The first portal is made at the dorsal margin of the internal abdominal oblique muscle (mid tuber coxae level) midway between the last rib and the tuber coxae. After a 1.5-cm stab incision is made, a 10-mm-diameter, 20-cm-long trocar-cannula unit with conical blunt obturator (Optomed Endoscopy, Courtaboeuf Cedex, France) is inserted into the abdomen slightly angled to the opposite stifle until perforation of the peritoneum is achieved. Aspiration of room air in the abdomen can often be heard because of the negative pressure normally present within the abdomen. Upon trocar removal, a 10-mm, 58-cm rigid 0° or 30° angled laparoscope is inserted through the cannula to check for proper intra-abdominal placement before CO2 insufflation is started. The abdomen is then insufflated with CO2 (6–8 L/min) with an intra-abdominal pressure cutoff level of 12 mmHg. The laparoscopic portal between the 17th and 18th ribs ±5 cm ventral to the ventral border of the tuber coxae is then made under direct visualization. This avoids accidental injury or perforation of the spleen. Entrance in the pleural space does not seem to be a problem when placing trocars between the 17th and 18th ribs. The laparoscope is then switched from the paralumbar position to the intercostal position and the ipsilateral vaginal ring is visualized. The small intestine, small colon, or bladder covering the caudal aspect of the vaginal ring are pushed aside using a 10-mm-diameter Babcock forceps through the proximal instrument portal. A second more distal and caudal instrument portal is made for the 20-cm and 12-mm-diameter laparoscopic trocar-cannula unit, at the level of the vaginal ring as caudal as possible and proximal to the flank fold (Figure 14.1A,B). Through this portal, the 12-mm-diameter Endo Hernia 65° stapler will be introduced. This Endo Hernia stapler has a maximal working length of only ±30 cm. It is very important to position this portal as caudal as possible to be able to reach the abdominal wall caudal to the vaginal ring. After visualization of the vaginal ring, mesorchium, vas deferens, and peritoneal wall, the borders of the intended peritoneal flap are identified (Figure 14.2). Mepivacaine hydrochloride (2%, 30 mL) is injected subperitoneally along the intended borders of the peritoneal flap using a laparoscopic injection needle introduced through the proximal instrument portal. Good local subperitoneal anesthesia is important to reduce movement during dissection.
Figure 14.2 Diagram (yellow lines) illustrating the borders of the peritoneal flap in the left inguinal region. The peritoneal flap has an inverted U shape and averages 10 cm in height to 6 cm in width. The blue arrows (1–3) illustrate the cutting directions. B, bladder; in, instrument; V, vaginal ring; M, mesorchium.
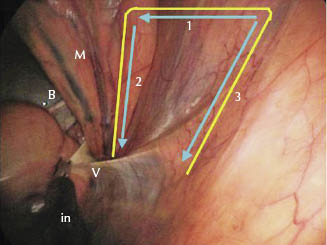
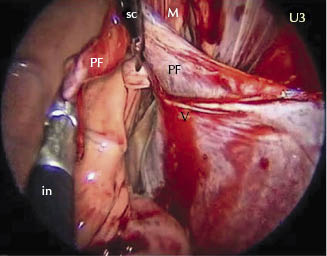
The peritoneal flap has an inverted U shape with the base oriented ventrally and averages 10 cm in height to 6 cm in width (Figure 14.2). The caudal half of the flap is located at the level of the cranial third of the vaginal ring, with the cranial half of the flap extending 2–3 cm cranial to the vaginal ring. The injection needle is removed and 5-mm laparoscopic scissors is introduced through the dorsal instrument portal. A ±6-cm horizontal incision is made in a cranial to caudal direction in the peritoneum approximately 10 cm proximal to the vaginal ring. The caudal vertical border of the flap is made by creating a vertical incision in the peritoneum covering the cranial part of the mesorchium and ending at the level of the vaginal ring. A 5-mm curved laparoscopic grasping forceps is then introduced through the distal instrument portal in order to grasp the caudal corner of the horizontal portion of the peritoneal flap, and the cranial vertical border of the flap is made using laparoscopic scissors, ending approximately 3–4 cm cranial and marginally distal to the level of the vaginal ring. The U-shaped peritoneal flap is at this point still attached to the subperitoneal fat and underlying abdominal muscle. The flap is now dissected free from the underlying internal abdominal oblique muscle using 5-mm laparoscopic scissors, taking care not to perforate the flap (Figure 14.3). Subperitoneal fat is left attached to the flap and dissection is carried out close to the abdominal muscles and to such an extent that a tension-free 180° rotation of the flap can be achieved. The flap should be large enough to completely cover the caudal portion of the vaginal ring (Figure 14.4) without tension. Major hemorrhage during dissection of the flap is unusual and can be avoided by careful dissection and coagulating larger blood vessels as needed.
Figure 14.3 Dissecting the peritoneal flap (x) from the underlying muscles in the left inguinal region, taking care not to perforate the flap and leaving the subperitoneal fat attached to the flap. Note how flap shrinks and how the underlying internal abdominal oblique muscle is exposed. in, instrument; SC, scissors; M, mesorchium; PF, peritoneal flap; F, fat; IOM, internal abdominal oblique muscle; X, borders of the peritoneal flap.
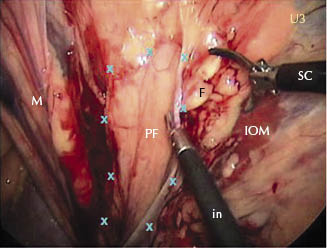
Figure 14.4 Peritoneal flap after dissection in the left inguinal region, ready for use. The peritoneal flap should be made large enough to allow a 180° tension-free rotation. The flap will now be inverted caudally to cover the entire vaginal ring. in, instrument; SC, scissors; M, mesorchium; PF, peritoneal flap; V, vaginal ring.
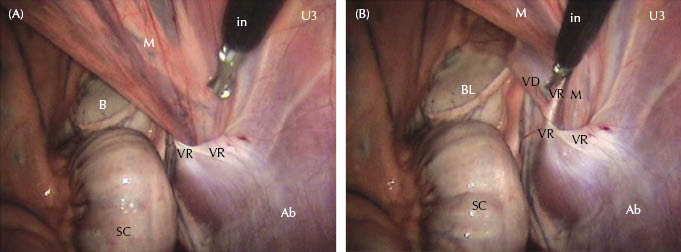
The 5-mm curved laparoscopic grasping forceps is then introduced through the dorsal instrument portal and the peritoneal flap is inverted caudally over the vaginal ring, making sure that the flap contains both mesorchium and vas deferens and covers the entire vaginal ring (Figure 14.5A,B). A 12-mm 30-cm-long Endo Hernia roticulator (Endo Universal 65°, Covidien) containing ten 4.8-mm stainless steel staples is introduced through the more ventral and caudal instrument portal, and the tip is rotated to its maximum 65° toward the flap. The caudal part of the flap is secured to the peritoneum caudal to the vaginal ring with two staples (Figure 14.5A,B). Pushing the mesorchium against the body wall is essential for proper visualization and staple placement when covering and closing the caudal aspect of the vaginal ring (Figure 14.6A,B).
Figure 14.5 (A) Attaching the peritoneal flap to the abdominal wall caudal to the left vaginal ring. Note the grasping forceps (in) pulling the flap caudal, covering the entire vaginal ring containing both the mesorchium and the vas deferens. The Endo Hernia stapler is flexed to its maximum 65° and readied to secure the tip of the flap to the abdominal wall caudal to the vaginal ring. The flap still needs to be stretched distally to cover the cranial and mid part of the vaginal ring. Note the large piece of fat tissue that was dissected free from the abdominal wall together with the flap. This can be removed or tucked in underneath the flap before stapling the mid and cranial part of the peritoneal flap. in, instrument; S, Endo Hernia stapler; M, mesorchium; PF, peritoneal flap; VD, vas deferens; LB, lateral ligament bladder; VR, cranial part of the vaginal ring; Ab, abdominal wall; F, fat. (B) Attaching the peritoneal flap to the abdominal wall caudal to the left vaginal ring. The peritoneal flap contains both the mesorchium and the vas deferens. Covering the caudal aspect of the vaginal ring is paramount to prevent reherniation in the future. S, Endo Hernia stapler; M, mesorchium; PF, peritoneal flap; LB, lateral ligament bladder; EV, branch of the epigastric vein; Ab, abdominal wall caudal to the vaginal ring.
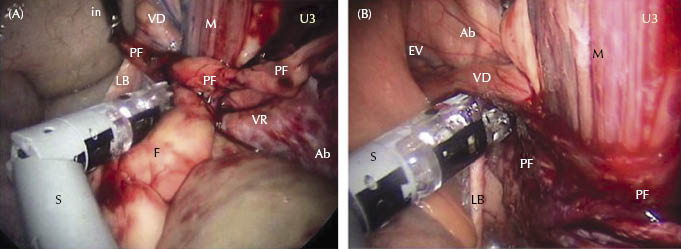
Figure 14.6 (A) Laparoscopic view of the left vaginal ring before pushing the mesorchium against the body wall. Only the cranial and mid part of the vaginal ring can be visualized. The vas deferens cannot be seen; it is hidden behind the mesorchium. in, instrument; M, mesorchium; B, bladder; VR, cranial and mid third of the vaginal ring; Ab, abdominal wall; SC, small colon/descending colon/colon tenue. (B) Laparoscopic view of the same left vaginal ring as in (A) but with the mesorchium pushed against the body wall. Note how the caudal aspect of the vaginal ring can be visualized together with the vas deferens. Pushing the mesorchium against the body wall is essential to expose the abdominal wall and to attach the peritoneal flap caudal to the vaginal ring. in, instrument; M, mesorchium; BL, bladder; VR, cranial, mid, and caudal third of the vaginal ring; Ab, abdominal wall; SC, small colon/descending colon/colon tenue; VD, vas deferens.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


