Ashlee E. Watts
Regenerative Medicine in Orthopedics
Muscle, tendon, cartilage, and bone are efficiently and appropriately built during embryonic development. This is particularly manifested by the fact that injury to fetal tendon will result in complete healing and a fully functional structure that cannot be distinguished from uninjured tissue. Unfortunately, healing of musculoskeletal tissues in the postnatal animal is not as efficient or precise. Scar tissue, with alterations in cellular content and matrix components, leads to suboptimal performance of healed tissues. This is important in tendon, ligament, and cartilage healing in the horse. Inefficient healing is especially problematic in the horse with bone fracture because of the immediate need for weight bearing and the susceptibility of implants to fatigue failure.
Regenerative medicine is the method of harnessing natural healing processes to improve on various aspects of tissue repair to achieve a more functional healed tissue. The holy grail of regenerative medicine would be to recapitulate fetal development, resulting in healed tissues that cannot be distinguished from uninjured tissue. Although to date this has not been achieved in musculoskeletal tissues, the potential for substantially improving outcomes with the use of regenerative techniques is considerable. Consequently, there has been much activity in research and widespread clinical use of regenerative therapies for equine orthopedic applications. Some of the tools for regenerative medicine in orthopedics include stem cells, platelet-rich plasma, autologous conditioned serum, growth factors, and gene therapy. Regenerative therapies can be applied by intralesional, perilesional, intraarticular, or intravenous injections.
Stem Cells
Definitions
Stem cells, unlike their somatic cell counterpart, are self-renewing, highly proliferative, and capable of multilineage differentiation. The ultimate stem cell is made at conception. After fertilization, the zygote consists of totipotent stem cells that are able to form all three germ layers as well as placental tissue. After the zygote becomes a preimplantation blastocyst, the inner cell mass consists of pluripotent stem cells that will give rise to all three germ layers—ectoderm, mesoderm, and endoderm—and can no longer form placental tissues. At that stage, the stem cells are embryonic. After day 8, the cells become either somatic cells (terminally differentiated) or stem cells committed to a specific lineage (multipotent). After that point, the stem cells are considered adult derived despite their presence in fetal tissues. Local niches of lineage-committed multipotent stem cells remain in adult tissue throughout life for normal tissue remodeling and repair. With increasing age, the number, expansion potential, differentiation potential, and so-called potency of stem cells decline; therefore there is increasing interest in allogeneic embryonic and fetus-derived stem cells as well as banking of autologous stem cells from postnatal samples.
The initial enthusiasm for stem cells in regenerative medicine was related to the capacity for tissue-specific differentiation, in that stem cells implanted in a cartilage lesion would engraft, become chondrocytes, and produce cartilage matrix. As both scientific and clinical data accumulate, it appears that the effects of stem cell therapy may also be, largely or in part, a result of local production of bioactive molecules and immune modulation rather than tissue-specific differentiation and long-term engraftment of the implanted cells. What treatment effects stem cells actually impart is an important question. The answers will likely change what conditions are treated with stem cells and by which stem cell source, when the cells are applied and by which route, how often they are administered, and the number of cells used. To answer these questions, additional clinical and experimental studies are needed.
Because of the difficulty in isolation, expansion, and cryopreservation of equine embryonic stem cells, they have not been investigated in the horse for regenerative medicine and will not be discussed in this chapter. In contrast, adult-derived stem cells (nonembryonic) are generally considered to be safe and to carry little risk for tumor formation, are easy to isolate and expand, and have been used extensively in the horse. This chapter will focus on adult-derived stem cells. Modifications to these classifications of stem cells (embryonic and adult derived) are also being investigated and will be briefly discussed. One modification is a fetus-derived stem cell that has been manipulated in vitro to act more like an embryonic stem cell. One such product has been developed and tested in the horse, but commercial availability is pending U.S. Food and Drug Administration (FDA) approval. An important benefit of this type of stem cell is its immediate availability as an off-the-shelf product and its increased potency because of its pluripotent-like (embryonic-like) state. Another modification is the induced pluripotent stem (iPS) cell, in which in vitro manipulations are applied to adult somatic cells, such as skin fibroblasts, to dedifferentiate them and induce a stem cell–like state. The iPS cell is currently being investigated by several equine research groups.
Adult-derived mesenchymal stem cells (MSCs) are considered an excellent stem cell source for musculoskeletal regenerative therapies because they are readily available from several tissues, allow for use of autologous cells as well as allogeneic cells because of immune tolerance to non-self MSCs, and are of mesodermal lineage and thus able to differentiate into cartilage, tendon, and bone. The immune-privileged status of MSCs may be in part a result of their lack of expression of major histocompatibility complex class II proteins and most of the classic costimulatory molecules of antigen-presenting cells. Recent evidence also suggests that in addition to being immune privileged, MSCs are immune modulatory, through secretion of chemoattractants followed by regulation of immune cell (T and B cells) activation. Finally, MSCs may also be antiinflammatory through inhibition of interferon-γ and tumor necrosis factor-α and stimulation of metalloproteinase inhibitors and antiinflammatory interleukins, such as interleukin-10. The most exciting element of the MSC is an exquisite responsiveness to their microenvironment, in that the cells behave according to the environment in which they are placed. In this manner, MSCs would respond appropriately to the degree of disease and modulate the local environment in favor of some combination of reduced inflammation, reduced apoptosis, and enhanced matrix synthesis of endogenous progenitors and tissue-specific cells.
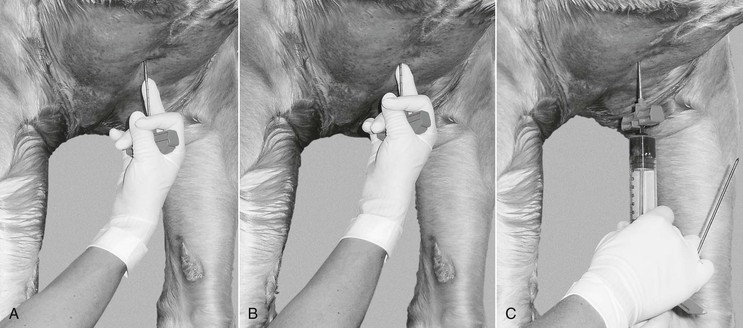
Because of their broad overlap with other cell populations, MSCs cannot yet be sorted accurately by cell surface markers. For that reason, many laboratories select and isolate MSCs by expanding the tissue culture plastic adherent population of colony-forming cells. This translates to a culture period of 2 to 3 weeks in vitro to isolate and expand MSCs from clinical samples for autogenous therapy. In the horse, MSCs have been isolated from bone marrow (Figures 25-1 and 25-2), adipose tissue (Figure 25-3), tendon, muscle, umbilical cord blood and tissue, gingiva and periodontal ligament, amniotic fluid, and blood. These tissue sources vary in ease of harvest, expansion potential, and differentiation capacity. Several academic and commercial laboratories provide for the isolation, expansion, and cryopreservation of stem cells from several different tissue sources, namely bone marrow, fat, and umbilical cord or blood. Directions for collection and shipping procedures are available from each laboratory. To date, bone marrow–derived MSCs from both the horse and human have been the most thoroughly studied and have the most evidence for ability to undergo chondrogenesis, tenogenesis, and osteogenesis and contribute to cartilage, tendon, and bone repair as well as to modulate inflammation and soft tissue repair within the joint.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


