells and tissues of the GI tract, but are not secreted into the gut lumen. They reach their target tissues by four different routes (Figure 27-4). Endocrine secretions are deposited close to blood vessels, and then blood cells carry the secretions to their target tissues. Paracrine denotes peptides secreted from cells with subsequent diffusion through the interstitial space to contact and affect other cells. Autocrine secretions of a given cell modify or regulate functions of the same cell. Neurocrine refers to secretion by enteric neurons of neuromodulators or regulatory peptides that affect nearby muscle cells, glands, or blood vessels. The endocrine and paracrine cells of the gut are columnar in shape with a wide base and a narrow apex (Figure 27-5). The narrow apex of the cell is exposed to the lumen of the gut, which allows it to “sample” or “taste” the luminal contents and respond to such stimuli by releasing hormones and/or other regulatory substances/peptides. The endocrine and paracrine cells have wide bases that contain secretory granules (storage forms of hormones and paracrine substances). This design allows cells to spread their secretions in a much wider area. Anatomically, the ENS consists of two main ganglionated plexuses, termed the submucosal (Meissner) and myenteric (Auerbach) plexuses. The submucosal plexus is located under the submucosal layer of the gut, and the myenteric plexus resides between the inner circular muscle layer and the outer longitudinal muscle layer (Figure 27-6). The enteric plexuses communicate with each other through interneurons and with the CNS through vagal, pelvic, and splanchnic nerves. In general, the enteric neurons consist of sensory (afferent) neurons, interneurons, and motor (efferent) neurons. Sensory input comes from mechanoreceptors within the muscular layers and chemoreceptors within the mucosa. Mechanoreceptors monitor distention of the gut wall, whereas chemoreceptors in the mucosa monitor chemical conditions in the gut lumen. Enteric motor nerves supply vascular muscle, gut muscle, and glands within the gut wall. Efferent neurons of the ENS may be stimulatory or inhibitory. The nature of their action is largely determined by the type of neurocrine substance they secrete and the nature of the receptors activated (Table 27-1). TABLE 27-1 MMC, Migrating motor complex. Unlike classical neurons, the enteric neurons release their neurotransmitter/neuromodulator molecules from vesicles located in swellings along often extensive branches of the axon, not just at the level of the distal synaptic terminals. These swellings are referred to as varicosities (Figure 27-7). The varicosities contain regulatory peptides, substances collectively known as neurocrines. These substances are secreted in response to action potentials, and they affect the activities of nearby smooth muscles or glandular cells. The presence of varicosities in the enteric neurons allows these neurons to activate a wider area in the vicinity of the axon compared with most other types of neurons, which release their neurotransmitters in a more focused and localized area at the distal synaptic terminal. On the basis of their morphology, three main types of enteric neurons exist: Dogiel type I, II, and III (Figure 27-8). These classifications are named for Alexander Dogiel, the histologist who initially described them. Dogiel type I neurons have small, irregular cell bodies with multiple short dendrites. Dogiel type II neurons have large, oval-shaped cell bodies with one or two long dendrites. Dogiel type III neurons have large cell bodies with different shapes and multiple dendrites.
Regulation of the Gastrointestinal Functions
The Gastrointestinal Tract, or Gut, Supplies the Body with Nutrients, Electrolytes, and Water by Performing Five Functions: Motility, Secretion, Digestion, Absorption, and Storage
Intrinsic and Extrinsic Control Systems Regulate Various Functions of the Gut
The Intrinsic Neuronal Control System of the Gastrointestinal Tract Is the Enteric Nervous System
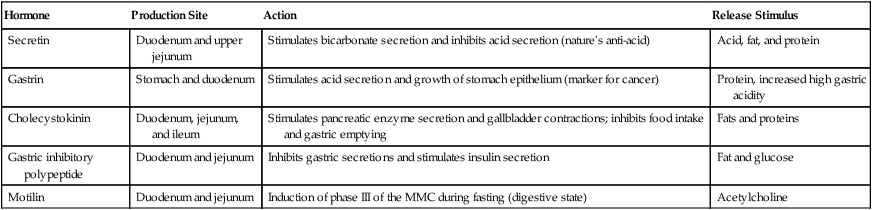
Hormone
Production Site
Action
Release Stimulus
Secretin
Duodenum and upper jejunum
Stimulates bicarbonate secretion and inhibits acid secretion (nature’s anti-acid)
Acid, fat, and protein
Gastrin
Stomach and duodenum
Stimulates acid secretion and growth of stomach epithelium (marker for cancer)
Protein, increased high gastric acidity
Cholecystokinin
Duodenum, jejunum, and ileum
Stimulates pancreatic enzyme secretion and gallbladder contractions; inhibits food intake and gastric emptying
Fats and proteins
Gastric inhibitory polypeptide
Duodenum and jejunum
Inhibits gastric secretions and stimulates insulin secretion
Fat and glucose
Motilin
Duodenum and jejunum
Induction of phase III of the MMC during fasting (digestive state)
Acetylcholine
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Regulation of the Gastrointestinal Functions
Only gold members can continue reading. Log In or Register to continue